Figure 1.
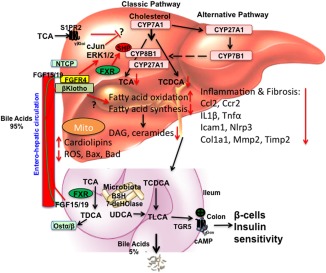
Targeting to bile acid and lipid metabolism in NASH treatment. Bile acids are synthesized from cholesterol in hepatocytes. Cyp7a1 is the first and rate‐limiting enzyme in the classic bile acid synthesis pathway to synthesize CA and CDCA. Cyp8b1 is required for synthesis of CA. Cyp27a1 is involved in steroid side‐chain oxidation. The alternative pathway is initiated by Cyp27a1, followed by Cyp7b1. Bile acids are conjugated to amino acids glycine and taurine for secretion into bile. In mice, CDCA is converted to α‐ and β‐muricholic acids. CDCA activates FXR to induce a negative factor, SHP, which inhibits Cyp7a1 and Cyp8b1 gene transcription. Bile acids are stored in the gallbladder and secreted into the gastrointestinal tract for nutrient absorption. In the intestine, conjugated bile acids are deconjugated by bacterial BSH and bacterial 7‐dehydroxylase activities convert CA and CDCA to DCA and LCA, respectively. In the ileum, FXR induces FGF15 (or human FGF19). Bile acids and FGF15/FGF19 are secreted into portal blood for circulation to the liver. In hepatocytes, FGF15 and FGF19 activate the FGF receptor 4/β‐Klotho complex to activate cJun/ERK1/2 of the MAPK pathway to inhibit Cyp7a1 gene transcription. Conjugated bile acid‐activated S1PR2 may also be involved in inhibiting Cyp7a1. In NAFLD and NASH, hepatic bile acid and lipid metabolisms are impaired to accumulate toxic bile acids and lipids along with cholestatic liver injury. Ceramides and diacylglycerols have been linked to insulin resistance in diabetes. FGF19 and M70 inhibit bile acid synthesis and reduce bile acid hydrophobicity. FGF19 and M70 stimulate fatty acid oxidation and inhibit fatty acid synthesis to reduce lipogenesis, ceramides, and diacylglycerol and to increase unoxidized‐cardiolipins in mitochondria; reduced ROS reduces inflammatory cytokines and chemokines (CCl2, Ccr2, IL‐1β, Tnf‐α), fibrosis markers (Col1a1, Timp2), and apoptosis markers (Bax, Bad). In colon, activation of TGR5 stimulates cAMP and secretion of GLP‐1 to improve insulin sensitivity. Abbreviations: BSH, bile salt hydrolase; CA, cholic acid; cAMP, cyclic adenosine monophosphate; CCl2, (C‐C motif) ligand 2; Ccr2, (C‐C motif) receptor 2; CDCA, chenodeoxycholic acid; Col1a1, collagen, type I, alpha 1; Cyp27a1, mitochondria sterol 27‐hydroxylase; Cyp7a1, cholesterol 7α‐hydroxylase; Cyp7b1, oxysterol 7α‐hydroxylase; Cyp8b1, sterol 12α‐hydroxylase; DAG, dystroglycan; DCA, deoxycholic acid; ERK, extracellular signal‐regulated kinase; GLP‐1, glucagon‐like peptide‐1; Icam1, intercellular cell adhesion molecule 1; IL‐1β, interleukin‐1β; LCA, lithocholic acid; MAPK, mitogen‐activated protein kinase; Mmp2, matrix metalloproteinase 2; Nlrp3, nucleotide‐binding domain and leucine‐rich repeat containing protein 3; NTCP, sodium‐taurocholate cotransporting polypeptide; Ostα/β, organic solute transporter alpha/beta; ROS, reactive oxygen species; S1PR2, sphingosine‐1‐phosphate receptor 2; SHP, small heterodimer partner; TCA, trichloroacetic acid; TCDCA, taurochenodeoxycholic acid; TDCA, taurodeoxycholic acid; TGR5, G protein‐coupled bile acid receptor 1; Timp2, tissue inhibitor of metalloproteinase 2; TLCA, taurolithocholic acid; Tnf‐α, tumor necrosis factor alpha; UDCA, ursodeoxycholic acid.
