Abstract
Background
The complication of vein patch rupture is well described after carotid patch angioplasty; however, there is a paucity of data about the safety of vein patch closure in the setting of femoral endarterectomy.
Methods/results
From May 2012 to May 2015, 115 femoral endarterectomies with patch closure were performed. A patch rupture occurred in three cases (2.6%) with a mortality rate of 66% (2/3). In all cases the greater saphenous vein below the knee was used as patch material.
Discussion/conclusion
Vein patches, particularly from small calibre veins, should be excluded in femoral endarterectomy procedures as they pose a substantial risk of rupture.
Keywords: Angioplasty, Patch rupture, Femoral artery, Patch, Great saphenous vein
Highlights
-
•
Choice of patch material for endarterectomy procedures of the common femoral artery may be crucial.
-
•
Patch rupture after use of the greater saphenous vein occurs in 3% of cases.
-
•
A particular risk of rupture occurs after the use of below knee greater saphenous vein patches.
-
•
Patch rupture is associated with a high mortality rate.
Background
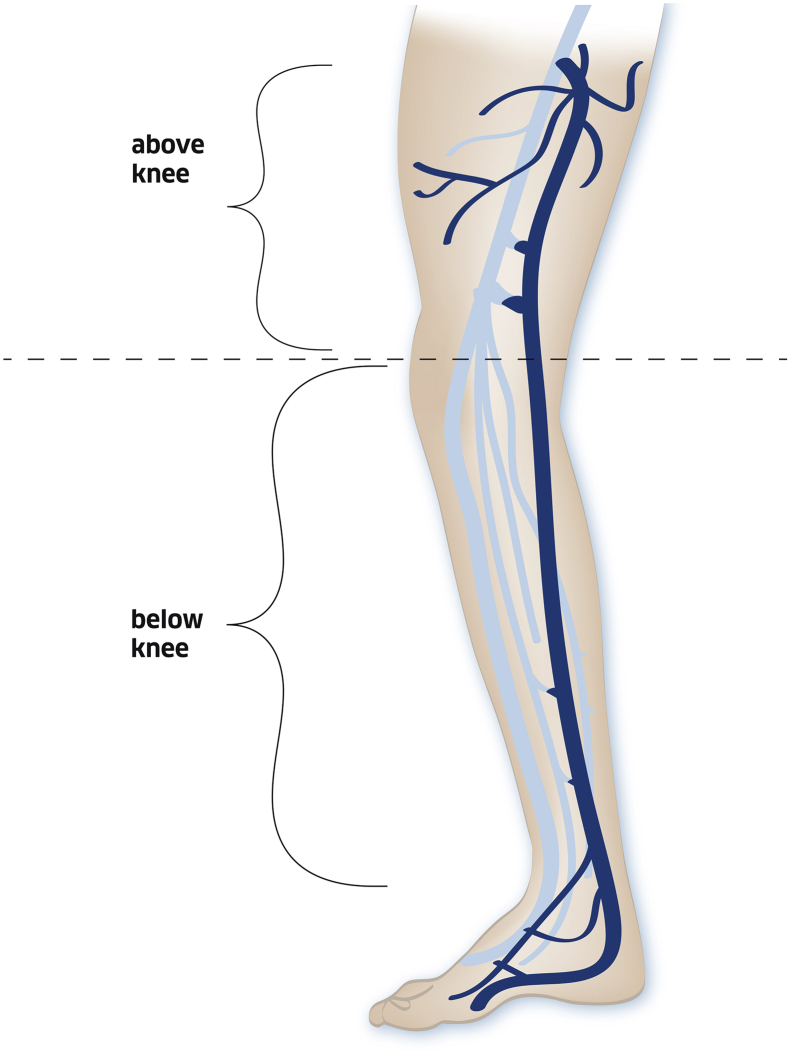
Femoral endarterectomy with patch angioplasty closure is the preferred surgical technique to treat an atherosclerotic stenotic lesion of the common femoral artery. Surgical site infection is the most relevant associated complication occurring in up to 9% of cases.1 The use of autologous vein patch material was a logical choice because of its known resistance to infection. For many years, an autologous greater saphenous vein (GSV) patch policy was pursued at the study hospital with a preference for use of the vein below the knee (Fig. 1) to spare the proximal part for potential future revascularisation procedures. The possibility of vein patch rupture after carotid endarterectomy is well described; however, there is a paucity of data regarding the safety of vein patches in the femoral position with a single report of two cases dating back to 1997.2 This case report describes a 3 year single centre experience and highlights the potential associated fatal risk of such procedures.
Figure 1.
Illustration of what was specified as greater saphenous vein below versus above the knee.
Methods/results
From May 2012 to May 2015, a total of 115 femoral endarterectomies with patch closure were performed in patients with a mean age of 73±7 years, with a 70% male predominance. In 76% (87 out of 115) and in 17% (20 out of 115), patients suffered from claudication and critical leg ischaemia respectively, while in the remaining eight patients, the surgical indication was for various other reasons, including acute limb ischaemia, inflow or outflow correction. The arterial lesion was a stenosis in 100 cases and an occlusion in 15 cases. The GSV was used in 88 cases; in the majority of cases it was the vein below the knee (N = 72), while in the remaining 16 cases it was the GSV above the knee (Fig. 1).
In patients with no adequate vein material, bovine pericardial patch material (N = 22) or synthetic patch material (N = 5) was used.
Vein patch rupture occurred in three cases (2.6%) yielding an incidence rate of 3.4% among those cases with vein patch closure (3 out of 88 cases). In all of these cases, the GSV below the knee was used as patch material. All of these ruptures occurred during the first 3 post-operative days, and in none of the cases was an associated infection assumed. The mortality rate was 66% (2 out of 3).
In case 1, the patient was found dead in her bed in the early morning. In case 2, the patient was transferred immediately to the operating theatre under manual compression of the bleeding surgical site, but emergency revision could not prevent the fatal outcome. In case 3, emergency surgical revision, during which the ruptured vein patch was replaced by a bovine pericardial patch, was successful. In all of the cases, a longitudinal rupture was identified in the centre of the patch.
Patch rupture following non-vein patch closure was not observed; a difference that does not reach statistical significance because of the small and unequal sample size with a low event rate.
Discussion
This short report demonstrates a 3.4% risk of early post-operative vein patch rupture after femoral endarterectomy using vein patch closure with a mortality rate of 66% (2 out of 3). This complication is well described after vein patch closure of carotid endarterectomy procedures with a rate of 0.1% to 4%, associated with a fatal outcome in 30%.3, 4, 5
Venous patch material has been used for many years, because of its specific favourable properties, including infection resistance, minimal suture hole bleeding, and less thrombogenic potential compared with synthetic patch material.6
In all ruptured cases, the below knee GSV was used as patch material. This is an experience which is well reflected in the carotid cases. A smaller calibre vein seems to be more vulnerable because of its lower rupture pressure. Archie and Green investigated this phenomenon in detail and they discourage using veins with a diameter below 3.5 mm.7
It was noted that the critical rupture time after carotid angioplasty was the first post-operative week, which is well in line with the present experience, as all cases ruptured within the initial 3 post-operative days.3, 8
All of the present cases demonstrated a longitudinal tear within the vein patch. Archie and Green suggested that the increased risk of rupture resulted from a change of arterial shape from circular to oval after patchplasty.7 The zone of a patch that is most likely to rupture is located where the radius of curvature is greatest and the circumferential wall stress is maximal, so the rupture was mainly longitudinal in the centre of the patch.7
The rupture pressure of the vein patch depends on the diameter of the donor vein and the new diameter of the patched femoral artery. It is accepted that larger veins have a higher rupture pressure and are less likely to disrupt. Clearly, there are some other factors such as vein wall thickness and wall structure that impact on vein patch stability.7, 9
Harvesting the GSV at the groin level, however, could result in higher local morbidity and would make a later use of the ipsilateral GSV for more extensive revascularisation procedures impossible.
Synthetic graft materials are alternative patch materials. They are easy to handle, but their biggest drawback is their lack of resistance to infection. In such situations, most synthetic patches have to be removed.10 This problem may be overcome by the use of pericardial patch material, which shares similar properties with autologous vein patch material, namely high biocompatibility, easy handling with improved suturability, less suture line bleeding, and also probable reduced rates of infection. Consequently, this material has even proved useful in infected scenarios.11
One drawback, however, is its higher incurred costs. It could be argued that vein patch harvesting would also increase the costs because of a likely increased operation duration. In the authors' routine, however, the vein was harvested simultaneously to the access to the groin vessels and thus it is unlikely that operation time was affected.
Since the last rupture, the authors' patch policy has been changed for femoral endarterectomy procedures, with bovine pericardial patches now used, that combine the most desired patch properties.12
This case series has particular strengths and limitations. The main strength of the report is the large number of endarterectomy procedures, which renders the reported incidence of vein patch ruptures very reliable. However, as this is a retrospective study, some relevant data were not available, including vein patch length and width. Furthermore, the ruptured patches were not sent for histological examination, which was a missed opportunity to assess the detailed characteristics of the vein patch tear and patch thickness.
Conclusion
Vein patches, particularly from small calibre veins, should be excluded in femoral endarterectomy procedures as they pose a non-negligible risk of rupture with a high mortality rate.
Conflict of interest
None.
Funding
None.
References
- 1.Siracuse J.J., Gill H.L., Schneider D.B., Graham A.R., Connolly P.H., Jones D.W. Assessing the perioperative safety of common femoral endarterectomy in the endovascular era. Vasc Endovasc Surg. 2014;48:27–33. doi: 10.1177/1538574413508827. [DOI] [PubMed] [Google Scholar]
- 2.Florenes T., Kroese A. Rupture of the vein patch: a serious complication of profundaplasty. Eur J Surg. 1992;158:621–622. [PubMed] [Google Scholar]
- 3.Tawes R.L., Jr., Treiman R.L. Vein patch rupture after carotid endarterectomy: a survey of the Western Vascular Society members. Ann Vasc Surg. 1991;5:71–73. doi: 10.1007/BF02021782. [DOI] [PubMed] [Google Scholar]
- 4.White S.A., Thompson M.M., Gaunt M.E., Boyle J.R., Budd J.S., Naylor A.R. Vein patch rupture after carotid endarterectomy. Eur J Vasc Endovasc Surg. 1995;9:351–352. doi: 10.1016/s1078-5884(05)80144-3. [DOI] [PubMed] [Google Scholar]
- 5.Yamamoto Y., Piepgras D.G., Marsh W.R., Meyer F.B. Complications resulting from saphenous vein patch graft after carotid endarterectomy. Neurosurgery. 1996;39:670–675. doi: 10.1097/00006123-199610000-00003. discussion 5–6. [DOI] [PubMed] [Google Scholar]
- 6.Ren S., Li X., Wen J., Zhang W., Liu P. Systematic review of randomized controlled trials of different types of patch materials during carotid endarterectomy. PLoS One. 2013;8 doi: 10.1371/journal.pone.0055050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Archie J.P., Jr., Green J.J., Jr. Saphenous vein rupture pressure, rupture stress, and carotid endarterectomy vein patch reconstruction. Surgery. 1990;107:389–396. [PubMed] [Google Scholar]
- 8.Riles T.S., Lamparello P.J., Giangola G., Imparato A.M. Rupture of the vein patch: a rare complication of carotid endarterectomy. Surgery. 1990;107:10–12. [PubMed] [Google Scholar]
- 9.Archie J.P. Carotid endarterectomy saphenous vein patch rupture revisited: selective use on the basis of vein diameter. J Vasc Surg. 1996;24:346–351. doi: 10.1016/s0741-5214(96)70190-8. discussion 51–2. [DOI] [PubMed] [Google Scholar]
- 10.Mertens R.A., O'Hara P.J., Hertzer N.R., Krajewski L.P., Beven E.G. Surgical management of infrainguinal arterial prosthetic graft infections: review of a thirty-five-year experience. J Vasc Surg. 1995;21:782–790. doi: 10.1016/s0741-5214(05)80009-6. discussion 90–1. [DOI] [PubMed] [Google Scholar]
- 11.McMillan W.D., Leville C.D., Hile C.N. Bovine pericardial patch repair in infected fields. J Vasc Surg. 2012;55:1712–1715. doi: 10.1016/j.jvs.2011.11.139. [DOI] [PubMed] [Google Scholar]
- 12.Ho K.J., Nguyen L.L., Menard M.T. Intermediate-term outcome of carotid endarterectomy with bovine pericardial patch closure compared with Dacron patch and primary closure. J Vasc Surg. 2012;55:708–714. doi: 10.1016/j.jvs.2011.10.007. [DOI] [PubMed] [Google Scholar]