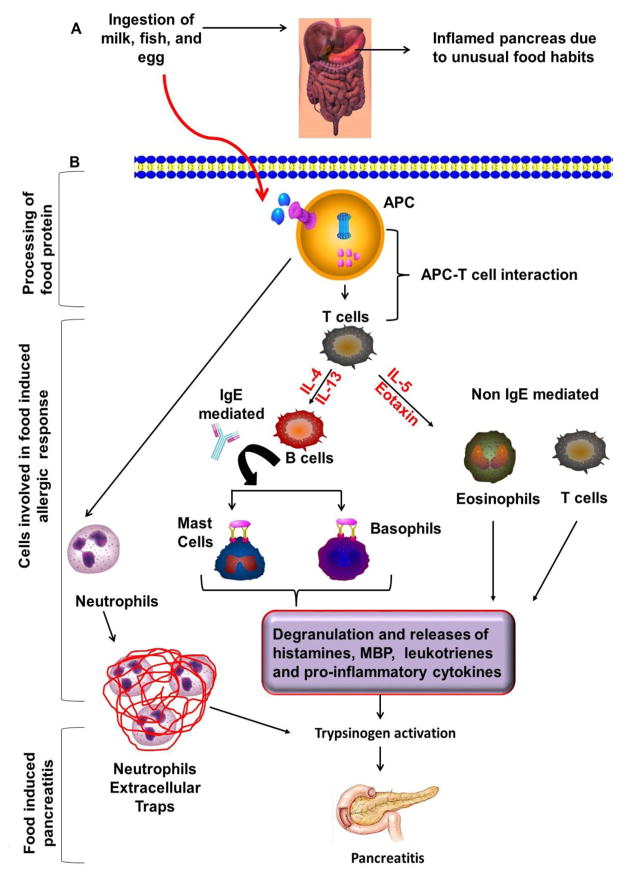
Figure 1. The possible operational mechanism in food allergen-induced acute pancreatitis.
Food allergens internalized and processed by antigen presenting cells (APCs) with the help of proteosomal complex and presented by major histocompatibility complex class-II (MHC-II) to the naive CD4+ T cells that differentiate into the Th2 cells in the presence of IL-4 and produce IL-5 and IL-13 that activate downstream allergic pathways and induces food allergen associated acute pancreatitis. The food allergen–induced allergic response in the pancreas may be IgE or non-IgE mediated. In IgE mediated response, Th2 cells secrete IL-4 and IL-13 that causes B cell activation and IgE class switching. IgE antibodies bind to FcεRI surface receptors present on mast cells and basophils that lead degranulation and release of several allergic mediators. These allergic mediators probably cause trypsinogen activation and development of pancreatitis. However, this hypothesis needs to be explored further for the designing treatment strategies. In contrast, the non-IgE mediated response may also occur that includes the role of IL-5 and eosinophil active chemokines eotaxins that recruit, activate and releases several inflammatory mediators and lead trypsinogen activation. Increased level of trypsin consecutively setup the episode of acute pancreatitis. In addition, neutrophils are forming neutrophil extracellular traps (NETs) of de-condensed DNA and histones, which is sufficient to induce trypsin activation to promote pancreatitis pathogenesis.