Abstract
Introduction
In Japan, dipeptidyl peptidase-4 (DPP-4) inhibitors are frequently used as the treatment of choice for patients with type 2 diabetes. In some cases, however, poor glycaemic and body weight control issues persist despite treatment with DPP-4 inhibitors. Previous researchers have revealed that sodium-dependent glucose transporter-2 (SGLT-2) inhibitors reduce both plasma glucose levels and body weight in patients with type 2 diabetes. However, further investigation regarding the effects of SGLT-2 inhibitors on body composition, especially in the Asian population who tends to have relatively low-to-moderate body mass indices, is required. Therefore, we aim to determine the effects of treatment with SGLT-2 inhibitors or metformin for reducing visceral fat in 106 Asian patients with type 2 diabetes who were undergoing treatment with the DPP-4 inhibitor sitagliptin (50 mg daily) for poor glycaemic control.
Methods and analysis
A prospective, multicentre, blinded-endpoint phase IV randomised controlled study will be conducted to evaluate the safety and efficacy of a 24-week treatment with either an SGLT-2 inhibitor (ipragliflozin) or metformin for reducing visceral fat and plasma glucose levels in patients with type 2 diabetes. Patients who satisfy the eligibility criteria will be randomised (1:1) to receive ipragliflozin (50 mg daily) or metformin (1000 mg daily). The primary outcome is the rate of change in the total area of visceral fat for patients in both treatment groups, measured using CT, after 24 weeks of therapy. Two radiologists, blinded to the clinical information, will perform centralised analysis of the images in a unified measurement condition.
Ethics and dissemination
The protocol was approved by the institutional review board of each hospital. This study is ongoing and due to finish in April 2017. The findings of this study will be disseminated via peer-reviewed publications and conference presentations, and will also be disseminated to participants.
Trial registration number
UMIN000015170, R000016861 (https://upload.umin.ac.jp/cgi-open-bin/ctr/ctr_view.cgi?recptno=R000016861); Pre-results
Keywords: sodium-dependent glucose transporter-2 inhibitor, metformin, visceral fat reduction, dipeptidyl peptidase-4 inhibitor, type 2 diabetes, glucose
Strengths and limitations of this study.
The design of this study provides a unique opportunity to examine alternative treatment strategies.
No studies have been conducted to compare the effects of sodium-dependent glucose transporter-2 inhibitors and metformin in patients with type 2 diabetes receiving first-line treatment with dipeptidyl peptidase-4 inhibitors.
CT will be used to measure visceral fat.
This study is not a double-blind study; however, the endpoint evaluation is blinded.
Introduction
Previous researchers have estimated that the number of patients with type 2 diabetes mellitus will continue to increase worldwide, especially in Asia.1 2 While metformin is regarded as the first-choice treatment for patients with type 2 diabetes in the USA, dipeptidyl peptidase-4 (DPP-4) inhibitors are used by 70% of such patients in Japan for efficacy and safety reasons.3 Indeed, it has been indicated that DPP-4 inhibitors are associated with lower risks of hypoglycaemia in Asian patients with type 2 diabetes who tend to have low insulin secretion levels. Some researchers have also speculated that dietary differences may account for some of the efficacy of DPP-4 inhibitors in Asian patients.4–6 In some cases, however, issues with poor glycaemic control and body weight control persist despite treatment with DPP-4 inhibitors.7 In such cases, metformin is recommended as a second-line treatment option. Although the efficacy of metformin, which is associated with a low risk of weight gain and reduced cost, has been supported in numerous studies, the risk of side effects (ie, gastrointestinal disturbances and severe lactic acidosis) often leads to low medication adherence.
Sodium-dependent glucose transporter-2 (SGLT-2) inhibitors have recently been developed, which differ from existing diabetic medications in that they reduce plasma glucose levels by promoting glucose excretion in urine.8 Moreover, researchers have indicated that SGLT-2 inhibitors also reduce body weight.9 10 However, the effects of these medications on body composition need to be fully elucidated. The reduction of visceral fat is expected to lead to improvements in metabolic syndrome and prevention of atherosclerotic disease. In a previous study, the SGLT-2 inhibitor, empagliflozin, was observed to exert cardioprotective effects in patients with type 2 diabetes.11 Adherence to treatment with SGLT-2 inhibitors is expected to be high; however, there is concern that SGLT-2 inhibitors may cause a loss of muscle and bone mass, and lead to osteoporosis and decreased physical function.10 12
Visceral fat obesity has been associated with diabetes, dyslipidaemia and hypertension.13 However, reductions in the amount of visceral fat can lead to metabolic improvements in patients with diabetes. It has been previously indicated that even a 3% reduction in body weight has a clinically significant effect on the symptoms of obese patients with diabetes.14 However, no studies have been conducted to date to compare the effects of SGLT-2 inhibitors and metformin on visceral fat reduction in patients taking DPP-4 inhibitors.
In a previous study, treatment with dapagliflozin and metformin resulted in body weight reductions, which accounted for a 2/3 reduction in fat, in patients with type 2 diabetes.10 However, this study was conducted primarily in a Caucasian population. Asian patients with type 2 diabetes have a relatively lower body mass index (BMI) relative to Caucasian patients. Therefore, the effects of SGLT-2 inhibitors should be investigated in patients with lower BMI.
Objectives
We aim to conduct a prospective, multicentre, blinded-endpoint phase IV randomised controlled study (PRIME-V study) to evaluate the safety and efficacy of a 24-week treatment with either an SGLT-2 inhibitor (ipragliflozin) or metformin for reducing visceral fat and plasma glucose levels in Asian patients with type 2 diabetes (BMI >22 kg/m2) undergoing treatment with the DPP-4 inhibitor, sitagliptin (50 mg daily), for poor glycaemic control. CT will be used to measure visceral fat at the level of the fourth lumbar vertebra. We will also evaluate the effects of each treatment on other metabolic parameters, such as body weight, BMI, blood pressure, cholesterol level, waist circumference, bone mineral density, muscle strength, muscle mass and basal metabolism as secondary endpoints.
Methods and analysis
Study design
The PRIME-V study is designed and independently conducted by Chiba University. The trial organisation and a complete list of investigators are provided in the online supplementary appendix file 1. The ethics committee at each participating trial site approved the protocol and consent form. The study will be conducted in full compliance with the articles of the Declaration of Helsinki. All analyses will be conducted by Chiba University, independent of the sponsor, according to the prespecified statistical analysis plan. The first and second authors wrote the first draft of the manuscript. Executive committee members, coauthors and the sponsor will review the data, revise the manuscript, and assume responsibility for trial adherence to the protocol and the accuracy and completeness of the data and analyses. The Standard Protocol Items: Recommendations for Interventional trials (SPIRIT checklist) was followed in designing the study protocol (see online supplementary appendix 2).
bmjopen-2016-015766supp001.pdf (277.4KB, pdf)
Sample size calculation
A total sample size of 106 patients will be required, based on the results of a previous analysis,15 which reported that SGLT-2 inhibitor and metformin treatments resulted in a 4.0 kg and a 1.3 kg reduction in body weight, respectively. We calculated that ipragliflozin and metformin treatments produce a 20% and 3% reduction in visceral fat, respectively. Assuming a group difference of 17% (SD=24.9%), allocating 47 patients per group will provide >90% power to detect a difference in the rate of visceral fat reduction between ipragliflozin and metformin treatment using a two-sided, two-sample t-test at a 5% level of significance. To allow for a 10% dropout rate, 53 participants are required per group, resulting in a total of 106 participants in the study.
Recruitment and consent
From September 2014 to September 2016, 106 participants were recruited. Participants are currently undergoing follow-up observation; the last patient visit is scheduled in April 2017. This study is being conducted at 20 hospitals in Japan. All enrolled patients provided written informed consent.
Eligibility criteria
Inclusion criteria
Eligible patients are those who meet the following inclusion criteria: (1) diagnosis of type 2 diabetes, confirmed in accordance with Japanese guidelines16; (2) age between 20 and 75 years; (3) inadequate control of plasma glucose levels despite treatment with 50 mg of the DPP-4 inhibitor sitagliptin for >12 weeks; (4) glycosylated haemoglobin (HbA1c, which provides an indication of the average blood glucose concentration of a patient over the previous 3 months) level >7.0% or <10.0% (according to the National Glycohemoglobin Standardization Program (NGSP)); (5) BMI >22 kg/m2; (6) estimated glomerular filtration rate >50 mL/min/1.73 m2; and (7) an adequate understanding of the contents of the trial and provision of written informed consent.
Exclusion criteria
Patients meeting any of the following criteria will be excluded from the trial: (1) diagnosis of type 1 diabetes; (2) history of metabolic acidosis, diabetic coma and/or precoma up to 6 months prior to providing consent; (3) history of serious infections requiring insulin treatment, prior/upcoming surgeries and/or severe injuries; (4) considerable loss of kidney function (blood creatinine level >1.3 mg/dL in men or >1.2 mg/dL in women) and/or need for dialysis (including peritoneal dialysis); (5) serious liver damage; (6) history of stroke, myocardial infarction, heart failure or other severe cardiovascular complications requiring hospitalisation; (7) use of oral hypoglycaemic agents other than DPP-4 inhibitors at the start of the trial; (8) pregnancy, nursing or plans to become pregnant; (9) history of chemical sensitivity to DPP-4 inhibitors, SGLT-2 inhibitors and/or metformin; (10) current diagnosis of, or at risk for, urinary tract infection and/or dehydration; (11) positive for ketone bodies; (12) history of lactic acidosis; (13) excessive alcohol consumption; (14) history of bone fracture caused by osteoporosis; (15) need for CT scan within 3 months prior to providing written consent; and/or (16) determination of ineligibility by the attending physician for any other reason.
Study setting
The community clinics and academic hospitals in Japan that were involved with this study are mentioned in the online supplementary appendix file 1. Each clinical centre involved in this study was chosen based on patient availability.
Random allocation and study medication
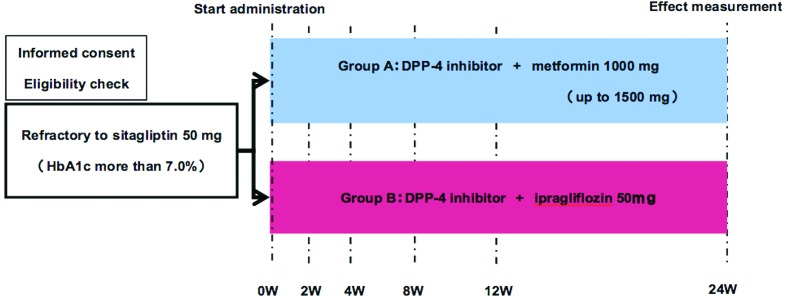
The investigators will send a registration form for an eligible patient to the registration centre at the Chiba University Clinical Trial Data Center (via fax). Registration and allocation will be implemented at the registration centre. Eligible patients who provide written informed consent will be randomised to treatment with either ipragliflozin (50 mg daily) or metformin (1000–1500 mg daily) at a ratio of 1:1 by a computer program located at the registration centre using a minimisation method with biased coin assignment balancing age (≤65 or >65 years old), HbA1c level (≤8.0 or >8.0%) and waist circumference (men: ≤85 or >85 cm; women: ≤80 or >80 cm) at the time of screening (figure 1).
Figure 1.
Schematic depiction of the trial design. Eligible participants are randomly assigned to a 24-week treatment regimen with either ipragliflozin (50 mg daily) or metformin (1000 mg daily, up to 1500 mg). DPP-4, dipeptidyl peptidase-4; HbA1c, glycosylated haemoglobin.
Visceral fat CT measurement
CT was used to measure the visceral, subcutaneous and total fat areas. The CT images are measured as the central measurement by two blind radiologists and the average value is calculated. The following imaging conditions will be used at all sites and for all participants: unified CT imaging, conventional method, voltage 120 kVp, dose 200 mAs, abdominal simple image reconstruction condition, field of view of 500 mm, expiratory phase end position for respiratory phase and at the fourth lumbar spine centre level. The imaging position is the same in all the periods. To minimise exposure to radiation by positioning with scouts, the number of images obtained should be as minimal as possible. Slice width was preferably 10 mm, or 8 mm if there are equipment restrictions. For facilities with multiple CT devices, one particular CT device was used for this study.
Blinding
Participating sites will send electronic imaging data saved using the the Digital Imaging and Communication in Medicine method to the contracted research organisation (Micron Technology, Tokyo, Japan). Micron Technology will then mask patients’ personal information (ie, age, sex, facility and date of CT scan) and send the converted data to the two radiologists. The radiologists will remain blinded to the clinical information and perform centralised analysis of the images in a unified measurement condition. FatScan (East Japan Institute of Technology, Ibaraki, Japan) will be used to measure the visceral, subcutaneous and total fat areas, waist circumference, CT level (bone density) of the fourth lumbar vertebra, and cross-sectional area of abdominal muscle. The average values for the above measurements will then be calculated.
Interventions
Ipragliflozin or metformin will be administered for 24 weeks. The study medication will be initiated on day 0 after the first CT scan. The metformin dose will be increased to 1000 mg daily at 2–4 weeks if the patient does not experience adverse gastroenterological effects. The metformin dose will also be increased to 1500 mg daily at 12 weeks if the HbA1c value is ≥7.4% or ≥6.9% for patients with day 0 HbA1c values ≥8.0% or <8.0%, respectively.
Treatment adherence
To evaluate treatment adherence, the investigators will ask patients regarding the frequency of medication use during each visit.
Concomitant medication
Use of additional drugs or therapies (ie, antidiabetic agents other than sitagliptin, ipragliflozin or metformin; antiobesity medications, such as mazindol, cetilistat or bofu-tsusho-san; and other drugs, such as mosapride, ephedrine or citric acid supplements) will not be permitted during the study period. Patients will be instructed not to alter their diet and exercise programmes during the study. The use of anticoagulants, antihypertensive agents, antidyslipidaemia agents and diuretics will be permitted. However, alterations in medication dose and initiation/termination should be avoided when possible.
Outcomes
The rate of change in the total area of visceral fat in each group, as measured via CT following the 24-week treatment period, was regarded as the primary outcome. Secondary outcomes included the rates of change in (1) HbA1c (NGSP); (2) body weight and BMI; (3) waist circumference; (4) bone markers (alkaline phosphatase, bone alkaline phosphatase (BAP) and tartrate-resistant acid phosphatase-5b (TRACP5b)); (5) muscle strength; (6) fasting plasma glucose level, homeostatic model assessment (HOMA)-b and HOMA-R; (7) cholesterol level (total cholesterol, low-density lipoprotein cholesterol as calculated using the Friedewald equation, fasting triglycerides, high-density lipoprotein cholesterol); (8) blood pressure; (9) adipocytokine (adiponectin) and inflammatory marker (high-sensitivity C-reactive protein (hs-CRP)); (10) subcutaneous fat area and total fat area; (11) respiratory quotient, basal metabolism, whole-body dual-energy X-ray absorption (DXA), eating behaviour questionnaire, and calorie and glucose intake; (12) area of abdominal muscle as measured via CT; and (13) bone density in the fourth lumbar vertebra as measured via CT. Levels of BAP, TRACP5b, insulin, adipocytokine (adiponectin), inflammatory markers (hs-CRP) and α1-microglobulin will be measured at a central laboratory (LSI Medience Corporation, Tokyo, Japan).
Total body composition will be determined by whole-body DXA using a fan beam bone densitometer (Discovery DXA system; Hologic, Marlborough, Massachusetts), and all the scans will be analysed using Discovery software V.13.3.0.1 (Hologic), which contains the Hologic Advanced Body Composition assessment and InnerCore visceral adipose tissue assessment. Two certified technologists perform all the scans.
Serious adverse events (AEs) will be documented and reported per regulatory requirements.
Data collection
Study visits and examinations
The schedule for the study visits and data collection is summarised in table 1.
Table 1.
Schedule of data collection
| Before observation period | Start of administration | Dosing period | |||||
| Within 4 weeks | Day 0 | 2 weeks | 4 weeks | 8 weeks | 12 weeks | 24 weeks | |
|---|---|---|---|---|---|---|---|
| Allowance | Within ±1 week | Within ±1 week | Within ±2 weeks | Within ±2 weeks | Within ±4 weeks | ||
| Visit | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| Informed consent | X | ||||||
| Patient characteristics | X | ||||||
| Study drug administration |
 X X 
|
||||||
| Symptom check |
 X X 
|
||||||
| Adverse events check |
 X X 
|
||||||
| Visceral fat area measured via CT | X | X | |||||
| Body weight | X | X | X | X | X | X | X |
| Heart rate, blood pressure | X | X | X | X | X | X | |
| Blood tests | X | X | X | X | X | ||
| Blood chemistry | X | X | X | X | X | ||
| Urine tests | X | X | X | X | X | X | |
| Insulin, bone marker, inflammation marker | X | X | X | ||||
| α1-Microglobulin | X | X | |||||
| Adipocytokine | X | X | |||||
| Waist circumference | X | X | X | X | X | X | X |
| Hand griping test | X | X | X | ||||
| Medication adherence check | X | X | X | X | X | ||
| Special examination* | X | X | |||||
| Screening blood examination | X | ||||||
*Special examination includes whole-body DXA, dietary behaviour questionnaire, respiratory quotient, basal metabolism, and calorie and glucose intake for patients.
DXA, dual-energy X-ray absorption.
Data management, monitoring and auditing
The investigators (or their delegates) will maintain individual records for each patient as source data, which will include a log of informed consent, medical records, laboratory data and other records or notes, as appropriate. All entries in the case report form (CRF) must be backed up by the relevant source data. CRFs must be completed in a timely manner.
All data will be collected by the independent data management centre. There will be no direct communication between investigators and the coordinating data centre. The clinical data entry (double data entry), coding, data management and reporting will be performed using the data management system ACReSS (Fujitsu, Tokyo, Japan).
A monitor will confirm that the investigational team is adhering to the protocol, data are being accurately recorded in CRFs, AEs have been properly documented on CRFs, severe AEs (SAEs) have been forwarded to the coordinating investigator and the provider of the investigational product, and the SAEs that met the criteria for reporting have been forwarded to the Institutional Review Board (IRB). An interim analysis will not be performed.
The study may be audited or inspected by a third party (Increase, Tokyo, Japan). In case of an audit, the investigators must provide study documentation to the auditor. If an audit or inspection occurs, the investigators at the study site must discuss the findings and any relevant issues.
Adverse events
Investigators must record all AEs in the patients’ CRFs. All AEs are to be followed up continually during their course until the end of the trial. All SAEs must be reported to all investigators and discussed.
Statistical analysis
The analyses of the primary and secondary efficacy endpoints will be performed using the full analysis set. Safety analysis will be conducted in the safety analysis population. For the baseline variables, summary statistics will be constructed using frequencies and proportions for categorical data, and means and SDs for continuous variables. Patient characteristics will be compared using Pearson’s χ2 test or Fisher’s exact test for categorical outcomes, and Student’s t-test for continuous variables, as appropriate.
For the primary analysis to evaluate treatment efficacy, the least square mean difference in the rate of visceral fat reduction between ipragliflozin and metformin treatment at week 24 and its 95% CI will be estimated using an analysis of covariance model adjusted for allocation factors (ie, age, HbA1c and abdominal circumference). As a sensitivity analysis, a mixed-effects model for repeated measures, the last observational carried forward method and the multiple imputation method will be applied to examine the effect of missing data. The secondary analysis will be performed in the same manner as the primary analysis. Data regarding hypoglycaemia, dehydration, urinary tract infection, drug eruption and other AEs will be evaluated during the safety analysis. The frequencies of AEs will be compared using Fisher’s exact test. A subgroup analysis based on patient characteristics (ie, diabetes duration, drug combinations, age and BMI) will be performed to investigate the mechanisms underlying patient responses to ipragliflozin.
All comparisons have been planned, and all p values will be two-sided. P values <0.05 will be considered statistically significant. All statistical analyses will be performed using SAS V.9.4. This plan for statistical analysis was developed by the chief investigator and statisticians at Chiba University, and will be finalised prior to database lock.
Ethics and dissemination
Research ethics approval and protocol amendments
The study protocol was approved by the following IRBs: Institutional Review Board of Chiba University Hospital (ID number: G26009), Asahi General Hospital Ethics Review Committee (ID number: 2014091602), National Hospital Organization Chiba Medical Center Research Review Board, Seirei Sakura Citizen Hospital Ethics Committee, Chiba Rosai Hospital Ethics Committee (ID number: 26–21), Toho University Sakura Medical Center Ethics Committee (ID number: 2014–077), Tokyo Women’s Medical University Yachiyo Medical Center Ethics Committee (ID number: 1 50 303), Chiba Aoba Municipal Hospital Ethics Review Committee, Kimitsu Chuo Hospital Ethics Committee, Funabashi Central Hospital Ethics Committee (ID number: H27-1) and Chiba Kaihin Municipal Hospital Ethics Review Committee. Other facilities were judged at the Institutional Review Board of Chiba University Hospital, which was the centralised IRB. Substantial amendments of the study protocol must be approved by the IRBs. The study was registered in the University hospital Medical Information Network (UMIN) Clinical Trials Registry (UMIN000015170).
Informed consent
All participants will receive adequate information about the nature, purpose, possible risks and benefits of the trial, and alternative therapeutic choices using an informed consent protocol approved by the IRB. All participants must be given ample time and opportunity to ask questions and consider participation in the trial. A completed informed consent form is required for enrolment in the trial. The investigators must maintain the original signed consent form, as well as an additional copy of this form.
If the blood and/or the urine specimens to be stored are to be used for another research in the future, a new research plan should be prepared and sent to IRB for approval prior to study commencement. Samples will be discarded anonymously.
Confidentiality
To ensure confidentiality, trial participants will be allocated a unique trial identification number for use throughout the trial.
Dissemination
The findings of this trial will be disseminated via peer-reviewed publications and conference presentations, and will also be disseminated to participants. The principal investigator and other investigators will publish the results of the clinical study.
Discussion
In this study, we evaluated the safety and efficacy of 24 weeks of treatment with either an SGLT-2 inhibitor (ipragliflozin) or metformin for reducing visceral fat and plasma glucose levels in Asian patients with type 2 diabetes (BMI >22 kg/m2) undergoing treatment with the DPP-4 inhibitor, sitagliptin (50 mg daily), for poor glycaemic control. We also evaluated the effects of each treatment on other metabolic parameters. Studies regarding the effects of SGLT-2 inhibitors and metformin on visceral fat reduction in patients with type 2 diabetes receiving first-line treatment with DPP-4 inhibitors are limited; therefore, the design of the present study provides a unique opportunity to examine alternative treatment strategies in an Asian population. Another strength of this study is the blind measurement of visceral fat by CT.
Clinicians must remain conscious about weight gain following increases in insulin secretion when treating patients with type 2 diabetes. Metformin allows for reductions in plasma glucose levels without affecting insulin secretion by pancreatic beta cells. In addition to promoting uptake in peripheral tissues (mainly muscle) and improving insulin sensitivity, metformin is associated with a low risk of body weight gain. Previous researchers have further revealed that combined treatment with metformin and a DPP-4 inhibitor leads to significant reductions in body weight.17 Therefore, metformin may be an effective second-line treatment option in patients with symptoms refractory to treatment with DPP-4 inhibitors. However, metformin has been known to induce gastrointestinal disturbances and severe lactic acidosis in some patients. Furthermore, the need to take medication two to three times per day often results in poor medication adherence.
Similarly, SGLT-2 inhibitors do not affect insulin secretion. SGLT-2 inhibitors act to reduce glucose reabsorption in the kidneys, thereby preventing increases in blood glucose levels, reducing the burden of pancreatic beta cells, restoring insulin secretion and improving glucose toxicity and insulin resistance.8 In clinical studies, it has been reported that treatment with SGLT-2 is associated with improvements in insulin sensitivity18 and reductions in body weight.19 20 In one clinical study, combined treatment with dapagliflozin and metformin produced significant reductions in visceral fat.10 These findings indicate that such treatment may aid in lowering the risk of several conditions associated with high levels of visceral fat, such as arteriosclerosis. Furthermore, once-daily drug administration is sufficient, which may increase medication adherence.
In the Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes (EMPA-REG OUTCOME) study, empagliflozin exerts cardioprotective effects.11 Therefore, our findings may provide further evidence regarding the cardioprotective effects of SGLT-2 inhibitors.
Further studies have revealed that adjunct treatment with dapagliflozin in patients with symptoms refractory to DPP-4 inhibitor treatment resulted in HbA1c reductions of 0.5% and body weight reductions of 2.1 kg.21 In a comparative study of a single treatment with either empagliflozin or metformin, metformin treatment resulted in HbA1c reductions of 0.56% and body weight reductions of 1.3 kg at 90 weeks after administration, while empagliflozin treatment resulted in HbA1c reductions of 0.63% and body weight reductions of 4.0 kg.15 In a comparative study of single treatment with either ipragliflozin (50 mg) or metformin (up to 1500 mg), no significant differences in HbA1c were observed at 12 weeks, although ipragliflozin treatment resulted in body weight reductions of 0.78 kg.22 Based on these previous findings, we speculate that combined treatment with an SGLT-2 inhibitor and a DPP-4 inhibitor results in comparable reductions in blood glucose level and a greater visceral fat reduction than combined treatment with metformin and a DPP-4 inhibitor. Previous researchers have provided a strong rationale for dual therapy with a DPP-4 inhibitor and an SGLT-2 inhibitor.23 This study aims to provide new insight on the most appropriate combination of DPP-4 and SGLT-2 inhibitors, which may lead to the development of new treatment options for patients with type 2 diabetes.
Although reductions in visceral fat are important for reducing the impact of metabolic disorders and preventing complications, such as atherosclerosis, there are currently no studies that have been conducted to compare the effects of SGLT-2 inhibitors and metformin on visceral fat reduction in patients taking DPP-4 inhibitors. The administration of SGLT-2 inhibitors, particularly in patients with poor glycaemic control despite treatment with DPP-4 inhibitors, may exert such beneficial effects. However, the risk of sarcopenia and osteopaenia remains a concern. Therefore, it is necessary to clarify specific changes in body composition, rather than reductions in body weight alone, to evaluate such risks. Our study will provide evidence regarding the safety and efficacy of the SGLT-2 inhibitor ipragliflozin as a second-line treatment for reducing visceral fat and blood glucose levels in patients with type 2 diabetes.
bmjopen-2016-015766supp002.pdf (114.6KB, pdf)
Supplementary Material
Acknowledgments
The authors thank the staff and patients participating in the present study. Staff members include Mayumi Negishi, Mayumi Ogawa, Mayumi Matsui, Chisato Ishii, Yoko Ohno, Kengo Kamata, Yumi Yamada, Takatoshi Sato, Syoko Ogawa, Nobuko Yamaguchi and David Reed from Chiba University; Yukie Sakuma from Asahi General Hospital; Saki Hashidume and Ayaka Fujino from Kimitsu Chuo Hospital; Fumie Kawano and Yoshie Iida from National Hospital Organization Chiba Medical Center and Tomoko Murakami from Tokyo Women’s Medical University Yachiyo Medical Center. We also thank Editage (www.editage.jp) for English language editing.
Footnotes
Contributors: All authors made a significant contribution to the conception and design of the study protocol. KY designed the original concept. The protocol was written by MK, KI, TI, KK and MT, and it was critically reviewed by TH, RS, ST, KN, YS, IT, TT, NH, NK, DU, and KY. All authors provided approval for the publication of the manuscript.
Funding: To conduct this study, an agreement was signed between Chiba University and Astellas Pharma (Tokyo, Japan). This work was funded by Astellas Pharma.
Competing interests: KY received research grants from Astellas Pharma and MSD. KK received a lecture fee from Astellas Pharma and Sumitomo Dainippon Pharma (Tokyo, Japan). No conflicts of interest are declared for other authors.
Ethics approval: The protocol was approved by the Institutional Review Board of each participating hospital.
Provenance and peer review: Not commissioned; externally peer reviewed.
Collaborators: Collaborators of PRIME-V Study Investigators include Asahi General Hospital; Chiba Aoba Municipal Hospital; Chiba Chuo Geka Naika; Chiba Kaihin Municipal Hospital; Chiba Rosai Hospital; Chiba University Hospital; Funabashi Central Hospital; Funabashi Municipal Medical Center; Hotaruno Central Naika; Inage Hospital; Izumi Chuo Hospital; Kimitsu Chuo Hospital; National Hospital Organization Chiba Medical Center; Kujyukuri Home Hospital; Kouyukai Memorial Hospital; Seirei Sakura Citizen Hospital; Sousa Citizen Hospital; Tamura Memorial Hospital; Toho University Sakura Medical Center; Tokyo Womens Medical University Yachiyo Medical Center.
Contributor Information
Collaborators: PRIME-V Study Investigators, Hidetaka Yoko, Shunichiro Onishi, Tomohiko Yoshida, Kyohei Yamamoto, Hanna Deguchi, Tomohiro Ohno, Akina Kobayashi, Kaneyuki Watanabe, Masahiro Mimura, Kouichiro Nemoto, Emi Tsuchiya, Yukari Maeda, Kenichi Sakamoto, Masaya Yamaga, Mayumi Shoji, Akiko Hattori, Shintaro Ide, Kana Ide, Yoshiro Maezawa, Hideaki Iwaoka, Tatsushi Shimoyama, Syunsyuke Nakamura, Susumu Nakamura, Harukiyo Kawamura, Ryouichi Ishibashi, Tomoko Takiguchi, Kenji Takeda, Norio Shimada, Hirotake Tokuyama, Tetsuya Okazaki, Kenchi Yui, Emi Ohara, Yusuke Baba, Atsuto Saiki, Yasuhiro Watanabe, Takahiko Tokuyama, Jun Ogino, Chihiro Yoneda, Kana Tajima, Mayumi Negishi, Mayumi Ogawa, Mayumi Matsui, Chisato Ishii, Yoko Ohno, Kengo Kamata, Yumi Yamada, Takatoshi Sato, Syoko Ogawa, Nobuko Yamaguchi, David Reed, Yukie Sakuma, Saki Hashidume, Ayaka Fujino, Fumie Kawano, Yoshie Iida, and Tomoko Murakami
References
- 1. King H, Aubert RE, Herman WH. Global burden of diabetes, 1995-2025: prevalence, numerical estimates, and projections. Diabetes Care 1998;21:1414–31. 10.2337/diacare.21.9.1414 [DOI] [PubMed] [Google Scholar]
- 2. Whiting DR, Guariguata L, Weil C, et al. . IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract 2011;94:311–21. 10.1016/j.diabres.2011.10.029 [DOI] [PubMed] [Google Scholar]
- 3. Seino Y, Kuwata H, Yabe D. Incretin-based drugs for type 2 diabetes: focus on east Asian perspectives. J Diabetes Investig 2016;7(Suppl 1):102–9. 10.1111/jdi.12490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sone H, Yoshimura Y, Ito H, et al. . Japan diabetes complications study G: energy intake and obesity in japanese patients with type 2 diabetes. Lancet 2004;363:248–9. [DOI] [PubMed] [Google Scholar]
- 5. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363:157–63. 10.1016/S0140-6736(03)15268-3 [DOI] [PubMed] [Google Scholar]
- 6. Sone H, Ito H, Ohashi Y, et al. . Japan diabetes complication study G: obesity and type 2 diabetes in japanese patients. Lancet 2003;361:85. [DOI] [PubMed] [Google Scholar]
- 7. Lipska KJ, Yao X, Herrin J, et al. . Trends in drug utilization, glycemic control, and rates of severe hypoglycemia, 2006-2013. Diabetes Care 2017;40:468–75. 10.2337/dc16-0985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Washburn WN, Poucher SM. Differentiating sodium-glucose co-transporter-2 inhibitors in development for the treatment of type 2 diabetes mellitus. Expert Opin Investig Drugs 2013;22:463–86. 10.1517/13543784.2013.774372 [DOI] [PubMed] [Google Scholar]
- 9. Roden M, Weng J, Eilbracht J, et al. . Empagliflozin monotherapy with sitagliptin as an active comparator in patients with type 2 diabetes: a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Diabetes Endocrinol 2013;1:208–19. 10.1016/S2213-8587(13)70084-6 [DOI] [PubMed] [Google Scholar]
- 10. Bolinder J, Ljunggren Ö, Kullberg J, et al. . Effects of dapagliflozin on body weight, total fat mass, and regional adipose tissue distribution in patients with type 2 diabetes mellitus with inadequate glycemic control on metformin. J Clin Endocrinol Metab 2012;97:1020–31. 10.1210/jc.2011-2260 [DOI] [PubMed] [Google Scholar]
- 11. Zinman B, Wanner C, Lachin JM, et al. . Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 2015;373:2117–28. 10.1056/NEJMoa1504720 [DOI] [PubMed] [Google Scholar]
- 12. Watts NB, Bilezikian JP, Usiskin K, et al. . Effects of canagliflozin on fracture risk in patients with type 2 diabetes mellitus. J Clin Endocrinol Metab 2016;101:157–66. 10.1210/jc.2015-3167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fox CS, Massaro JM, Hoffmann U, et al. . Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham heart study. Circulation 2007;116:39–48. 10.1161/CIRCULATIONAHA.106.675355 [DOI] [PubMed] [Google Scholar]
- 14. Muramoto A, Matsushita M, Kato A, et al. . Three percent weight reduction is the minimum requirement to improve health hazards in obese and overweight people in Japan. Obes Res Clin Pract 2014;8:e466–75. 10.1016/j.orcp.2013.10.003 [DOI] [PubMed] [Google Scholar]
- 15. Ferrannini E, Berk A, Hantel S, et al. . Long-term safety and efficacy of empagliflozin, sitagliptin, and metformin: an active-controlled, parallel-group, randomized, 78-week open-label extension study in patients with type 2 diabetes. Diabetes Care 2013;36:4015–21. 10.2337/dc13-0663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. The Japanese Diabetes Society. Treatment guide for diabetes 2014-2015. Japan: BUNKODO, 2014. [Google Scholar]
- 17. Velija-Asimi Z, Izetbegovic S, Karamehic J, et al. . The effects of dipeptidyl peptidase-4 inhibitors in treatment of obese patients with type 2 diabetes. Med Arch 2013;67:365–7. 10.5455/medarh.2013.67.365-367 [DOI] [PubMed] [Google Scholar]
- 18. Kurosaki E, Ogasawara H. Ipragliflozin and other sodium-glucose cotransporter-2 (SGLT2) inhibitors in the treatment of type 2 diabetes: preclinical and clinical data. Pharmacol Ther 2013;139:51–9. 10.1016/j.pharmthera.2013.04.003 [DOI] [PubMed] [Google Scholar]
- 19. Kashiwagi A, Kazuta K, Yoshida S, et al. . Randomized, placebo-controlled, double-blind glycemic control trial of novel sodium-dependent glucose cotransporter 2 inhibitor ipragliflozin in Japanese patients with type 2 diabetes mellitus. J Diabetes Investig 2014;5:382–91. 10.1111/jdi.12156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kashiwagi A, Kazuta K, Takinami Y, et al. . Ipragliflozin improves glycemic control in Japanese patients with type 2 diabetes mellitus: the BRIGHTEN study. Diabetol Int 2015;6:8–18. 10.1007/s13340-014-0164-0 [DOI] [Google Scholar]
- 21. Jabbour SA, Hardy E, Sugg J, et al. . Dapagliflozin is effective as add-on therapy to sitagliptin with or without metformin: a 24-week, multicenter, randomized, double-blind, placebo-controlled study. Diabetes Care 2014;37:740–50. 10.2337/dc13-0467 [DOI] [PubMed] [Google Scholar]
- 22. Fonseca VA, Ferrannini E, Wilding JP, et al. . Active- and placebo-controlled dose-finding study to assess the efficacy, safety, and tolerability of multiple doses of ipragliflozin in patients with type 2 diabetes mellitus. J Diabetes Complications 2013;27:268–73. 10.1016/j.jdiacomp.2012.11.005 [DOI] [PubMed] [Google Scholar]
- 23. Scheen AJ. DPP-4 inhibitor plus SGLT-2 inhibitor as combination therapy for type 2 diabetes: from rationale to clinical aspects. Expert Opin Drug Metab Toxicol 2016;12:1407–17. 10.1080/17425255.2016.1215427 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2016-015766supp001.pdf (277.4KB, pdf)
bmjopen-2016-015766supp002.pdf (114.6KB, pdf)