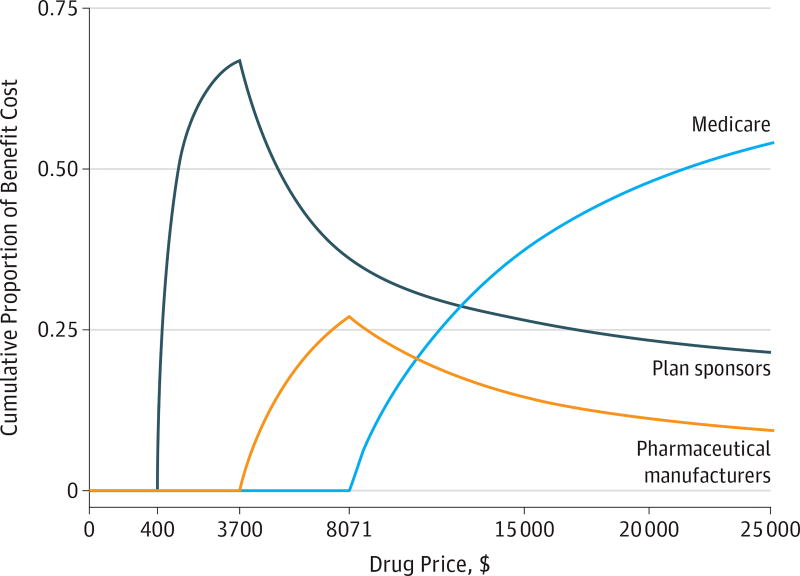
Figure 3. Cumulative Share of Drug Payments by Payer as Drug Prices Increase.
As a drug’s price increases under the 2017 Part D standard benefit, the cumulative share of Part D spending shifts from plan sponsors and pharmaceutical manufacturers to Medicare. The standard 2017 benefit has a $400 deductible (where the patient pays 100%), and then drug costs are shared between the patient (who pays 25%) and the payer (which pays 75%) during the initial coverage phase until total drug spending reaches $3700. After this limit, the patient, payer, and manufacturer pay 40%, 10%, and 50%, respectively, of branded drug prices during the coverage gap phase (the “donut hole”) until total drug spending reaches $8071. After this point, the patient enters the catastrophic phase in which Medicare bears 80% of costs, plans 15%, and patients 5%, with no upper limit on patient spending.