Abstract
Objective
This study assessed healthcare seeking patterns of families of infants with circumcision-related morbidities and families of infants with acute illnesses in rural Ghana.
Design
Two population-based cohort studies.
Setting
Brong Ahafo Region of central rural Ghana.
Participants
A total of 22 955 infants enrolled in a large population-based trial (Neovita trial) from 16 August 2010 to 7 November 2011 and 3141 infants in a circumcision study from 21 May 2012 to 31 December 2012.
Primary outcome
Care seeking for circumcision-related morbidities and acute illnesses unrelated to circumcision.
Results
Two hundred and thirty (8.1%) infants from the circumcision study had circumcision-related morbidities and 6265 (27.3%) infants from the Neovita study had acute illnesses unrelated to circumcision. A much lower proportion (35, 15.2%) of families of infants with circumcision-related morbidities sought healthcare compared with families of infants with acute illnesses in the Neovita study (5520, 88.1%). More families sought care from formal providers (24, 69%) compared with informal providers (11, 31%) for circumcision-related morbidities. There were no obvious determinants of care seeking for acute illnesses or circumcision-related morbidities in the population.
Conclusions
Government and non-government organisations need to improve awareness about the complications and care seeking needed for circumcision-related morbidities.
Keywords: public health, epidemiology, paediatric urology
Strengths and limitations of this study.
A major strength of this study is the use of two large community and population-based cohort studies.
This is the first study to our knowledge to have compared health seeking patterns between families of infants with circumcision-related morbidities and families of infants with acute illnesses that are not circumcision related.
The main limitation was the small sample size in our circumcision cohort due to the low level of healthcare seeking so we were unable to statistically compare care seeking in the circumcision and total study cohort. However, we were able to assess the association between key sociodemographic factors and healthcare seeking patterns in the larger Neovita cohort of 22 955 mother–infant pairs.
Introduction
Infant male circumcision is a common surgical procedure and is performed for cultural, religious and medical reasons. Approximately 90% of men aged under 12 weeks are circumcised in Ghana1 and much of West Africa.2 We reported concerning high risk of circumcision-related morbidity (8.1%), following infant male circumcision in our community-based study in rural Ghana.1 Overall, 53% of the complications were observed following circumcision performed by an informal provider (including village-based traditional circumcision providers) and 47% after circumcision performed by formal healthcare providers including doctors, nurses and medical assistants.1
Appropriate healthcare seeking for infants with circumcision-related morbidities could minimise the occurrence of severe long-term and short-term morbidities. Studies conducted in rural Ghana have reported that poor women believe infant illnesses related to traditional practices are not meant to be managed in the hospital or clinic.3–5 However, no other data on care seeking for infant male circumcision-related morbidity in rural African areas are available. There are more studies that have examined the determinants of care seeking for acute infectious diseases and newborn complications in rural Africa.6 7 A recent study conducted among mothers and infants in Ghana identified poor healthcare seeking behaviour in families of infants with acute illness during the postpartum period. In this study, 29% and 54% of sick infants received healthcare within 2 and 14 days, respectively.8 Another Ghanaian study identified poverty and personal preferences as key determinants of poor care seeking behaviour by families of infants with illness.9 A study from Burkina Faso also linked traditional concepts of illness in Africa to delays in seeking professional medical care by families of infants with malaria.10 Distance to health facility, health provider attitude and inadequate supplies have also been reported as key determinants of delayed care seeking for malaria cases in infants in sub-Saharan African populations.11 However, it appears that there have been no studies which have compared health seeking behaviour between families of infants with circumcision-related morbidities and families of infants with acute illnesses that are not circumcision related.
The overall aim of this study was to assess healthcare seeking patterns of families of infants with circumcision-related morbidities and families of infants with other acute illnesses in rural Ghana. The primary objective was to investigate whether there were differences in the healthcare seeking patterns of families of infants with circumcision-related problems, including infants who died and families of infants with acute illnesses. The secondary objective was to assess the factors that influence care seeking patterns of families in the study area.
Methods
Study design and setting
Data from two separate cohort studies in the same part of the Brong Ahafo Region of central Ghana were analysed separately and compared descriptively. The larger of the two cohorts includes data from a population-based trial of newborn vitamin A supplementation (Neovita trial), conducted between 16 August 2010 and 7 November 2011 and involving 22 955 mother–infant pairs; full details have been published previously.12 The smaller cohort was conducted between 21 May 2012 and 31 December 2012 and focused on circumcision. This was implemented to obtain additional observational data on births, cause-specific mortality and circumcision-related morbidity in the study area. Over the period from 2010 to 2012, 80% of the study population lived in rural settlements and 20% of mothers had no primary school education. Four major district hospitals and over 80 small health facilities provided healthcare services to the population. There were 30 doctors and 44 other formal health service providers (medical assistants and nurses) providing curative services in the four district hospitals at the time of the circumcision study. There were also approximately 120 informal care providers such as drug sellers, traditional healers and religious leaders in the study area.
Data collection
For the Neovita study, from August 2010 to November 2011, all births in the study area were reported to the trial team via a network of fieldworkers. Fieldworkers visited all families at home between 2 hours and 2 days after birth and interviewed the mother of the infant or the primary caregiver. Fieldworkers weighed the baby and asked the mother or the primary caregiver about: date of birth, site of birth, current address, distance to health facilities, sociodemographic characteristics and socioeconomic information (using an asset index). At the monthly surveillance visits, the families were asked by fieldworkers for detailed information on infant illness including start and end dates and healthcare seeking during infant illness. Due to time constraints, families were not asked exactly who they sought care from. The fieldworkers also asked the families who sought healthcare whether the infant was admitted to hospital. The fieldworkers next reviewed infant health records and checked for consistency with family’s report. The fieldworkers also collected data on the vital status of the baby (including if the baby was alive, dead or hospitalised).
The circumcision study included all male live-born infants who were born in the study population from May to December 2012 and were aged under 12 weeks. Follow-up visits were scheduled between 8 to 11 weeks postbirth and trained senior fieldworkers asked for consent to collect additional detailed data on: age at circumcision, site of circumcision and type of circumcision provider. The fieldworkers asked about circumcision morbidities and whether these morbidities had been confirmed by a trained health professional. Families were also asked if they sought care for circumcision-related morbidities and if they had been given advice about potential problems or care seeking. The fieldworkers also asked detailed information on the following: site of healthcare, type of healthcare provider, medicines prescribed, admissions and surgery. Consent to access the baby’s Neovita data including socioeconomic, sociodemographic and care seeking was obtained.
In both studies the fieldworkers were trained for 2 weeks in all study procedures prior to the commencement of the study. Inter-rater reliability was checked between all fieldworkers. We did not perform statistical evaluation of agreements between the fieldworkers and the study coordinator (GT). However, each fieldworker was supervised during two visits per month as part of the study scheduled and unscheduled supervisory visits. During these visits, GT and field supervisors observed the fieldworker interviewing mothers and examined infants and recorded findings independently. Recorded data were compared between the fieldworker and GT/field supervisor and used to provide feedback after the home visits and at weekly fieldworker meetings. The fieldworkers used standardised paper-based data collection tools (including a standardised list of closed-ended questions) for all interviews.
Study definitions
We defined a formal healthcare service as medical care provided at hospitals, clinics or health posts by professionally trained, licensed and regulated providers of medical services including: doctors, medical assistants, nurses or pharmacists. An informal healthcare service was defined as care provided by untrained, unlicensed, unregulated private provider of care services including: drug sellers, traditional healers and religious leaders. Circumcision-related morbidities were defined as complications occurring during or after the circumcision procedure as reported by the primary caregiver including: excess skin removal or incision, excess bleeding, inadequate skin removal, infection, abnormal stream of urine, glans amputation, ulcer.1 Acute illnesses were defined as illnesses or injuries other than circumcision-related complications such as malaria, sepsis, acute respiratory tract infection or diarrhoea.13 14 A formal circumcision provider referred to professionally trained, licensed and regulated providers of medical services. This included: doctors, medical assistants or nurses. An informal circumcision provider was an untrained, unlicensed, unregulated private provider of medical services including: drug sellers, domestic staff, family members and Wanzams (village-based traditional circumcision providers).
Outcome
Our primary outcome was care seeking. In the circumcision study, we defined care seeking as the percentage of families of infants who sought care from either a formal healthcare provider or an informal care provider among families who reported of an infant having a circumcision-related morbidity after circumcision during the circumcision follow-up visits (occurred between 8 and 11 weeks postbirth). In the Neovita study, care seeking was defined as the percentage of families of infants with acute illnesses unrelated to circumcision who sought care outside the home of the infant as reported by caregivers during the Neovita infant follow-up visits (from 4 weeks up to 52 weeks of age).
Statistical analysis
Two hundred and thirty (8.1%) infants had circumcision-related morbidities and of these, only 35 (15.2%) families sought care. Thus, we reported care seeking patterns in our circumcised cohort only using simple proportions and descriptive analyses. Statistical analyses were used to assess care seeking patterns in the larger Neovita cohort of 22 955 infants. Multivariable logistic regression models were constructed a priori to assess the association between care seeking patterns and morbidity risk and adjusted for the effect of important explanatory variables including: religion, maternal education level, maternal age, distance to health facility, site of delivery, sex, birth weight and income status. Adjusted ORs (aORs) and 95% CI were calculated. All analyses were conducted in STATA V.13.
Ethical issues
Ethical approvals were obtained from Ghana Health Service Ethical Review Committee, the institutional ethics committee of Kintampo Health Research Centre, the research ethics committee of London School of Hygiene and Tropical Medicine and the human research ethics committee of the University of Western Australia. Written informed consent was obtained from all the families of the circumcised male infants.
Results
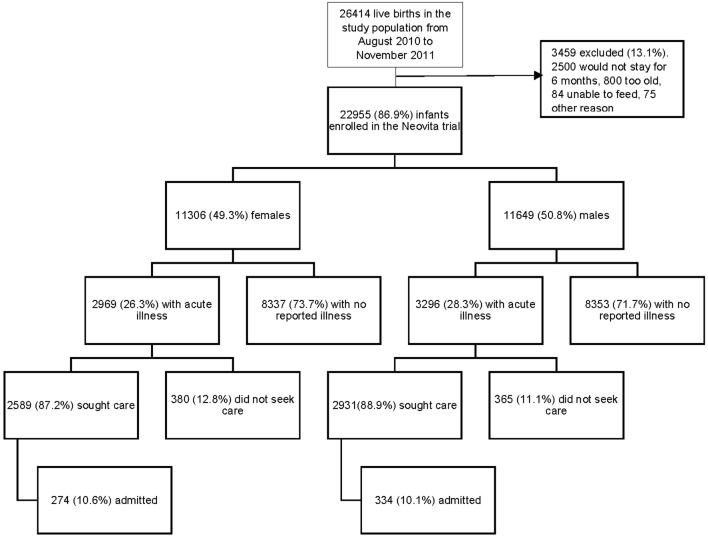
From 16 August 2010 to 7 November 2011, 22 955 infants comprising 11 649 (50.8%) males and 11 306 (49.3%) females were recruited into the Neovita trial (figure 1). A total of 4510 (19.7%) of the mothers were in the lowest socioeconomic quintile, 17 581 (76.6%) delivered in a health facility and 7127 (31.1%) had no primary education (table 1).
Figure 1.
Flow diagram for live births from August 2010 to November 2011 included in the Neovita study.
Table 1.
Characteristics of families and infants who sought care for acute illness in the Neovita trial
| Characteristics | Neovita study population | Neovita trial infants with acute illness | Neovita trial infants with acute illness whose families sought care |
| n=22 955 | n=6265 (27.3%) | n=5520 (88.1%) | |
| Religion | |||
| Christian | 15 979 | 4314 (27.0%) | 3820 (88.5%) |
| Muslim | 5511 | 1566 (28.4%) | 1357 (86.7%) |
| Traditional Africa/none | 1465 | 385 (26.3%) | 343 (89.1%) |
| Missing data | – | – | – |
| Mother’s highest educational level | |||
| None | 7127 | 2009 (28.2%) | 1752 (86.2%) |
| Primary | 4236 | 1241 (29.3%) | 1088 (87.7%) |
| Secondary | 11 578 | 3013 (26.0%) | 2678 (88.9%) |
| Carer did not know | 14 | 2 (14.3%) | 2 |
| Income status of household | |||
| 1 (Lowest) | 4510 | 1316 (29.2%) | 1147 (87.2%) |
| 2 | 4550 | 1297 (28.5%) | 1147 (88.4%) |
| 3 | 4583 | 1274 (27.8%) | 1130 (88.7%) |
| 4 | 4644 | 1212 (26.1%) | 1063 (87.7%) |
| 5 (Highest) | 4668 | 1166 (25.0%) | 1033 (88.6%) |
| Missing data | – | – | – |
| Maternal age (years) | |||
| Less than 20 | 2646 | 760 (28.7%) | 658 (86.6%) |
| 20–29 | 12 041 | 3269 (27.1%) | 2900 (88.7%) |
| 30 or more | 8239 | 2228 (27.0%) | 1954 (87.7%) |
| Carer did not know | 30 | 8 (26.7%) | 8 |
| Site of delivery | |||
| Health facility | 17 581 | 4775 (27.2%) | 4213 (88.2%) |
| Home | 5374 | 1490 (27.7%) | 1307 (87.7%) |
| Missing data | – | – | |
| Distance to health facility | |||
| <1 km | 13 880 | 3657 (26.3%) | 3234 (88.4%) |
| 1–4.9 km | 5285 | 1497 (28.3%) | 1324 (88.4%) |
| 5–10 km | 2950 | 752 (25.5%) | 646 (85.9%) |
| 10 km or more | 1197 | 359 (30.0%) | 316 (88.0%) |
| Missing data | – | – | – |
| Birth weight | |||
| Less than 2.5 kg | 3592 | 998 (27.8%) | 867 (86.9%) |
| 2.5 kg or greater | 19 361 | 5267 (27.2%) | 4653 (88.3%) |
| Missing data | – | – | – |
| Sex | |||
| Male | 11 649 | 3296 (28.3%) | 2931 (88.9%) |
| Female | 11 306 | 2969 (26.3%) | 2589 (87.2%) |
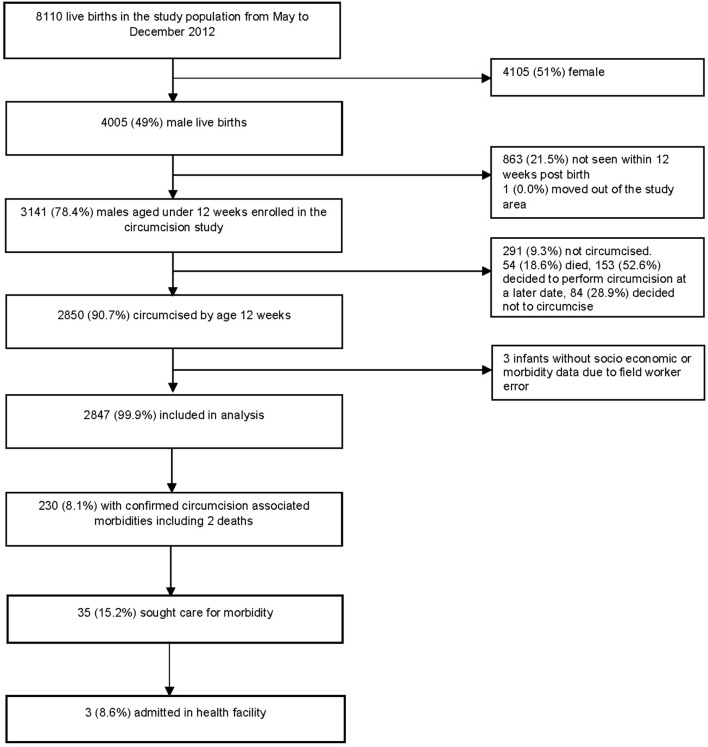
From 21 May to 31 December 2012, 3141 male infants were recruited in the circumcision study (figure 2). Overall, 2850 (90.7%) of these infants were circumcised. We excluded three babies (0.1%) who had no socioeconomic or sociodemographic data. A total of 503 (16.0%) of mothers were in the lowest income quintile; 2479 (78.9%) delivered in a facility and 601 (19.1%) had no primary education (table 2).
Figure 2.
Flow diagram for live births from May 2012 to December 2012 included in the circumcision study.
Table 2.
Characteristics of families and infants who sought care for morbidity in the circumcision study
| Characteristics | Circumcision study population | Circumcised infants | Circumcised infants with morbidity | Circumcised infants with morbidity whose families sought care |
| n=3141 | n=2850* (90.7%) | n=230 (8.1%) | n=35 (15.0%) | |
| Religion | ||||
| Christian | 2234 | 2048 (91.7%) | 172 (8.4%) | 24 (14.0%) |
| Muslim | 727 | 666 (91.6%) | 49 (7.4%) | 9 (18.4%) |
| Traditional Africa/none | 171 | 129 (75.4%) | 9 (7.0%) | 2 (22.2%) |
| Missing data | 9 | 7 (77.8%) | – | – |
| Mother’s highest educational level | ||||
| None | 601 | 512 (85.2%) | 50 (9.8%) | 6 (12.0%) |
| Primary | 1619 | 1481 (91.5%) | 127 (8.6%) | 21 (16.5%) |
| Secondary | 913 | 850 (93.1%) | 53 (6.2%) | 8 (15.1%) |
| Carer did not know | 8 | 7 (87.5%) | – | – |
| Income status of household | ||||
| 1 (Lowest) | 503 | 387 (76.9%) | 28 (7.2%) | 6 (21.4%) |
| 2 | 608 | 532 (87.5%) | 41 (7.7%) | 4 (9.8%) |
| 3 | 676 | 628 (92.9%) | 47 (7.5%) | 9 (19.1%) |
| 4 | 725 | 687 (94.8%) | 62 (9.0%) | 8 (12.9%) |
| 5 (Highest) | 629 | 613 (97.5%) | 52 (8.5%) | 8 (15.4%) |
| Missing data | 0 | 3 (0.1%) | – | – |
| Maternal age (years) | ||||
| Less than 20 | 360 | 319 (88.6%) | 26 (8.2%) | 3 (11.5%) |
| 20–29 | 1603 | 1458 (91.0%) | 130 (8.9%) | 18 (13.8%) |
| 30 or more | 1170 | 1066 (91.1%) | 74 (6.9%) | 14 (18.9%) |
| Carer did not know | 8 | 7 (87.5%) | – | – |
| Site of delivery | ||||
| Health facility | 2479 | 2292 (92.5%) | 196 (8.6%) | 28 (14.3%) |
| Home | 650 | 549 (84.5%) | 34 (6.2%) | 7 (20.6%) |
| Missing data | 12 | 6 (50.9%) | – | – |
| Distance to health facility | ||||
| <1 km | 1545 | 1444 (93.5%) | 110 (7.6%) | 21 (19.1%) |
| 1–4.9 km | 801 | 741 (92.5%) | 77 (10.4%) | 7 (9.1%) |
| 5–10 km | 484 | 400 (82.6%) | 27 (6.8%) | 3 (11.1%) |
| 10 km or more | 231 | 186 (80.5%) | 14 (7.5%) | 3 (21.4%) |
| Missing data | 80 | 76 (95.0%) | 2 (2.6%) | 1 (50.1%) |
| Birth weight | – | |||
| Less than 2.5 kg | 255 | 214 (83.9%) | 21 (9.1%) | 1 (4.8%) |
| 2.5 kg or greater | 2886 | 2633 (91.2%) | 209 (7.9%) | 34 (16.3%) |
| Missing data | 0 | – | – | – |
*Three circumcised infants had no socioeconomic and demographic data due to field worker error.
Acute illness and care seeking
A total of 6265 (27.3%) Neovita trial infants had an acute illness during the first year of life. There was little difference in the prevalence of acute illness by sex in the Neovita population; 3296 (28.3%) males and 2969 (26.3%) females (figure 1 and table 1). Healthcare was sought for 5520 (88.1%) Neovita trial infants with acute illness and 608 (11.0%) were admitted to hospital (10.6% females and 10.1% males) (figure 1 and table 1). A total of 1033 (88.6%) families who sought care for acute illness were in the highest socioeconomic quintile compared with 1147 (87.2%) in the lowest quintile, 4213 (88.2%) delivered in a health facility compared with 1307 (87.7%) who delivered at home and 2678 (88.9%) had more than primary school education compared with 1752 (86.2%) with no formal education (table 1).
A slightly lower proportion of families of female infants with acute illness (87.2%) sought care compared with families of male infants (88.9%) (aOR 0.85, 95% CI 0.73 to 0.99, p=0.039) (table 3). Surprisingly, there were no obvious differences in the prevalence of healthcare seeking related to levels of education (aOR 0.89, 95% CI 0.72 to 1.10, p=0.260), socioeconomic status (aOR 1.00, 95% CI 0.75 to 1.33, p=0.848), maternal age (aOR 1.15, 95% CI 0.89 to 1.48, p=0.131), site of delivery (aOR 1.01, 95% CI 0.83 to 1.24, p=0.886), distance to health facility (aOR 0.96, 95% CI 0.68 to 1.37, p=0.369) or birth weight (aOR 0.89, 95% CI 0.72 to 1.09, p=0.260) in the Neovita trial population (table 3).
Table 3.
Predictors of care seeking behaviour in the Neovita trial population
| Characteristics | Neovita study population | Neovita trial infants with acute illness | Neovita trial infants whose families sought care | Unadjusted OR | p Value | Adjusted OR* | p Value |
| n=22 955 | n=6265 (27.3%) | n=5520 (88.1%) | |||||
| Religion | |||||||
| Christian | 15 979 | 4314 (27.0%) | 3820 (88.5%) | 1.00 | 0.121 | 1.00 | 0.195 |
| Muslim | 5511 | 1566 (28.4%) | 1357 (86.7%) | 0.84 (0.70 to 1.00) | 0.86 (0.72 to 1.03) | ||
| Traditional Africa/none | 1465 | 385 (26.3%) | 343 (89.1%) | 1.06 (0.76 to 1.47) | 1.10 (0.79 to 1.55) | ||
| Missing data | – | – | |||||
| Mother’s highest educational level | |||||||
| None | 7127 | 2009 (28.2%) | 1752 (86.2%) | 0.89 (0.73 to 1.09) | 0.89 (0.72 to 1.10) | ||
| Primary | 4236 | 1241 (29.3%) | 1088 (87.7%) | 0.85 (0.72 to 1.01) | 0.84 (0.69 to 1.03) | ||
| Secondary | 11 578 | 3013 (26.0%) | 2678 (88.9%) | 1.00 | 0.174 | 1.00 | 0.260 |
| Carer did not know | 14 | 2 (14.3%) | 2 | – | |||
| Income status of household | |||||||
| 1 (Lowest) | 4510 | 1316 (29.2%) | 1147 (86.6%) | 0.87 (0.69 to 1.11) | 1.00 (0.75 to 1.33) | ||
| 2 | 4550 | 1297 (28.5%) | 1147 (86.4%) | 0.98 (0.77 to 1.26) | 1.07 (0.82 to 1.39) | ||
| 3 | 4583 | 1274 (27.8%) | 1130 (88.7%) | 1.01 (0.79 to 1.30) | 1.08 (0.83 to 1.39) | ||
| 4 | 4644 | 1212 (26.1%) | 1063 (87.7%) | 0.92 (0.72 to 1.18) | 0.95 (0.74 to 1.22) | ||
| 5 (Highest) | 4668 | 1166 (25.0%) | 1033 (88.6%) | 1.00 | 0.714 | 1.00 | 0.848 |
| Missing data | – | – | – | ||||
| Maternal age (years) | |||||||
| Less than 20 | 2646 | 760 (28.7%) | 658 (86.6%) | 1.00 | 0.208 | 1.00 | 0.131 |
| 20–29 | 12 041 | 3269 (27.1%) | 2900 (88.7%) | 1.22 (0.96 to 1.54) | 1.23 (0.97 to 1.57) | ||
| 30 or more | 8239 | 2228 (27.0%) | 1954 (87.7%) | 1.11 (0.87 to 1.41) | 1.15 (0.89 to 1.48) | ||
| Carer did not know | 30 | 8 (26.7%) | 8 | – | |||
| Site of delivery | |||||||
| Health facility | 17 581 | 4775 (27.2%) | 4213 (88.2%) | 1.00 | 0.595 | 1.00 | 0.886 |
| Home | 5374 | 1490 (27.7%) | 1307 (87.7%) | 0.95 (0.80 to 1.14) | 1.01 (0.83 to 1.24) | ||
| Missing data | – | ||||||
| Distance to health facility | |||||||
| <1 km | 13 880 | 3657 (26.3%) | 3234 (88.4%) | 1.00 | 0.278 | 1.00 | 0.369 |
| 1–4.9 km | 5285 | 1497 (28.3%) | 1324 (88.4%) | 1.00 (0.83 to 1.21) | 0.99 (1.82 to 1.20) | ||
| 5–10 km | 2950 | 752 (25.5%) | 646 (85.9%) | 0.80 (0.63 to 1.00) | 0.80 (0.62 to 1.03) | ||
| 10 km or more | 1197 | 359 (30.0%) | 316 (88.0%) | 0.96 (0.69 to 1.34) | 0.96 (0.68 to 1.37) | ||
| Missing data | – | – | – | – | – | ||
| Birth weight | |||||||
| Less than 2.5 kg | 3592 | 998 (27.8%) | 867 (86.9%) | 0.87 (0.71 to 1.07) | 0.89 (0.72 to 1.09) | ||
| 2.5 kg or greater | 19 361 | 5267 (27.2%) | 4653 (88.3%) | 1.00 | 0.194 | 1.00 | 0.260 |
| Missing data | – | – | – | ||||
| Sex | |||||||
| Male | 11 649 | 3296 (28.3%) | 2931 (88.9%) | 1.00 | 0.035 | 1.00 | 0.039 |
| Female | 11 306 | 2969 (26.3%) | 2589 (87.2%) | 0.84 (0.73 to 0.99) | 0.85 (0.73 to 0.99) | ||
*Adjusted for religion, maternal education, distance to health facility, site of delivery and sex.
Circumcision complications and care seeking
Of the 2847 circumcised male infants included in the circumcision analysis, 230 (8.1%) had confirmed morbidities related to circumcision and two died. Only 35 (15.2%) families of infants with circumcision-related morbidities sought care and 3 (8.6%) were admitted to hospital (figure 2 and table 2).
The proportion of mothers aged less than 20 years who sought care for their infants with circumcision-related morbidity (3 (11.5%)) was slightly lower than mothers aged 30 years or more (14 (18.9%)). Healthcare seeking of mothers of infants with low birth weight was lower (1 (4.8%)) than mothers of infants with normal birth weight though the total numbers were small (34 (16.3%)) (table 2). There were no other obvious determinants of care seeking for circumcision-related morbidity.
Type of provider
In the circumcision study, of the 35 families of infants who sought care for circumcision-related morbidity, 20 (57.1%) infants were circumcised by an informal provider and 15 (42.9%) by a formal provider (table 4). Most families of infants circumcised by a formal provider also sought care from a formal provider for complications (13, 87.7%). In contrast, only 45% (9) families of infants circumcised by an informal provider also sought healthcare for circumcision-related morbidity from an informal healthcare provider (table 4).
Table 4.
Type of healthcare provider for circumcision-related morbidity
| Characteristics | Circumcised infants whose families sought care | Type of healthcare provider for circumcision morbidity | |
| Formal provider | Informal provider* | ||
| n=35 | 24 (68.6%) | 11 (31.4%) | |
| Religion | |||
| Christian | 24 | 17 (70.8%) | 7 (29.2%) |
| Muslim | 9 | 6 (66.7%) | 3 (33.3%) |
| Traditional Africa/none | 2 | 1 (50.0%) | 1 (50.0%) |
| Missing data | – | – | – |
| Mother’s highest educational level | |||
| None | 6 | 2 (33.3%) | 4 (66.7%) |
| Primary | 21 | 15 (71.4%) | 6 (28.6%) |
| Secondary | 8 | 7 (87.5%) | 1 (12.5%) |
| Carer did not know | – | – | – |
| Income status of household | |||
| 1 (Lowest) | 6 | 2 (33.3%) | 4 (66.7%) |
| 2 | 4 | 2 (50.0%) | 2 (50.0%) |
| 3 | 9 | 7 (77.8%) | 2 (22.2%) |
| 4 | 8 | 7 (87.5%) | 1 (12.5%) |
| 5 (Highest) | 8 | 6 (75.0%) | 2 (25.0%) |
| Missing data | – | – | – |
| Maternal age (years) | |||
| Less than 20 | 3 | 3 | – |
| 20–29 | 18 | 11 (61.1%) | 7 (38.9%) |
| 30 or more | 14 | 10 (71.4%) | 4 (28.6%) |
| Carer did not know | – | – | – |
| Site of delivery | |||
| Health facility | 28 | 22 (78.6%) | 6 (21.4%) |
| Home | 7 | 2 (28.6%) | 5 (71.4%) |
| Missing data | – | – | – |
| Distance to health facility | |||
| <1 km | 21 | 18 (85.7%) | 3 (14.3%) |
| 1–4.9 km | 7 | 3 (42.9%) | 4 (57.1%) |
| 5–10 km | 3 | 1 (33.3%) | 2 (66.7%) |
| 10 km or more | 3 | 1 (33.3%) | 2 (66.7%) |
| Missing data | 1 | 1 | – |
| Type of circumcision provider | |||
| Formal provider | 15 | 13 (86.7%) | 2 (13.3%) |
| Informal provider | 20 | 11 (55.0%) | 9 (45.0%) |
| Missing data | 0 | – | – |
| Birth weight | |||
| Less than 2.5 kg | 1 | – | 1 (100.0%) |
| 2.5 kg or greater | 34 | 24 (70.6%) | 10 (29.4%) |
| Missing data | – | – | |
*Informal care provider included drug sellers, traditional healers and religious leaders.
A similar proportion of mothers in the lowest income quintile (4 (66.7%)) sought healthcare for circumcision -related morbidity from an informal care provider compared with mothers in the highest income quintile (2 (25.0%)), however, numbers were low in this analysis (table 4). A greater proportion of mothers who delivered their infants at home (5 (71.4%) sought healthcare for circumcision-related morbidity from an informal care provider compared with mothers with health facility births (6 (21.4%)). The proportion of mothers who lived 10 km or more from a health facility (2 (66.7%)) who sought healthcare for circumcision-related morbidity from an informal care provider was higher than those who lived within 1 km from a health facility (3 (14.3%)). There were no data on type of healthcare provider available from the Neovita trial population.
Discussion
There appeared to be substantial differences in healthcare seeking in families with infants experiencing circumcision-related morbidities and those with other acute illnesses in the Brong Ahafo Region of central rural Ghana. A much lower proportion (15.2%) of families of infants with circumcision-related morbidities sought healthcare compared with families who had an infant with an acute illness in the larger Neovita population (88.1%). However, the proportion of hospital admissions in infants of families who sought healthcare was almost the same (11% in the Neovita study and 9% in the circumcision study). There was some indication that mothers of low birthweight infants had poorer care seeking for circumcision-related morbidities than mothers of infants with normal birthweight infants. There were no other clear determinants of healthcare seeking for acute illnesses or circumcision-related morbidities in our study populations.
A study conducted in Nigeria also reported lower healthcare seeking by families of male infants with circumcision-related morbidities compared with infants with other health problems.15 Other studies have suggested that poor care seeking behaviour after circumcision can be due to family expectations that complications will heal without any intervention,15 16 poor recognition of illness,5 17 18 poor recognition of severity of illness5 19–21 and beliefs that some infant illnesses are not meant to be treated in hospitals.3 5
Interestingly, the proportion of hospital admissions after care seeking was almost the same in the Neovita and circumcision populations (11% of infants with acute morbidities whose families sought care were hospitalised and 9% of infants with circumcision-related morbidities whose families sought healthcare were also hospitalised). This indicates that families may not be seeking care for many circumcised infants in our study area with morbidities that do require hospital admission and specialised hospital care. Overall, hospital admission rates were similar to a recently published study from Ghana that reported rates of 9% to 18%.22
The determinants of care seeking for acute illness have been reported in low-income and middle-income countries.5 23 24 However, few studies have reported population-based data on the care seeking patterns of families with infants who experience circumcision-related morbidities and acute illness. There was some indication that mothers of low birthweight infants had poorer care seeking for circumcision-related morbidities (5%) than mothers of infants with normal birthweight infants (16%) though numbers were small. These findings are similar to other studies that reported poor care seeking for acute illness25 and vaccination26 in families of low birthweight infants. We found no evidence that other socioeconomic and sociodemographic factors influence families’ care seeking behaviour for circumcision-related morbidity and acute illness in our population. These findings contrast with that of other earlier studies from Ghana5 22 26 27 and Bangladesh28 that reported higher care seeking for infants with acute illness by richer families and mothers with higher educational levels. This indicates that healthcare seeking behaviour for acute illness may be improving over time in rural Ghana.
Overall, we found that more families sought care for a circumcision-related morbidity from formal (68.6%) than informal (13.4%) healthcare providers. Unsurprisingly, most families of infants circumcised by a formal provider also sought care from a formal provider for complications. However, fewer families of infants circumcised by an informal provider sought care from an informal provider (45%) than a formal provider (55%). These findings differ from another published study from Kenya16 which reported families of male infants who were circumcised by an informal provider were twofold less likely to seek care for a circumcision-related morbidity from a formal healthcare provider.16 We were not able to assess the type of care provider for acute illness in the Neovita study as these data were not collected in the Neovita study.
Generally, healthcare seeking for acute illness in the Neovita study population was very high (88.1%). The proportion of families seeking healthcare in our study was higher than data reported by the Ghana Demographic and Health Survey in 2008, close to the time of conducting the Neovita study (acute respiratory infection 51.0%, fever 51.0% and diarrhoea 35.2%).29 Care seeking for acute illness in rural populations has also been reported to be around 61% in Kenya,21 47% in Nigeria30 and 27% in Vietnam.31 The high healthcare seeking patterns for acute illnesses seen in our study population may be due to recent communications and promotion of care seeking by the local government district health management teams. However, that these communications do not appear to have influenced care seeking for circumcision-related morbidities to date.
The most important limitation to our study was the small sample size in our circumcision cohort due to the low level of healthcare seeking, so we were unable to statistically compare care seeking in the circumcision and total study cohort. However we were able to assess the association between key sociodemographic factors and healthcare seeking patterns in the 22 955 infants in the community-level population-based Neovita cohort. Another limitation was our use of family-level recall of health service usage which could have led to some episodes of care seeking being under-reported in the circumcised cohort. However, both families and data collectors were blinded to the study hypothesis and our trained fieldworkers reviewed infant health records and checked for consistency with a family’s report. The Neovita study lacked data on the type of provider care was sought from. However, the population-based nature of the data on whether care was sought for acute illnesses serves as a proxy for care seeking patterns. Understanding the type of care provider sought for acute illnesses would be important to investigate in the future
Conclusions
Our study has implications for policy and programme development. Infant male circumcision is commonly practised in many parts of sub-Saharan Africa including our study area. We report substantial differences in healthcare seeking patterns in families in the two cohorts in the Brong Ahafo Region of central rural Ghana. A much lower proportion of families of infants with circumcision-related morbidity sought healthcare for acute morbidity compared with families of infants with acute illness. The findings from this study indicate that government and non-governmental organisations need to prioritise circumcision and improve awareness of this highly prevalent, but potentially dangerous practice. Circumcision carries a triple burden of high prevalence, high morbidity load and poor care seeking. Community awareness of the burden, consequences and solutions needs to increase. This requires the involvement of community leaders and other stakeholders and include behaviour change communication strategies.
Supplementary Material
Acknowledgments
The authors thank the management and staff of the KHRC particularly Oscar Agyei, a data manager, for their continuing support. We also thank all the families and infants who participated in the studies.
Footnotes
Contributors: TG drafted the manuscript which was edited and reviewed by all the authors. KME, TG, KM and NAS designed the study. TG, KME and MO were responsible for the study conduct. TG, KME, KM and MO managed the database and designed the analysis plan. TG analysed the data.
Funding: This study was supported by the University of Western Australia scholarship fund.
Competing interests: None declared.
Patient consent: Detail has been removed from this case description/these case descriptions to ensure anonymity. The editors and reviewers have seen the detailed information available and are satisfied that the information backs up the case the authors are making.
Ethics approval: Ethical approvals were obtained from Ghana Health Service Ethical Review Committee, the institutional ethics committee of Kintampo Health Research Centre, the research ethics committee of London School of Hygiene and Tropical Medicine and the human research ethics committee of the University of Western Australia.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The dataset analysed during the current study is available from the corresponding author on reasonable request and with permission of KME.
References
- 1. Gyan T, McAuley K, Strobel NA, et al. . Determinants of morbidity associated with infant male circumcision: community-level population-based study in rural Ghana. Trop Med Int Health 2017;22:312–22. 10.1111/tmi.12829 [DOI] [PubMed] [Google Scholar]
- 2. Weiss H, Larke N, Halperin D, et al. . Neonatal and child male circumcision: a global review. UNAIDS Technical Bulletin 2010. [Google Scholar]
- 3. Okyere E, Tawiah-Agyemang C, Manu A, et al. . Newborn care: the effect of a traditional illness, asram, in Ghana. Ann Trop Paediatr 2010;30:321–8. 10.1179/146532810X12858955921311 [DOI] [PubMed] [Google Scholar]
- 4. Hill Z, Manu A, Tawiah-Agyemang C, et al. . How did formative research inform the development of a home-based neonatal care intervention in rural Ghana? J Perinatol 2008;28 Suppl 2:S38–S45. 10.1038/jp.2008.172 [DOI] [PubMed] [Google Scholar]
- 5. Hill Z, Kendall C, Arthur P, et al. . Recognizing childhood illnesses and their traditional explanations: exploring options for care-seeking interventions in the context of the IMCI strategy in rural Ghana. Trop Med Int Health 2003;8:668–76. 10.1046/j.1365-3156.2003.01058.x [DOI] [PubMed] [Google Scholar]
- 6. Ansah Manu A, ten Asbroek A, Soremekun S, et al. . Evaluating the implementation of community volunteer assessment and referral of sick babies: lessons learned from the Ghana Newhints home visits cluster randomized controlled trial. Health Policy Plan 2014;29 Suppl 2:ii114–ii127. 10.1093/heapol/czu080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rutherford ME, Mulholland K, Hill PC. How access to health care relates to under-five mortality in sub-Saharan Africa: systematic review. Trop Med Int Health 2010;15:508–19. 10.1111/j.1365-3156.2010.02497.x [DOI] [PubMed] [Google Scholar]
- 8. Okawa S, Ansah EK, Nanishi K, et al. . High Incidence of Neonatal Danger Signs and Its Implications for Postnatal Care in Ghana: A Cross-Sectional Study. PLoS One 2015;10:e0130712 10.1371/journal.pone.0130712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bazzano AN, Kirkwood BR, Tawiah-Agyemang C, et al. . Beyond symptom recognition: care-seeking for ill newborns in rural Ghana. Trop Med Int Health 2008;13:123–8. 10.1111/j.1365-3156.2007.01981.x [DOI] [PubMed] [Google Scholar]
- 10. Beiersmann C, Sanou A, Wladarsch E, et al. . Malaria in rural Burkina Faso: local illness concepts, patterns of traditional treatment and influence on health-seeking behaviour. Malar J 2007;6:106 10.1186/1475-2875-6-106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ahorlu CK, Koram KA, Ahorlu C, et al. . Socio-cultural determinants of treatment delay for childhood malaria in southern Ghana. Trop Med Int Health 2006;11:1022–31. 10.1111/j.1365-3156.2006.01660.x [DOI] [PubMed] [Google Scholar]
- 12. Edmond KM, Newton S, Shannon C, et al. . Effect of early neonatal vitamin A supplementation on mortality during infancy in Ghana (Neovita): a randomised, double-blind, placebo-controlled trial. Lancet 2015;385:1315–23. 10.1016/S0140-6736(14)60880-1 [DOI] [PubMed] [Google Scholar]
- 13. Lambrechts T, Bryce J, Orinda V. Integrated management of childhood illness: a summary of first experiences. Bull World Health Organ 1999;77:582. [PMC free article] [PubMed] [Google Scholar]
- 14. Gove S. Integrated management of childhood illness by outpatient health workers: technical basis and overview. The WHO Working Group on Guidelines for Integrated Management of the Sick Child. Bull World Health Organ 1997;75:7. [PMC free article] [PubMed] [Google Scholar]
- 15. Osifo OD, Oriaifo IA. Circumcision mishaps in Nigerian children. Ann Afr Med 2009;8:266 10.4103/1596-3519.59583 [DOI] [PubMed] [Google Scholar]
- 16. Bailey RC, Egesah O, Rosenberg S. Male circumcision for HIV prevention: a prospective study of complications in clinical and traditional settings in Bungoma, Kenya. Bull World Health Organ 2008;86:669–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Geldsetzer P, Williams TC, Kirolos A, et al. . The recognition of and care seeking behaviour for childhood illness in developing countries: a systematic review. PLoS One 2014;9:e93427 10.1371/journal.pone.0093427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nabiwemba EL, Atuyambe L, Criel B, et al. . Recognition and home care of low birth weight neonates: a qualitative study of knowledge, beliefs and practices of mothers in Iganga-Mayuge Health and Demographic Surveillance Site, Uganda. BMC Public Health 2014;14:546 10.1186/1471-2458-14-546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Paudel M. Male circumcision: care practices and attitudes in a Muslim community of western Nepal. Italian Journal of Public Health 2012;8. [Google Scholar]
- 20. Muula AS, Prozesky HW, Mataya RH, et al. . Prevalence of complications of male circumcision in Anglophone Africa: a systematic review. BMC Urol 2007;7:4 10.1186/1471-2490-7-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Taffa N, Chepngeno G. Determinants of health care seeking for childhood illnesses in Nairobi slums. Trop Med Int Health 2005;10:240–5. 10.1111/j.1365-3156.2004.01381.x [DOI] [PubMed] [Google Scholar]
- 22. Manu A, Hill Z, Ten Asbroek AH, et al. . Increasing access to care for sick newborns: evidence from the Ghana Newhints cluster-randomised controlled trial. BMJ Open 2016;6:e008107 10.1136/bmjopen-2015-008107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Colvin CJ, Smith HJ, Swartz A, et al. . Understanding careseeking for child illness in sub-Saharan Africa: a systematic review and conceptual framework based on qualitative research of household recognition and response to child diarrhoea, pneumonia and malaria. Soc Sci Med 2013;86:66–78. 10.1016/j.socscimed.2013.02.031 [DOI] [PubMed] [Google Scholar]
- 24. Mohan P, Iyengar SD, Martines J, et al. . Impact of counselling on careseeking behaviour in families with sick children: cluster randomised trial in rural India. BMJ 2004;329:266 10.1136/bmj.38149.703380.47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. O’Leary M, Edmond K, Floyd S, et al. . & Thomas L. S. A cohort study of low birth weight and health outcomes in the first year of life, Ghana. Bulletin of the World Health Organization 2017;95:574–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. O’Leary M, Edmond K, Floyd S, et al. . Neonatal vaccination of low birthweight infants in Ghana. Arch Dis Child 2017;102:145–51. Archdischild-2016-311227 10.1136/archdischild-2016-311227 [DOI] [PubMed] [Google Scholar]
- 27. Kirkwood BR, Manu A, ten Asbroek AH, et al. . Effect of the Newhints home-visits intervention on neonatal mortality rate and care practices in Ghana: a cluster randomised controlled trial. Lancet 2013;381:2184–92. 10.1016/S0140-6736(13)60095-1 [DOI] [PubMed] [Google Scholar]
- 28. Shah R, Mullany LC, Darmstadt GL, et al. . Determinants and pattern of care seeking for preterm newborns in a rural Bangladeshi cohort. BMC Health Serv Res 2014;14:417 10.1186/1472-6963-14-417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ghana Statistical Service (GSS), Ghana Health Service (GHS), and ICF Macro. Ghana Demographic and Health Survey 2008. Accra, Ghana: GSS, GHS, and ICF Macro, 2009. [Google Scholar]
- 30. National Population Commission (NPC) [Nigeria] and ICF Macro. Nigeria Demographic and Health Survey 2008. Abuja, Nigeria: National Population Commission and ICF Macro, 2009. [Google Scholar]
- 31. Lee H-Y, Van Huy N, Choi S. Determinants of early childhood morbidity and proper treatment responses in Vietnam: results from the Multiple Indicator Cluster Surveys, 2000–2011. Global Health Action 2016;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.