Abstract
A newly designed, low-cost, disposable inhalable aerosol sampler was developed to assess workers personal exposure to inhalable particles. This sampler was originally designed to operate at 10 L/min to increase sample mass and, therefore, improve analytical detection limits for filter-based methods. Computational fluid dynamics modeling revealed that sampler performance (relative to aerosol inhalability criteria) would not differ substantially at sampler flows of 2 and 10 L/min. With this in mind, the newly designed inhalable aerosol sampler was tested in a wind tunnel, simultaneously, at flows of 2 and 10 L/min flow. A mannequin was equipped with 6 sampler/pump assemblies (three pumps operated at 2 L/min and three pumps at 10 L/min) inside a wind tunnel, operated at 0.2 m/s, which has been shown to be a typical indoor workplace wind speed. In separate tests, four different particle sizes were injected to determine if the sampler’s performance with the new 10 L/min flow rate significantly differed to that at 2 L/min. A comparison between inhalable mass concentrations using a Wilcoxon signed rank test found no significant difference in the concentration of particles sampled at 10 and 2 L/min for all particle sizes tested. Our results suggest that this new aerosol sampler is a versatile tool that can improve exposure assessment capabilities for the practicing industrial hygienist by improving the limit of detection and allowing for shorting sampling times.
Keywords: Aerosols, exposure assessment, high-flow, inhalable sampler, wind tunnel
Introduction
Airborne particles that enter the body through the nose and/or mouth during breathing are called “inhalable particles/dusts,” or the “inhalable aerosol fraction.”[1,21] This fraction is defined for particle sizes with aerodynamic diameters smaller than 100 μm.[1,21] The inhalable fraction also encompasses the respirable fraction (the mass fraction of inhaled particles penetrating beyond the larynx) and the thoracic fraction (the mass fraction of inhaled particles penetrating to the unciliated airways).[21] Exposure to these types of inhalable dust is commonplace in many workplace environments across the U.S. Examples of these types of dusts include mineral dusts (coal and cement dusts from mining, refining, and construction),[5,9,22] metallic dusts (lead, cadmium, and nickel dusts from manufacturing and machining),[6–8,22] chemical dusts (pesticides from farming),[22] organic and vegetable dusts (grain, flour, wood, cotton dusts from farming and forestry),[2–4,22] and biohazards (molds and spores).[22] The Institute of Occupational Medicine (IOM) personal inhalable sampler, the Button inhalable sampler, and 37-mm closed-face cassette (CFC) “total” dust sampler are some of the commonly used air samplers in the U.S. These samplers have all been used to assess the worker’s personal exposure to particles in a workplace environment.[10,11]
The criterion that has been established and adopted by the American Conference of Governmental Industrial Hygienists (ACGIH) for these inhalable samplers is known as the inhalable particulate matter (IPM) criterion. The IOM sampler—perhaps the best known of all the inhalable samplers—has a sampling efficiency that is considered the field standard for collecting inhalable dust.[12] The IOM was designed to achieve sampling efficiencies that meet the IPM criterion, which is used to assess exposure to those materials that are hazardous when deposited anywhere in the respiratory tract.[14] The Button inhalable aerosol sampler was also found to closely match the IPM under specific operating conditions.[20] However, both the Button and IOM samplers can be costly, retailing for $249.00 and $85.00–$269.00, respectively, which may be cost prohibitive for some health and safety professionals.[10] The CFC costs around $1.00, which makes it a significantly more affordable option. However, the CFC under-samples particles larger than 30 μm in aerodynamic diameter [13] and therefore should not be assumed to estimate inhalable aerosol exposures, particularly when the particle size distribution is known to be large (e.g., wood dust). The complexity of the IOM and Button samplers may also play a factor in why they have not been more widely adopted by health and safety professionals, e.g., the IOM has seven components and can be challenging to assemble and maintain.[10] It should also be noted that the Button has difficulty sampling droplet aerosol.[23] Due to their expense, the IOM samplers are not disposable and must be shipped back to the user after laboratory analysis. For the Button sampler, only the filter goes to and from the lab, requiring the industrial hygienist to handle the filter. This is a major drawback due to the high likelihood of contamination during handling.
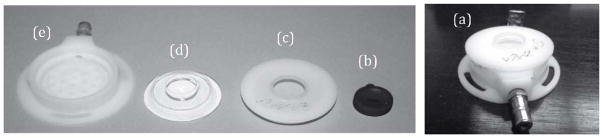
A new, low-cost, disposable inhalable aerosol sampler (Figure 1) was designed by L’Orange et al. [10] to assess workers personal exposure to inhalable particles in a workplace environment. The newly designed disposable inhalable aerosol sampler was constructed to be a less expensive option, as well as more user-friendly than other commonly used samplers. Consisting of only three components, the new sampler may be a more feasible option. One of the components is a lightweight internal capsule with a 15-mm inlet bonded to a 37-mm sampling filter. The capsule allows for the collection of particles deposited on the internal walls of the sampler, similar to the internal cassette of the IOM.[10] Due to the low cost and simple nature of the capsule, after one use it can be discarded, similar to the CFC.
Figure 1.
The newly designed sampler, disassembled: (a) housing, (b) capsule and filter, (c) inlet, and (d) inlet cover. To assemble: capsule/filter is placed in housing, then inlet placed on top, followed by the inlet cover (e). Photo courtesy of Tracy M. Rees.
The new prototype sampler was initially tested at a flow rate of 2 L/min to collect inhalable particulate matter with the same efficiency as the IPM convention and other existing technologies (e.g., IOM sampler, Button sampler). It was originally designed, however, to operate at 10 L/min to increase sample mass and, therefore, improve analytical detection limits for filter-based methods. A previous study of the new sampler by L’Orange et al.[10] showed that it closely matched the low velocity inhalability criterion for particles ranging from 9.5–60.1 μm and matched the efficiency and accuracy of the IOM sampler at all particle sizes tested. These results indicate the new sampler is an efficient—and also less expensive, disposable, and simpler—alternative for assessing exposure to inhalable aerosol hazards in the workplace within this particle size range.
Cheng et al.[15] used the IOM sampler to collect aerosols in an environment with low aerosol concentrations. They found that when the IOM sampler was operating at 2 L/min, it could not always collect enough material to surpass the limit of detection for chemical analysis.[15] Anthony et al. [17] reported that computerized simulations of the new sampler operating at a flow rate of 10 L/min also achieved the targeted sampler efficiency. Zhou et al. [16] researched the effect of increasing the flow rate of an IOM sampler from 2 L/min to 10.6 L/min in order to evaluate if the performance of the sampler was similar at both flow rates. Using a wind tunnel, they evaluated the sampling efficiency of the IOM sampler as it pertained to particle size, wind speed, and wind direction.[16] Zhou and his colleagues concluded that at a low wind speed of 0.56 m/s, the IOM could maintain its original collection capabilities while operated at a higher flow rate. They found that the direction-averaged sampling efficiencies for both flow rates had a similar trend, but there was a slightly lower efficiency for the 10.6 L/min sampling flow rate as compared with that of the 2 L/min flow rate.
Given these prior studies, it was decided that the newly designed sampler should be tested at multiple flow rates, 2 L/min and 10 L/min. Some existing personal sampling pumps have the ability to sample with a flow rate of up to 15 L/min (e.g., Leland Legacy or the Gillian 12), so such a comparison is now possible. Increasing the sampler flow rate would also increase the rate of particle mass depositing on the filter, thus increasing the likelihood of surpassing the analytical limit of detection in lower concentration environments. Lowering the detection limit assists in the quantification of low concentration exposures to aid in risk assessments. Also, the risk of not having enough material on the filter for lab analysis would be reduced. Increasing the flow rate could also require less sampling time while still enabling collection of the same sample volume (i.e., task-based exposure assessment). If the new sampler can operate at 10 L/min with no substantial difference in sampling efficiency than at 2 L/min, it could provide improved exposure assessment methods for the practicing industrial hygienist.
Methods
The newly designed inhalable aerosol samplers were tested, side-by-side, at 2 L/min flow rate and at 10 L/min flow rate. A mannequin was equipped with six pump/sampler assemblies (3 pumps at 2 L/min and 3 pumps at 10 L/min) inside a wind tunnel into which particles were injected in order to determine if the sampler’s performance with the higher flow rate significantly differed from that of a more typical flow rate.
Capsule/filter assembly
The capsule (shown in Figure 1b) is made of polyethylene (i.e., polyethene). The outer ring of the capsule is a 2-mm flange that is chemically bonded to the sampling filter (for this study, a 37-mm glass fiber) with toluene. Assembly was simple and straightforward: filter media was placed in a typical 37-mm plastic filter cassette (CFC) on top of a support pad (i.e., of the type typically used for “total” dust sampling). A cotton swab was dipped into a small amount of toluene, and then the filter media was wetted on the outside edge, ensuring that the wet area was larger than the contact area (flange) of the capsule. Using tweezers, the capsule was placed in the cassette with the media and, using the middle section of a CFC sampler, pressure was applied to ensure a good seal.
In this study, we wanted to be certain that the excess toluene had evaporated and the assembly was gravimetrically stable, therefore the assembly was conditioned for at least 24 hr prior to use. To test for gravimetric stability, several assemblies were weighed over the course of five days to verify there was no change in weight. The capsule-filter assembly weight only changed slightly (range: ±0.02 mg) during that time. Gravimetric stability of the capsule-filter assembly is important for sampler practicality and gravimetric limit of detection,[10] and a change of 0.02 mg is within acceptable limits. Even better gravimetric stability can also be achieve by using a 24-hr heating cycle followed by a 24-hr equilibration.[10] A total of 110 capsules were constructed for testing and all capsules were conditioned in the lab for over one week to achieve gravimetric stability.
Wind tunnel
Sampling efficiencies of the new sampler were evaluated at the Rocky Mountain Center for Occupational & Environmental Health (RMCOEH) Wind Tunnel Laboratory at the University of Utah in Salt Lake City, UT (see Figure 2). Sampler efficiency was tested with samplers attached to a mannequin torso—of human dimensions—in a low velocity wind tunnel. The mannequin was rotating at two rotations per minute to enable orientation-averaged sampling. Particles were injected upstream of the mannequin using a TOPAS aerosol generator (Solid Aerosol Generator 410, Dresden, Germany) connected to an outlet tube.[18] To ensure a uniform distribution of airborne particles, the outlet tube oscillated across a 45˚ arc while it traversed the wind tunnel cross section.[18] A wind speed of 0.2 m/s was used, as this has been shown to be a typical indoor work place wind speed.[19] Air speed in the wind tunnel was calibrated with a digital manometer (MA204E, Modus Instruments Inc., Clinton, MA). This study followed the same mannequin setup, concentration uniformity, and wind tunnel setup as Schmees et al. [18] and a more detailed description can be found in that study. Electrostatic and agglomeration particle effects were not directly addressed.
Figure 2.
Wind tunnel with mannequin located at the Rocky Mountain Center of Occupational and Environmental Health. Schmees, D.K., Y.-H. Wu, and J.H. Vincent: Experimental methods to determine inhalability and personal sampler performance for aerosols in ultra-low windspeed environments. J. Environ. Monit. 10(2):1426.1436 (2008). Reproduced by permission of The Royal Society of Chemistry.
Four particle sizes that are in the inhalable size range were used for this study. The particles consisted of narrowly graded fused alumina powder (Duralum, Washington Mills, Niagara, NY) with mass median aerodynamic diameters of 32.7, 12.8, 9.5, and 4.9 μm (Duralum grit sizes of F500, F800, F1200, and F2400, respectively). These particle size distributions have nominal geometric standard deviations ranging from 1.19–1.38.[18]
Personal sampler
For each test, the mannequin was fitted with three samplers operating at 2 L/min using XR5000 pumps (SKC Inc., Eighty Four, PA) and three samplers at 10 L/min using Leland Legacy pumps (SKC Inc., Eighty Four, PA). The position of a given sampler type was randomized for each test. Due to the weight and logistical issues associated with six pumps on the mannequin, the pumps were placed in a backpack to ensure no drag as the mannequin rotated. All hoses were clipped to the torso of the mannequin so as to not interfere with the inlets of the samplers and all samplers were positioned so that the inlet faced outwards, i.e., with no upward or downward angle (see Figure 3).
Figure 3.
Mannequin equipped with six pump/sampler assemblies (three pumps at 2 L/min and three pumps at 10 L/min).
Isokinetic samplers were used to determine the reference air concentration for calculating the collection efficiency of the new sampler at each flow rate. These samplers consist of four parts: a 2-inch long metal inlet, outlet, sampling filter (25-mm glass fiber), and plastic o-ring. The o-ring is used to secure the sampling filter in place. For each test, two of these samplers were placed 0.75 m upstream of the mannequin along the central axis of the wind tunnel (i.e., in line with the mannequin/samplers) and offset vertically from each other by about 15 cm. Both samplers were set to operate at 0.55 L/min to match the wind tunnel air velocity (0.2 m/s), using XR5000 pumps (SKC Inc., Eighty Four, PA).
All XR5000 sample pumps were calibrated using a BIOS DryCal flow meter (DC-Lite) (Mesa Labs, Lakewood, CO). Leland Legacy pumps (SKC Inc., Eighty Four, PA) were calibrated using a BIOS DryCal Defender flow meter (Mesa Labs, Lakewood, CO). All pumps were calibrated before and after each test to ensure that sampling flow rates did not change more than ±5%, which would have invalidated that sample.
Test protocol
The order in which the particle sizes were tested was randomly selected. Each sampling session lasted 45 min, with one particle size injected for each test. This amount of time was sufficient to provide uniform concentration across the wind tunnel but prevented overloading of filters. One “field” blank (i.e., it traveled to and from the wind tunnel with the other samples) per test was also analyzed. The four particle sizes were tested four times each (16 tests) for 52 samples (3 samples per test × 4 particle sizes × 4 repeats; including blanks) at the two flow rates (104 samples total). Sampling filters were analyzed gravimetrically using a semi-microbalance (accuracy: ±0.012 mg) with high voltage neutralizer (Sartorius Cubis MSA, Sartorius Weighing Technology GmbH, Goettingen, Germany). All sampling media (capsule/filter assembly and isokinetic filter) were weighed prior to testing and then reweighed after the test. The isokinetic sampler’s inside walls, 2-in inlet, and plastic ring were rinsed with isopropyl alcohol to collect particles deposited on the walls, which were added to the isokinetic filter mass to determine the reference concentration.
Data analysis
All data analysis was performed with Microsoft Excel (Microsoft, Redmond, WA) and Stata 13.1 (StataCrop, College Station, TX). For each particle size, the mean and standard deviation were calculated for both flow rates (12 samples per particle size). A quantitative normality test (skewness and kurtosis) was performed in Stata, which indicated the data were not normally distributed. The result of the test showed that the data were not normally distributed. Non-normal distributed data required the use of a Wilcoxon signed-rank test (nonparametric paired test). The P-values were determined for each particle size to compare the means between the particle concentration of samplers run at the 2 L/min and the 10 L/min flow rate. The level of significance set for the test was 0.05. This had ~80% power to detect a 15% difference between samplers, based on a coefficient of variation of 20% using a two-sided test.
Sampler efficiency was also analyzed by comparing the mean and standard deviation of each particle size for both flow rates to that of the IPM (Equation (1)) and low-velocity inhalability curves (Equation (2)):
| (1) |
where IPM (dae) is the inhalable particulate matter collection efficiency and dae = aerodynamic diameter of particle in μm; and
| (2) |
where I(dae) is the low wind inhalability collection efficiency. The low-velocity inhalability curve has shown that it more closely represents particles inhaled at lower wind velocities.[20]
Results and discussion
The mean concentration and standard deviation of the samples run at the 2 L/min flow rate as compared to the mean concentration of the samples run at 10 L/min are shown in Table 1. Mean concentrations for all particle sizes collected at 2 L/min and 10 L/min were not statistically significantly different from each other, although some discrepancies were apparent. Overall, the 2 L/min concentrations had less variability relative to the 10 L/min concentrations. The largest concentration difference between 2 L/min and 10 L/min flow rates was 17% at particle size 4.9 μm, however this difference was not statistically significant.
Table 1.
Concentration by particle size. P-values were determined of the concentration of each particle size using the Wilcoxon signed rank test.
| Particle Size (μm) | @ 2 L/min, mg/m3 | @ 10 L/min, mg/m3 | p | ||
|---|---|---|---|---|---|
| Mean | Standard Dev. | Mean | Standard Dev. | ||
| 4.9 | 21.8 | 2.9 | 25.5 | 3.1 | 0.08 |
| 9.5 | 22.8 | 4.3 | 21.6 | 3.6 | 0.38 |
| 12.8 | 21.6 | 3.8 | 24.5 | 3.7 | 0.10 |
| 32.7 | 21.5 | 4 | 20.9 | 1.7 | 0.31 |
|
| |||||
| p(total) = 0.36 | |||||
Looking back at a few individual samples within the same test, there were some samples operated at the same flow rate that show an unexplainable variance. For example, two samples operating at 2 L/min collected similar concentrations (29.5 mg/m3 and 31.5 mg/m3), while the third sample at 2 L/min was different (23.5 mg/m3). This could be due to the fact that the capsule top (Figure 1b) that sits just inside the inlet (Figure 1c) may not have been completely sealed. This would create a gap between the two parts that could result in under sampling with that sampler. Other reasons could be random operator error, or an unknown error with the performance of the wind tunnel during any given test.
A Wilcoxon signed rank test was conducted for each particle size to compare the means between the concentration of samplers run at the 2 L/min and 10 L/min flow rate. The p-value for each particle size (p(4.9 μm) = 0.08; p(9.5 μm) = 0.38; p(12.8 μm) = 0.10; p(32.7 μm) = 0.31) suggests that there was not a significant difference in concentration measurements when operating the sampler at 10 L/min as compared to 2 L/min. At particle sizes 4.9 μm and 12.8 μm, the p-values of 0.08 and 0.10, respectively, trended toward significance but was still above the significance level (p = 0.05). A Wilcoxon signed rank test was also conducted on all particle sizes together, which again showed no statistical difference in measured concentrations between the flow rates (p(total) = 0.36). Although there was not a statistical difference between the two flow rates, for 69% of the tests carried out, the 10 L/min samples had a higher mean concentration than the 2 L/min samples. On average for all experiments, concentrations collected at 10 L/min were about 14% different than at 2 L/min.
The sampler efficiency data are shown in Table 2. There were four repeat tests for each of the three samplers. These repeat tests were conducted for each particle size. The average of the three samples per test (for a total of 12 data points) was taken to analyze the sampler efficiency (n = 48). Those data points were then compared to both the IPM criteria (Equation (1)) and the low wind inhalability (Equation (2)), as shown in Figure 4. On average for each particle size, the efficiency of the new inhalable sampler at 2 L/min was found to be between 6–21% different from proposed low-velocity inhalability criterion. The sampler efficiency at 10 L/min was found to be within a range of 3–11% from the low-velocity inhalability criterion.
Table 2.
Fractional sampler efficiency of the new sampler at 2 L/min vs. 10 L/min flow rates.
| Particle Size (μm) | @ 2 L/min, mg/m3 | @ 10 L/min, mg/m3 | ||
|---|---|---|---|---|
| Mean | Standard Dev. | Mean | Standard Dev. | |
| 4.9 | 0.78 | 0.17 | 0.89 | 0.13 |
| 9.5 | 0.9 | 0.12 | 0.87 | 0.08 |
| 12.8 | 0.84 | 0.21 | 0.92 | 0.02 |
| 32.7 | 1.01 | 0.34 | 0.97 | 0.22 |
Figure 4.
Comparison of sampler collection efficiency of the new sampler at 2 L/min (●) vs 10 L/min (○) flow rates. Data points are slightly offset to enable comparison of error bars, which represent one standard deviation. The data are compared against the inhalable particulate matter (IPM) criterion (solid line) and the low-velocity inhalability curve (dashed line).
At the largest particle size tested here (32.7 μm), the sampler seems to have over sampled relative to both curves at both flow rates. In general, the samples run at 10 L/min followed the low-velocity inhalability curve a little closer than the samples run at 2 L/min, which is not surprising when considering isokinetic sampling theory. However, based on our analysis, there seems to be no statistical difference between the concentrations measured by the two flow rates. For the three smallest particle sizes, the samplers at both flow rates underestimated the low-wind inhalability curve, which could suggest that at both flow rates the sampler is potentially underestimating worker’s exposure to that fraction of inhalable particles. Overall, however, the sampler did appear to follow the low-wind inhalability curve. Compared to the IPM, the samplers at both flow rates also followed the curve with the exception of the largest particle size (32.7 μm) and for the 2 L/min sampler at the smallest particle size (4.9 μm). Further research should involve extending the range of particle sizes to cover the entire inhalable range up to 100 μm.
Some limitations to the study include the fact that larger particle sizes (>32.7 μm) were not tested. This was because initial testing of the new sampler at 2 L/min in the same wind tunnel showed the sampler greatly overestimating the low-velocity inhalability curve and IPM curve for large particle sizes.[10] This was due to problems inherent in the wind tunnel design (which requires both upstream and overhead injection of large particles). It is still highly relevant to assess whether a 10 L/min flow rate is acceptable for particles on the smaller end of inhalable particle sizes. However, the next step in building upon the current research is to improve the wind tunnel so that it can accurately generate uniform concentrations of larger particle sizes and the full spectrum of potential exposures can be assessed.
Strengths of this study include that sampling at the 2 L/min flow rate and 10 L/min flow rate occurred simultaneously and within the same controlled environment. This assured a greater equivalency in particle exposure and decreased variability in the external environment. Another strength of this study was its use of the same material (alumina oxide powder) for all four particle sizes. Given that this is the first study to compare the prototype sampler’s performance at two different flow rates, the use of a single material provides a clear comparison of the sampler’s efficiency for multiple particle sizes at two sampling flow rates relevant to field exposure studies. There is little research on increasing the flow rate for inhalable air sampling devices and this study could open the discussion to testing other samplers.
This study was a good starting point for investigating the strengths and limitations of the prototype sampler. Future research should investigate the sampler’s efficiency at the two flow rates with a wider range of particle sizes and with a variety of materials.
Conclusion
After conducting a side-by-side test of the newly designed inhalable aerosol sampler at different sampling flow rates, it is suggested that there is not a significant difference in either the concentration sampled or the sampler efficiency when operating the sampler at 10 L/min as compared to 2 L/min. Operating the new sampler at 10 L/min could improve accuracy as it pertains to assessing personal exposure by enabling lower concentrations to be quantified. In this respect, the risk of not having enough material on the filter for lab analysis would be reduced. Increasing the flow rate would also enable the ability to sample for less time while still collecting the same sample volume. Task-based sampling is a good example of a benefit of increased flow rates with less sampling time. Overall, these changes could provide improved exposure assessment methods for the practicing industrial hygienist
Acknowledgments
The authors would like to thank Ms. Tracy Rees for her review of this article.
Funding
The National Institute for Occupational Safety and Health (NIOSH) funded this project through Grant R01/OH010295.
References
- 1.Nieboer E, Thomassen Y, Chashchin V, Odland JO. Occupational exposure assessment. J Environ Monit. 2005;7:411–415. [PubMed] [Google Scholar]
- 2.Omland O. Exposure and respiratory health in farming in temperate zones-a review of the literature. Ann Agricult Environ Med. 2002;9(2):119–136. [PubMed] [Google Scholar]
- 3.Spaan S, I, Wouters M, Oosting I, Doekes G, Heederik D. Exposure to inhalable dust and endotoxins in agricultural industries. J Environ Monitor. 2006;8(1):63–72. doi: 10.1039/b509838f. [DOI] [PubMed] [Google Scholar]
- 4.Greskevitch M, Kullman G, Bang KM, Mazurek JM. Respiratory disease in agricultural workers: mortality and morbidity statistics. J Agromed. 2008;12(3):5–10. doi: 10.1080/10599240701881482. [DOI] [PubMed] [Google Scholar]
- 5.Ulvestad B, Bakke B, Melbostad E, Fuglerud P, Kongerud J, Lund MB. Increased risk of obstructive pulmonary disease in tunnel workers. Thorax. 2000;55(4):277–282. doi: 10.1136/thorax.55.4.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ameille J, Wild P, Choudat D, et al. Respiratory symptoms, ventilator impairment, and bronchial reactivity in oil mist-exposed automobile workers. Am J Industr Med. 1995;27(2):247–256. doi: 10.1002/ajim.4700270209. [DOI] [PubMed] [Google Scholar]
- 7.Greaves IA, Eisen EA, Smith TJ, et al. Respiratory health of automobile workers exposed to metal-working fluid aerosols: respiratory symptoms. Am J Industr Med. 1997;32(5):450–459. doi: 10.1002/(sici)1097-0274(199711)32:5<450::aid-ajim4>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 8.Kreiss K, Mroz MM, Newman LS, Martyny J, Zhen B. Machining risk of beryllium disease and sensitization with median exposures below 2 μg/m3. Am J Industr Med. 1996;30(1):16–25. doi: 10.1002/(SICI)1097-0274(199607)30:1<16::AID-AJIM3>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 9.NIOSH. Work-Related Lung Disease Surveillance Report, 2007. National Institute for Occupational Safety and Health, Department of Health and Human Services; 2008. [Google Scholar]
- 10.L’Orange C, Anderson K, Sleeth D, Anthony R, Volckens J. A simple and disposable sampler for inhalable aerosol. Ann Occup Hyg. 2016;60(2):150–1160. doi: 10.1093/annhyg/mev065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mark D, Vincent JH. A new personal sampler for airborne total dust in workplaces. Ann Occup Hyg. 1986;30:89–102. doi: 10.1093/annhyg/30.1.89. [DOI] [PubMed] [Google Scholar]
- 12.Bartley DL. Inhalable aerosol sampling. Appl Occup Environ Hyg. 1998;13:274–278. [Google Scholar]
- 13.Görner P, Simon X, Wrobel R, Kauffer E, Witschger O. Laboratory study of selected personal inhalable aerosol samplers. Ann Occup Hyg. 2010;54(2):165–187. doi: 10.1093/annhyg/mep079. [DOI] [PubMed] [Google Scholar]
- 14.ACGIH. TLVs and BEIs. Threshold Limit Values for Chemical Substances and Physical Agents and Biological Exposure Indices. Cincinnati, OH: ACGIH; 2015. p. 77. [Google Scholar]
- 15.Cheng YS, Zhou Y, Irvin CM, et al. Characterization of marine aerosol for assessment of human exposure to brevetoxins. Environ Health Perspect. 2005;113(5):638–643. doi: 10.1289/ehp.7496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhou Y, Cheng YS. Evaluation of IOM personal sampler at different flow rates. J Occup Environ Hyg. 2009;7:88–93. doi: 10.1080/15459620903418746. [DOI] [PubMed] [Google Scholar]
- 17.Anthony TR, Sleeth D, Volckens J. Sampling efficiency of modified 37-mm sampling cassettes using computational fluid dynamics. J Occup Environ Hyg. 2016;13(2):148–158. doi: 10.1080/15459624.2015.1091961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schmees DK, Wu YH, Vincent JH. Experimental methods to determine inhalability and personal sampler performance for aerosols in ultra-low wind speed environments. J Environ Monit. 2008;10(2):1426–1436. doi: 10.1039/b806431h. [DOI] [PubMed] [Google Scholar]
- 19.Baldwin PEJ, Maynard AD. A survey of wind speeds in indoor workplaces. Ann Ocup Hyg. 1998;42(5):303–313. doi: 10.1016/s0003-4878(98)00031-3. [DOI] [PubMed] [Google Scholar]
- 20.Sleeth DK, Vincent JH. Performance study of personal inhalable aerosol samplers at ultra-low wind speeds. Ann Occup Hyg. 2012;56(2):207–220. doi: 10.1093/annhyg/mer089. [DOI] [PubMed] [Google Scholar]
- 21.International Organization of Standards. ISO 9000: International Standards for Quality Management. International Organization of Standards; 1992. [Google Scholar]
- 22.World Health Organization. Hazard Prevention and Control in the Work Environment: Airborne Dust. Power to the People Energy in Europe over the Last Five Centuries. 2014;99(14):1–11. [Google Scholar]
- 23.Koehler KA, Anthony TR, Van Dyke M. Solid versus liquid particle sampling efficiency of three personal aerosol samplers when facing the wind. Ann Occup Hyg. 2012;56(2):194–206. doi: 10.1093/annhyg/mer077. [DOI] [PMC free article] [PubMed] [Google Scholar]