Abstract
Objectives
Studies in western healthcare settings suggest that preoperative anaemia is associated with poor outcomes after elective orthopaedic surgery. We investigated the prevalence of preoperative anaemia among patients with primary unilateral total knee arthroplasty (TKA) in Singapore and its association with length of hospital stay (LOS), perioperative blood transfusion and hospital readmission rates.
Methods
Retrospective cohort study performed in a tertiary academic medical centre in Singapore, involving patients who underwent primary unilateral TKA between January 2013 and June 2014. Demographics, comorbidities, preoperative haemoglobin (Hb) level, LOS and 30-day readmission data were collected. Anaemia was classified according to WHO definition. Prolonged LOS was defined as more than 6 days, which corresponds to >75th centile LOS of the data.
Results
We analysed 2394 patients. The prevalence of anaemia was 23.7%. 403 patients (16.8%) had mild anaemia and 164 patients (6.8%) had moderate to severe anaemia. Overall mean LOS was 5.4±4.8 days. Based on multivariate logistic regression, preoperative anaemia significantly increased LOS (mild anaemia, adjusted OR (aOR) 1.71, p<0.001; moderate/severe anaemia, aOR 2.29, p<0.001). Similar effects were seen when preoperative anaemia was defined by Hb level below 13 g/dL, regardless of gender. Transfusion proportionately increased prolonged LOS (1 unit: aOR 2.12, p=0.006; 2 or more units: aOR 6.71, p<0.001). Repeat operation during hospital stay, previous cerebrovascular accidents, general anaesthesia and age >70 years were associated with prolonged LOS. Our 30-day related readmission rate was 1.7% (42) cases.
Conclusion
Anaemia is common among patients undergoing elective TKA in Singapore and is independently associated with prolonged LOS and increased perioperative blood transfusion. We suggest measures to correct anaemia prior to surgery, including the use of non-gender-based Hb cut-off for establishing diagnosis.
Keywords: Anaemia; Arthroplasty, knee replacement; length of stay; perioperative blood transfusion, patient blood management
Strengths and limitations of this study.
Our study provides a unique perspective from a South East Asian healthcare system on anaemia and its impact on length of stay (LOS) and hospital readmission rates after unilateral, primary total knee arthroplasty.
We had minimal incomplete data (2.0%) due to the rigorous mandatory preoperative assessment database.
We found comparable adjusted OR of prolonged LOS using the WHO gender-based definition of anaemia, which defines mild anaemia in men to be haemoglobin (Hb) concentration between 11.0 g/dL and 12.9 g/dL and in women to be between 11.0 g/dL and 11.9 g/dL, and a non-gender-based definition that defines mild anaemia as Hb 11.0–12.9 g/dL for both genders. Therefore, this lends weight to the recent proposition for a non-gender-based cut-off of <13.0 g/dL in defining preoperative anaemia.
Our study is one of the first to control for the day of the week the surgery was done, which was recently found to be a significant predictor for LOS in arthroplasties.
This is a retrospective observational study, so it cannot establish a causal relationship between preoperative anaemia and adverse outcomes.
The selection of the 75th centile for defining prolonged LOS can be viewed as an arbitrary cut-off, although it is also used in other literature examining LOS after elective surgery.
Introduction
The prevalence of preoperative anaemia in patients undergoing non-cardiac surgery is considerably high, with rates of 30.4% and 28.7% recorded in the USA and Europe, respectively.1 This is an important health problem as even mild anaemia is associated with poor outcomes postsurgery,1–5 including prolonged length of hospital stay (LOS) and higher readmission rates.6 7
Total knee arthroplasty (TKA) is one of the most common orthopaedic procedures worldwide.2 8 Due to the low mortality and morbidity rates associated with TKA, improvement initiatives have mainly focused on reducing LOS and improving functional recovery after surgery.3 4 LOS associated with TKA is directly correlated with the total procedure cost, mainly due to provision of inpatient services.5 6 Reductions in LOS can therefore help to reduce the economic burden of TKA.7 9 Due to the fixed bed capacity, high overhead costs and the Diagnosis-Related Group reimbursement system in most health systems, the economic revenue of these systems depends on an increase in patient throughput by decreasing LOS. Additionally, unexpected prolonged LOS could negatively impact the patient’s perspective of a good surgical outcome. Hence, it is important for health systems and physicians to identify modifiable risk factors that are associated with the improved recovery and discharge of these patients. Most studies examining the association between hospital LOS after joint arthroplasties and preoperative anaemia10–17 were conducted within the western healthcare settings, with different demographics, potentially diverse discharge and rehabilitation policies from other regions in the world.
Therefore, in this study, we set out to investigate the relationship between preoperative anaemia and hospital LOS, perioperative blood transfusion as well as 30-day readmission rate among patients undergoing primary unilateral TKA in Singapore.
Methods
Institutional Review Board approval was obtained (Singhealth CIRB 2014/651/D) prior to the start of the study. The electronic medical records of all 2676 patients who underwent TKA between January 2013 and June 2014 in our institution were analysed. These clinical records were sourced from our institution's clinical information system (Sunrise Clinical Manager (SCM), Allscripts, Illinois, USA) and stored in our enterprise data repository and analytics system (SingHealth-IHiS Electronic Health Intelligence System), which integrates information from administration, clinical and ancillary healthcare systems. We generated a list of patients who underwent total knee replacements from January 2013 to June 2014 using specific surgical codes relevant to this surgery. Information from SCM included patient demographics, preoperative comorbidities such as smoking, haemoglobin (Hb) level, individual components of the Revised Risk Cardiac Index (RCRI),18 19 such as a history of previous cerebrovascular accidents (CVAs), ischaemic heart disease (IHD), congestive cardiac failure (CCF), diabetes mellitus (DM) on insulin and elevated preoperative creatinine level >2 mg/dL; American Society of Anesthesiologist Physical Status (ASA-PS) score20; details of the operation such as site, duration, type of anaesthesia and day of week the surgery was done21; and perioperative blood transfusion and repeat surgeries during hospital stay were also obtained. The LOS was calculated from the date of admission to the date of discharge from hospital to their home environment. Thirty-day readmission data after discharge was obtained from the clinical information system database, SCM. We filtered related readmission by the International Classification of Diseases (10th revision) diagnosis and further confirmed the cause of admission by looking up the patient’s electronic medical records. We defined the window for preoperative Hb levels to be taken at a maximum of 14 days and a minimum of 1 day before the surgery. We also defined perioperative blood transfusion to be within 2 weeks before up to 2 weeks after the date of surgery.
In our institution, most patients are admitted on the day of surgery and very infrequently, 1 day earlier for medical and/or social reasons. Routinely, all antiplatelet medications apart from aspirin are stopped for the recommended duration before the surgery. The use of intraoperative tranexamic acid infiltration to the knee joint, intravenous tranexamic acid and the placement of a drain into the joint after the surgery is not standardised. Use of cell salvage is rare. Postoperatively, all patients receive a standard hospital TKA protocol for postoperative care and discharge. This includes thromboembolism chemoprophylaxis with 40 mg once daily subcutaneous low molecular weight heparin (Clexane, Sanofi, Paris, France) on the first postoperative day, which is discontinued on discharge. Patients also receive routine physiotherapy starting from the first postoperative day, even if it falls on the weekend. They are deemed fit for discharge when there is an agreement between the surgeon and physiotherapist that the patient is medically stable and that their functional ability is sufficient to allow discharge to their home environment. This includes being able to climb up a few steps, transfer with the aid of a walking frame and to bend their operated knee close to 90°.
After excluding 51 patients with more than three missing variables, three patients who did not have preoperative Hb levels, 22 patients who underwent revision surgery and 206 patients who underwent bilateral surgery, we obtained 2394 patients in the final analysis (Figure 1). No sensitivity analysis accounting for the missing data was done due to the small number (2.0%).
Figure 1.
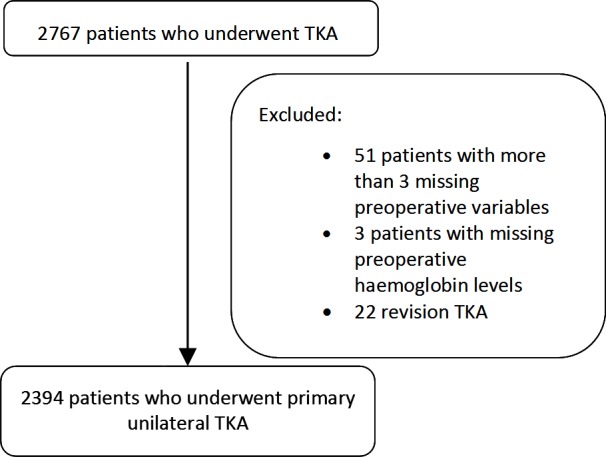
Flowchart showing derivation of study cohort
The primary outcome was prolonged LOS, defined as more than 6 days. This cut-off was selected as it represents >75th centile LOS of the whole sample. The use of 75th centile to define prolonged LOS is consistent with other studies.22 The secondary outcome was readmission for any reason within 30 days after surgery.
Statistical analysis
We used the WHO’s gender-based definition of anaemia severity.23 Thus, mild anaemia was defined as Hb concentration of 11–12.9 g/dL in males and 11–11.9 g/dL in females; moderate anaemia was defined for both genders to be Hb concentration between 8 and 10.9 g/dL and severe anaemia defined as Hb concentration <8.0 g/dL. Among the 567 patients (23.7%) with anaemia, 403 patients (16.8%) had mild preoperative anaemia, 159 patients (6.6%) had moderate anaemia and five patients had severe anaemia (0.2%). Due to the small incidence of severe anaemia in the sample, patients with moderate and severe anaemia were analysed together.
Patient demographics and clinical characteristics were compared between LOS >6 and <6 days (table 1). For continuous variables, mean and SD were presented, and Mann-Whitney U test was used to test the mean differences between the two groups. For categorical variables, χ2 test was used to compare the proportions between the two groups. We categorised continuous variable such as age according to their broad centile groups, body mass index (BMI) according to the WHO definition of obesity and operative duration according to ≤100 min or >100 min, which corresponds to >75th centile of the data. Multivariate logistic regression was performed to determine independent predictors for increased LOS (table 2) and perioperative blood transfusion (table 3) while adjusting for demographic, preoperative clinical risk factors and surgical factors. We repeated the logistic regression for LOS with non-gender based cut-offs for anaemia to see if it yielded significantly different results from the WHO definition of anaemia. No anaemia was defined as Hb ≥13.0 g/dL, mild anaemia as Hb 11.0–12.9 g/dL and moderate/severe anaemia as Hb <11.0 g/dL. Finally, we also constructed general linear model (GLM) with our data, taking LOS and Hb as continuous variables, to assess the effect size of every unit rise in Hb on LOS. We found little presence of collinearity between Hb level and perioperative blood transfusion and their effect on LOS based on linear regression. However, in our GLM, the addition of perioperative blood transfusion as a variable reduced the significance and effect size of preoperative Hb level, hence both models with and without perioperative blood transfusion were performed and presented. All analyses were performed using IBM SPSS Statistics V.21.
Table 1.
Demographics of patients with normal LOS (≤6 days) versus those with prolonged LOS (>6 days) after primary unilateral TKR
| Variable | LOS ≤6 days n=1933 |
LOS >6 days n=461 |
p Value | |
| Patient demographics | ||||
| Age: mean (SD) | 65.9 (8.0) | 69.2 (8.6) | <0.001 | |
| Race: n (%) | Chinese | 1628 (84.2) | 385 (83.5) | 0.02 |
| Malay | 148 (7.7) | 23 (5.0) | ||
| Indian | 106 (5.5) | 31 (6.7) | ||
| Others | 51 (2.6) | 22 (4.8) | ||
| Body mass index: n (%) | <25 | 555 (29.2) | 138 (31.8) | 0.16 |
| 25–29.9 | 812 (42.7) | 182 (41.9) | ||
| 30–34.9 | 410 (21.5) | 77 (17.7) | ||
| ≥35 | 126 (6.6) | 37 (8.5) | ||
| Gender: n (%) | Male | 477 (24.7) | 102 (22.1) | 0.25 |
| Female | 1456 (75.3) | 359 (77.9) | ||
| Details of operation | ||||
| Type of anaesthesia: n (%) | GA | 649 (33.6) | 184 (39.9) | 0.01 |
| RA | 1284 (66.4) | 277 (60.1) | ||
| Duration of operation: minutes (SD) | 79.6 (21.6) | 84.9 (27.5) | <0.001 | |
| Perioperative blood transfusion – n (%) | None | 1879 (97.2) | 394 (85.5) | <0.001 |
| one unit | 43 (2.2) | 37 (8.0) | ||
| ≥2 units | 11 (0.6) | 30 (6.5) | ||
| Repeat operation within hospital stay: n (%) | Yes | 1 (0.1) | 6 (1.3) | <0.001 |
| Day of week of operation: n (%) | Monday | 307 (15.9) | 90 (19.5) | <0.001 |
| Tuesday | 424 (21.9) | 119 (25.8) | ||
| Wednesday | 326 (16.9) | 84 (18.2) | ||
| Thursday | 472 (24.4) | 63 (13.7) | ||
| Friday | 301 (15.6) | 86 (18.7) | ||
| Saturday | 103 (5.3) | 19 (4.1) | ||
| Patient comorbidities | ||||
| Anaemia: n (%) | None | 1537 (79.5) | 290 (62.9) | <0.001 |
| Mild | 294 (15.2) | 109 (23.6) | ||
| Moderate/severe | 102 (5.3) | 62 (13.4) | ||
| DM on insulin: n (%) | Yes | 30 (1.6) | 11 (2.4) | 0.22 |
| Creatinine >2 mg/dL: n (%) | Yes | 9 (0.5) | 9 (2.0) | 0.001 |
| Previous CVA: n (%) | Yes | 26 (1.3) | 20 (4.3) | <0.001 |
| IHD: n (%) | Yes | 89 (4.6) | 39 (8.5) | 0.001 |
| CCF: n (%) | Yes | 12 (0.6) | 6 (1.3) | 0.128 |
| Smoking: n (%) | Yes | 184 (9.5) | 43 (9.3) | 0.90 |
| ASA-PS | 1 | 137 (7.1) | 26 (5.6) | <0.001 |
| 2 | 1699 (87.9) | 382 (82.9) | ||
| 3 | 97 (5.0) | 53 (11.5) | ||
ASA-PS, American Society of Anesthesiologist Physical Status; CCF, congestive cardiac failure; CVA, cerebrovascular accidents; DM, diabetes mellitus; GA, general anaesthesia; IHD, ischaemic heart disease; LOS, length of stay; RA, regional anaesthesia; TKR, total knee replacement.
Table 2.
Variables that predict increased LOS in hospital after primary unilateral total knee replacement, based on univariate and multivariate analysis
| Variable | OR (95% CI) | p Value | aOR (95% CI) | p Value | |
| Patient demographics | |||||
| Age (years) | <60 | REF | REF | ||
| 60–64 | 0.95 (0.66 to 1.37) | 0.78 | 1.08 (0.73 to 1.59) | 0.71 | |
| 65–69 | 1.37 (0.98 to 1.92) | 0.07 | 1.42 (0.98 to 2.06) | 0.06 | |
| >70 | 2.04 (1.51 to 2.75) | <0.001 | 1.94 (1.38 to 2.73) | <0.001 | |
| Race | Malay | 0.66 (0.42 to 1.03) | 0.07 | 0.53 (0.31 to 0.92) | 0.02 |
| Indian | 1.24 (0.82 to 1.87) | 0.32 | 1.34 (0.85 to 2.11) | 0.21 | |
| Others | 1.82 (1.09 to 3.04) | 0.02 | 1.49 (0.83 to 2.68) | 0.19 | |
| Chinese | REF | REF | |||
| Body mass index | <25 | REF | REF | ||
| 25–29.9 | 0.90 (0.71 to 1.15) | 0.41 | 1.02 (0.78 to 1.32) | 0.91 | |
| 30–34.9 | 0.76 (0.56 to 1.03) | 0.07 | 0.92 (0.65 to 1.28) | 0.61 | |
| ≥35 | 1.18 (0.78 to 1.78) | 0.43 | 1.56 (0.96 to 2.53) | 0.07 | |
| Gender | Male | REF | REF | ||
| Female | 1.15 (0.90 to 1.47) | 0.25 | 1.20 (0.89 to 1.63) | 0.23 | |
| Details of operation | |||||
| Type of anaesthesia | GA | REF | REF | ||
| RA | 0.76 (0.62 to 0.94) | 0.01 | 0.75 (0.59 to 0.95) | 0.02 | |
| Duration of operation (minutes) | ≤100 | REF | REF | ||
| >100 | 1.41 (1.09 to 1.84) | 0.01 | 1.37 (1.03 to 1.84) | 0.03 | |
| Perioperative blood transfusion (units) | None | REF | REF | ||
| 1 | 4.10 (2.61 to 6.45) | <0.001 | 2.12 (1.24 to 3.60) | 0.006 | |
| ≥2 | 13.01 (6.46 to 26.17) | <0.001 | 6.71 (3.14 to 14.33) | <0.001 | |
| Repeat operation within Hhospital stay | 25.48 (3.06 to 212.14) | 0.003 | 15.22 (1.38 to 167.59) | 0.03 | |
| Day of week of operation | Monday | 2.20 (1.54 to 3.13) | <0.001 | 2.38 (1.62 to 3.49) | <0.001 |
| Tuesday | 2.10 (1.51 to 2.93) | <0.001 | 2.42 (1.68 to 3.49) | <0.001 | |
| Wednesday | 1.93 (1.35 to 2.76) | <0.001 | 2.21 (1.50 to 3.24) | <0.001 | |
| Thursday | REF | REF | |||
| Friday | 2.14 (1.50 to 3.06) | <0.001 | 1.99 (1.35 to 2.94) | 0.001 | |
| Saturday | 1.38 (0.79 to 2.41) | 0.25 | 1.46 (0.80 to 2.67) | 0.22 | |
| Patient comorbidities | |||||
| Anaemia | None | REF | REF | ||
| Mild | 1.97 (1.53 to 2.53) | <0.001 | 1.71 (1.29 to 2.27) | <0.001 | |
| Moderate/severe | 3.22 (2.29 to 4.53) | <0.001 | 2.29 (1.54 to 3.39) | <0.001 | |
| DM on insulin | 1.55 (0.77 to 3.12) | 0.22 | 1.20 (0.53 to 2.76) | 0.66 | |
| Creatinine >2 mg/dL | 4.26 (1.68 to 10.78) | 0.002 | 2.35 (0.78 to 7.11) | 0.13 | |
| Previous CVA | 3.33 (1.84 to 6.01) | <0.001 | 2.89 (1.50 to 5.55) | 0.001 | |
| IHD | 1.92 (1.30 to 2.83) | 0.001 | 1.50 (0.95 to 2.36) | 0.08 | |
| CCF | 2.11 (0.79 to 5.66) | 0.14 | 1.19 (0.38 to 3.75) | 0.77 | |
| Smoking | 0.98 (0.69 to 1.39) | 0.90 | 1.15 (0.76 to 1.75) | 0.50 | |
| ASA-PS score | 1 | REF | REF | ||
| 2 | 1.19 (0.77 to 1.83) | 0.44 | 0.96 (0.61 to 1.52) | 0.86 | |
| 3 | 2.88 (1.68 to 4.92) | <0.001 | 1.40 (0.77 to 2.56) | 0.27 | |
aOR, adjusted OR; ASA-PS, American Society of Anesthesiologist Physical Status; CCF, congestive cardiac failure; CVA, cerebrovascular accidents; DM, diabetes mellitus; GA, general anaesthesia; IHD, ischaemic heart disease; LOS, length of stay; RA, regional anaesthesia; REF, reference.
Table 3.
Factors associated with perioperative blood transfusion after primary unilateral TKR
| Variable | aOR (95% CI)* | p Value | |
| Type of anaesthesia | GA | REF | |
| RA | 0.57 (0.37 to 0.87) | 0.009 | |
| Duration of operation (minutes) | ≤100 | REF | |
| >100 | 1.89 (1.14 to 3.14) | 0.014 | |
| Repeat operation within hospital stay | 16.51 (2.22 to 123.04) | 0.006 | |
| Anaemia | None | REF | |
| Mild | 4.13 (2.54 to 6.71) | <0.001 | |
| Moderate/severe | 9.13 (5.34 to 15.61) | <0.001 | |
| ASA-PS score | 1 | REF | |
| 2 | 2.08 (0.63 to 6.90) | 0.23 | |
| 3 | 4.00 (1.05 to 15.21) | 0.042 | |
| CCF | 7.71 (2.24 to 26.53) | 0.001 |
*Adjusted for all the variables listed in table 1.
aOR, adjusted OR; ASA-PS, American Society of Anesthesiologist Physical Status; CCF, congestive cardiac failure; GA, general anaesthesia; RA, regional anaesthesia; REF, reference; TKR, total knee replacement.
Results
Demographics
Of the 2394 patients who underwent primary TKA during the study period, 23.7% were anaemic. Four hundred and three patients (16.8%) had mild preoperative anaemia, 159 patients (6.6%) had moderate anaemia and 5 patients had severe anaemia (0.2%). In table 1, patients with prolonged LOS had higher mean age (69.2 years) compared with patients with normal LOS (65.9 years), p<0.001. There was no significant difference in BMI or gender distribution between the two groups. However, those with prolonged LOS tended to have a higher ASA-PS score (p<0.001), higher incidence of anaemia (p<0.001), previous CVA (p<0.001), undergo repeat operation within their hospital stay (p<0.001) and received general anaesthesia compared with regional anaesthesia (p<0.01).
Length of stay
The mean LOS for all patients with TKA was 5.4 days (±4.8 days), with a median of 4 days and 75th centile of 6 days. This result is similar to previous published LOS rates of primary unilateral TKA in our institution.24
Four hundred and sixty-one patients (19.3%) had LOS more than 6 days (ie, prolonged LOS). Based on the multivariate analysis presented in table 2, the variables associated with independent elevated risk of prolonged LOS include older age >70 years (aOR 1.94, p<0.001), repeat surgery within LOS (aOR 15.22, p=0.03), having mild anaemia (aOR 1.71, p<0.001) or moderate/severe anaemia (aOR 2.29, p<0.001) and previous CVA (aOR 2.89, p=0.001). Perioperative blood transfusion of 1 unit independently increased risk of prolonged LOS by 2.12 (p=0.006), while transfusion of 2 or more units independently increased risk by 6.71 (p<0.001). Variables that reduced LOS include having regional anaesthesia (aOR 0.74, p=0.02), having surgery on Thursday and being of Malay race. BMI, gender, presence of DM on insulin, previous diagnosis of IHD, previous history of congestive heart failure or smoking and elevated ASA-PS scores were not associated with higher odds of prolonged LOS.
We repeated multivariate logistic regression for LOS with the non-gender-based Hb cut-offs as described earlier. Compared with no anaemia, mild anaemia (Hb 11.0–12.9 g/dL) had an aOR 1.39 (1.09, 1.76, p=0.007), while moderate/severe anaemia (Hb <11.0 g/dL) had an aOR of 2.35 (1.56, 3.54, p<0.001) of prolonged LOS (>6 days). These results were comparable to the findings generated with WHO definition of anaemia.
Perioperative blood transfusion
Our overall transfusion rate was 5.0%. Factors that increased risk of perioperative blood transfusion (table 3) included repeat operation during hospital stay (aOR 16.51, p=0.006), presence of mild anaemia (aOR 4.13, p<0.001) and moderate/severe anaemia (aOR 9.13, p<0.001), ASA-PS score of 3 (aOR 4.00, p=0.04) and history of CCF (aOR 7.71, p=0.001). Regional anaesthesia was found to reduce risk of perioperative blood transfusion (aOR 0.57, p=0.009).
Effect size of Hb on LOS
As shown in table 4, when perioperative transfusion was excluded, every 1 g increase in preoperative Hb reduced LOS by 0.2 days (95% CI 0.08 to 0.34, p=0.002). However, after including perioperative transfusion, every 1 g increase in preoperative Hb reduced LOS minimally by 0.07 days (95% CI −0.20 to 0.06, p=0.28).
Table 4.
Effect size of every 1 g increase in Hb, with and without factoring effect of perioperative blood transfusion based on general linear model
| Without adjusting for perioperative transfusion* | ||
| Hb increase | Increase in LOS in days (95% CI) | p Value |
| 1 g | −0.21 (-0.34 to 0.08) | 0.002 |
| 2 g | −0.42 (-0.68 to 0.16) | 0.002 |
| 3 g | −0.63 (-1.01 to 0.24) | 0.002 |
| After adjusting for perioperative transfusion† | ||
| Perioperative transfusion | ||
| 0 units | REF | |
| 1 unit | 4.02 (3.01 to 5.03) | <0.001 |
| ≥2 units | 8.35 (6.97 to 9.73) | <0.001 |
| Per unit increase in Hb by 1 g | −0.07 (-0.20 to 0.06) | 0.28 |
*R2=0.114, adjusted R2=0.103.
†R2 = 0.182, adjusted R2=0.171.
Hb, haemoglobin; LOS, length of stay; REF, reference.
Hospital readmission within 30 days
We had 42 cases of related readmission within 30 days of discharge out of 2394 cases (1.7%) (table 5). Due to the low rates of readmission, no further statistical analysis was done.
Table 5.
Causes of related admission within 30 days of discharge after primary unilateral total knee replacement
| Causes of readmission | N |
| Surgical site infection | 13 |
| Pain/swelling/stiffness | 11 |
| Non-infective wound discharge | 5 |
| Deep vein thrombosis | 4 |
| Periprosthetic fracture | 3 |
| Haematoma/bleeding | 2 |
| Erythema | 2 |
| Contact dermatitis | 1 |
| Wound dehiscence | 1 |
| Grand total | 42 |
Discussion
In this retrospective cohort study of 2394 consecutive patients who underwent elective unilateral primary TKA in our centre, the prevalence of WHO-defined preoperative anaemia was 23.7%. Patients with mild preoperative anaemia had an adjusted OR (aOR) of prolonged LOS (>6 days) of 1.71, while patients with moderate/severe anaemia had an aOR of 2.29. Our findings are consistent with previous studies that show that preoperative anaemia independently increased LOS in ‘fast-track’ knee arthroplasty11 and in the ‘traditional pathway’ elective primary knee arthroplasty.25 As these studies were done in the western world health systems and variations in practice and rehabilitation protocols between countries may lead to a wide disparity in postoperative hospital stays after TKA,26–29 our study provided a perspective from a South East Asian healthcare system. In countries with advanced healthcare systems and an ageing population, the exponentially increasing number of TKAs performed yearly2 importunes that more effort is needed to identify modifiable risk factors for delayed hospital discharges.
Our study showed that every 1 g increase in preoperative Hb reduced the patient’s LOS in hospital by 0.2 days. While this number is small, the presence of preoperative anaemia is one of the strongest independent predictor of perioperative blood transfusion (mild anaemia is associated with aOR of blood transfusion of 4.13, p<0.001; moderate severe anaemia with aOR of transfusion of 9.13, p<0.001), which has a strong independent influence on prolonging LOS in our study. The transfusion of 1 unit of blood is associated with aOR of prolonged LOS of 2.12, p=0.006, while transfusion of 2 or more units has an aOR of 6.71, p<0.001. Other studies have also found preoperative anaemia to be a strong predictor for perioperative allogeneic blood transfusion in knee surgeries,30 31 which is associated with poorer outcomes and prolonged LOS.11 32 Thus, optimising preoperative anaemia becomes an important healthcare cost containment strategy, since TKAs are elective procedures that can be postponed to allow optimisation of risk factors for suboptimal outcomes.
Our study adds to the growing body of publications from Asian countries on the negative impact of preoperative anaemia on postoperative outcomes in orthopaedic and non-orthopaedic surgeries.33 34 International guidelines now recommend patient blood management programmes with early detection of preoperative anaemia to identify the cause and treat any underlying reversible causes, such as iron-deficiency anaemia.35 Such intervention can reduce postoperative blood transfusion, LOS and readmission. In particular, iron deficiency anaemia is amenable to administration of intravenous iron treatment. Froessler et al demonstrated that preoperative intravenous iron treatment of iron deficiency anaemia among patients who underwent major abdominal surgery resulted in reduction of median LOS by 3 days.36 In the UK, preoperative iron supplementation prior to elective hip/knee arthroplasty has reduced transfusion rates, 90-day readmission rates and halved median hospital LOS.37 In Australia, transfusion rates have also been reduced since similar interventions for the same surgeries.38 Unfortunately in our institution, further evaluation and management of anaemia is often left to the ordering physician’s discretion, and a more systematic approach to the detection and management of preoperative anaemia is timely.
We found comparable aOR of prolonged LOS using the WHO gender-based definition of anaemia, which defines mild anaemia in men to be between 11.0 and 12.9 g/dL and that in women to be between 11.0 and 11.9 g/dL, and a non-gender-based definition, which defines mild anaemia as Hb 11.0–12.9 g/dL for both genders. Therefore, this lends weight to the recent proposition for a non-gender based cut-off of <13.0 g/dL in defining preoperative anaemia for the purpose of patient blood management initiatives.39 40
One of the aims of our study was to identify the risk factors for 30-day hospital readmission in our study population. However, we were unable to do so due to the small incidence of 42 readmissions out of 2349 cases, which precludes any meaningful analysis. Our 30-day related readmission rates are similar to previous published rate in our institution, which is between 1.7% and 2.9% for primary unilateral TKR.24 This is lower than the 30-day all-cause readmission rates in literature of 4.0%–5.5%,41–43 because it only looks at readmission that is related to complications attributable to the surgery. Nevertheless, our readmission rates are similar to Schairer et al’s 30-day surgical readmission rate of 2.4%, of which cellulitis and surgical site infection are the most common causes. In our study, surgical site infection was also the most common cause of readmission (31.1%).
Strengths of study
One of the strengths of our study was that it is among the first few to control for the day of the week the surgery was done, which has recently been shown to affect LOS in TKA and total hip arthroplasty.21 We found that having surgery on Thursday is significantly associated with the lowest odds of prolonged LOS. We postulate that this is because patients would have received standard physiotherapy for at least 2 days, on Friday and Saturday, and may be inclined to go home on Sunday where there is more familial support at home.
Another strength of our study is that we included both subjective measures of clinical risk estimates such as the ASA-PS score,27 43 as well as the components of the RCRI, which comprise diagnosis of specific conditions. This allowed us to find that out of the five clinical conditions within the RCRI score, only a history of previous CVA was significantly associated with increased LOS (aOR 2.89, p=0.001). Furthermore, a history of CCF was found to be associated with increased risk of perioperative blood transfusion (aOR 7.71, p=0.001).
Finally, we focused our study on patients who underwent primary TKA rather than combining hip and knee arthroplasty together, which is more commonly done in literature, as we wanted a more homogenous study population. We excluded revision and bilateral TKA as they are known in literature to be associated with increased need for blood transfusion and LOS.44 45
Our study recruitment occurred over 1.5 years. Our recruitment period is similar to another study published on this topic, which recruited over a 2-year period.11 We feel that this is an advantage as no major changes in healthcare and discharge policy occurred during this short time frame that would influence our primary outcome of LOS.
Limitations of study
We also had a modest study cohort of 2349 patients, which is comparable with other studies.11 41 While our study was performed retrospectively, it had minimal missing data (2.0%). This may be due to the fact that our clinical data, such as the preoperative variables, were collected electronically in a mandatory, prospective manner during routine preoperative anaesthesia assessment. Due to the observational nature of the study, a causal relationship between preoperative anaemia and adverse outcomes is difficult to establish. In addition, while our selection of the 75th centile for defining prolonged LOS can be viewed as an arbitrary cut-off in the absence of a universal definition of prolonged LOS, the use of 75th centile has been done in literature before for a similar study.22 We do not have data on whether drains were placed by the surgeons during the surgery; however, a recent study done in the same institution showed that while drains were associated with a larger drop in Hb level and greater total blood loss, it did not significantly impact blood transfusion rate, LOS or 30-day readmission rates.24 We also did not have data on the prevalence of the use of intraoperative tranexamic acid infiltration into the joint, administration of intravenous tranexamic acid by the anaesthesiologists, or use of leucodepleted blood products for transfusion. Non-leucodepleted blood has been postulated to reduce transfusion related immunomodulatory effects including mortality,46 although clinical studies in cardiac surgery have not proven to be conclusive so far.47 48
Conclusion
In conclusion, we found the prevalence of preoperative anaemia to be 23.7% among patients who underwent primary TKA in Singapore. It was an independent risk factor for prolonged length of hospital stay and perioperative blood transfusion. We suggest measures to correct anaemia prior to surgery, including the use of non-gender-based Hb cut-off for establishing diagnosis.
bmjopen-2017-016403supp001.doc (80.5KB, doc)
Supplementary Material
Acknowledgments
We would like to thank Ms Serene Ong, Academic Medicine Research Institute, Duke-NUS Medical School, for her help in manuscript preparation. We would also like to thank Ms Sudha Harikrishnan, from the Department of Anaesthesiology, for her invaluable help in data extraction. This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. Lastly, we would also like to thank Dr Chan Yiong Huak, Head, Biostatistics Unit, Yong Loo Lin School of Medicine, National University of Singapore, National University Health System, Singapore, for his invaluable help in data analysis and interpretation.
Footnotes
Contributors: HRA contributed to the study conception and design, data acquisition, analysis and interpretation, drafting and final approval of the manuscript. YES contributed to data analysis and interpretation, drafting, revision and final approval of the manuscript. YH contributed to data analysis and interpretation, drafting of the manuscript and final approval. GYL contributed to data acquisition, analysis and interpretation, drafting of the manuscript and final approval. GHCL contributed to the study conception and design, data analysis, revision of the manuscript and final approval. ELL contributed to data analysis and critical appraisal, revision and final approval of the manuscript. MHT contributed to the study conception and design, drafting of manuscript and final approval.
Funding: This research was funded by the hospital department funds.
Competing interests: None declared.
Patient consent: As this was a retrospective analysis of medical records, waiver of patient's consent was obtained from the ethics board.
Ethics approval: Singhealth Institutional Review Board.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Full dataset used in the analysis can be downloaded from Dryad public repository at doi:10.5061/dryad.73250
References
- 1. Baron DM, Hochrieser H, Posch M, et al. . Preoperative anaemia is associated with poor clinical outcome in non-cardiac surgery patients. Br J Anaesth 2014;113:416–23. 10.1093/bja/aeu098 [DOI] [PubMed] [Google Scholar]
- 2. Maradit Kremers H, Larson DR, Crowson CS, et al. . Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am 2015;97:1386–97. 10.2106/JBJS.N.01141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. den Hertog A, Gliesche K, Timm J, et al. . Pathway-controlled fast-track rehabilitation after total knee arthroplasty: a randomized prospective clinical study evaluating the recovery pattern, drug consumption, and length of stay. Arch Orthop Trauma Surg 2012;132:1153–63. 10.1007/s00402-012-1528-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Husted H, Jensen CM, Solgaard S, et al. . Reduced length of stay following hip and knee arthroplasty in Denmark 2000-2009: from research to implementation. Arch Orthop Trauma Surg 2012;132:101–4. 10.1007/s00402-011-1396-0 [DOI] [PubMed] [Google Scholar]
- 5. Healy WL, Rana AJ, Iorio R. Hospital economics of primary total knee arthroplasty at a teaching hospital. Clin Orthop Relat Res 2011;469:87–94. 10.1007/s11999-010-1486-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lovald ST, Ong KL, Malkani AL, et al. . Complications, mortality, and costs for outpatient and short-stay total knee arthroplasty patients in comparison to standard-stay patients. J Arthroplasty 2014;29:510–5. 10.1016/j.arth.2013.07.020 [DOI] [PubMed] [Google Scholar]
- 7. Kim S, Losina E, Solomon DH, et al. . Effectiveness of clinical pathways for total knee and total hip arthroplasty: literature review. J Arthroplasty 2003;18:69–74. 10.1054/arth.2003.50030 [DOI] [PubMed] [Google Scholar]
- 8. HCUPnet: a tool for identifying, tracking, and analyzing national hospital statistics. http://hcupnet.ahrq.gov/ (accessed 15 Aug 2016).
- 9. Ayalon O, Liu S, Flics S, et al. . A multimodal clinical pathway can reduce length of stay after total knee arthroplasty. Hss J 2011;7:9–15. 10.1007/s11420-010-9164-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Liodakis E, Bergeron SG, Zukor DJ, et al. . Perioperative complications and length of Stay after Revision Total hip and knee arthroplasties: an analysis of the NSQIP database. J Arthroplasty 2015;30:1868–71. 10.1016/j.arth.2015.05.029 [DOI] [PubMed] [Google Scholar]
- 11. Jans Ø, Jørgensen C, Kehlet H, et al. . Role of preoperative Anemia for risk of transfusion and postoperative morbidity in fast-track hip and knee arthroplasty. Transfusion 2014;54:717–26. 10.1111/trf.12332 [DOI] [PubMed] [Google Scholar]
- 12. Viola J, Gomez MM, Restrepo C, et al. . Preoperative Anemia increases postoperative complications and mortality following total joint arthroplasty. J Arthroplasty 2015;30:846–8. 10.1016/j.arth.2014.12.026 [DOI] [PubMed] [Google Scholar]
- 13. Chamieh JS, Tamim HM, Masrouha KZ, et al. . The Association of Anemia and its severity with cardiac outcomes and Mortality after Total Knee Arthroplasty in Noncardiac Patients. J Arthroplasty 2016;31:766–70. 10.1016/j.arth.2015.10.035 [DOI] [PubMed] [Google Scholar]
- 14. Jans Ø, Jørgensen C, Kehlet H, et al. . Role of preoperative Anemia for risk of transfusion and postoperative morbidity in fast-track hip and knee arthroplasty. Transfusion 2014;54 http://onlinelibrary.wiley.com/doi/ 10.1111/trf.12332 [DOI] [PubMed] [Google Scholar]
- 15. Pitter FT, Jørgensen CC, Lindberg-Larsen M, et al. . Postoperative morbidity and discharge destinations after Fast-Track hip and knee arthroplasty in patients older than 85 years. Anesth Analg 2016;122:1807–15. 10.1213/ANE.0000000000001190 [DOI] [PubMed] [Google Scholar]
- 16. Greenky M, Gandhi K, Pulido L, et al. . Preoperative Anemia in total joint arthroplasty: is it associated with periprosthetic joint infection? Clin Orthop Relat Res 2012;470:2695–701. 10.1007/s11999-012-2435-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Husted H, Holm G, Jacobsen S. Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop 2008;79:168–73. 10.1080/17453670710014941 [DOI] [PubMed] [Google Scholar]
- 18. Fleisher LA, Fleischmann KE, Auerbach AD, et al. . ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice guidelines. Circulation 2014;2014:2215–45. [DOI] [PubMed] [Google Scholar]
- 19. Lee TH, Marcantonio ER, Mangione CM, et al. . Derivation and prospective validation of a simple index for prediction of cardiac risk of Major noncardiac surgery. Circulation 1999;100:1043–9. 10.1161/01.CIR.100.10.1043 [DOI] [PubMed] [Google Scholar]
- 20. American Society of Anesthesiologists - ASA physical status classification system. https://www.asahq.org/resources/clinical-information/asa-physical-status-classification-system (accessed 11 Jul2016).
- 21. Newman JM, Szubski CR, Barsoum WK, et al. . Day of Surgery affects length of Stay and Charges in primary total hip and knee arthroplasty. J Arthroplasty 2017;32 10.1016/j.arth.2016.06.032 [DOI] [PubMed] [Google Scholar]
- 22. Almashrafi A, Alsabti H, Mukaddirov M, et al. . Factors associated with prolonged length of stay following cardiac surgery in a Major referral hospital in Oman: a retrospective observational study. BMJ Open 2016;6:e010764 10.1136/bmjopen-2015-010764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Health Organization W. Nutritional anaemias: report of a WHO scientific group [meeting held in Geneva from 13 to 17 March 1967]. http://apps.who.int/iris/handle/10665/40707.
- 24. Chen JY, Lee WC, Chan HY, et al. . Drain use in total knee arthroplasty is neither associated with a greater transfusion rate nor a longer hospital stay. Int Orthop 2016;40:2505–9. 10.1007/s00264-016-3239-7 [DOI] [PubMed] [Google Scholar]
- 25. Smith ID, Elton R, Ballantyne JA, et al. . Pre-operative predictors of the length of hospital stay in total knee replacement. J Bone Joint Surg Br 2008;90:1435–40. 10.1302/0301-620X.90B11.20687 [DOI] [PubMed] [Google Scholar]
- 26. Monsef JB, Della Valle AG, Mayman DJ, et al. . The impact of blood management on length of stay after primary total knee arthroplasty. Open Orthop J 2014;8:108–13. 10.2174/1874325001408010108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Vorhies JS, Wang Y, Herndon JH, et al. . Decreased length of stay after TKA is not associated with increased readmission rates in a National Medicare sample. Clin Orthop Relat Res 2012;470:166–71. 10.1007/s11999-011-1957-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Krämer S, Wenk M, Fischer G, et al. . Continuous spinal anesthesia versus continuous femoral nerve block for elective total knee replacement. Minerva Anestesiol 2011;77:394–400. [PubMed] [Google Scholar]
- 29. Dauty M, Smitt X, Menu P, et al. . Which factors affect the duration of inpatient rehabilitation after total knee arthroplasty in the absence of complications? Ann Phys Rehabil Med 2009;52:234–45. 10.1016/j.rehab.2009.01.001 [DOI] [PubMed] [Google Scholar]
- 30. Salido JA, Marín LA, Gómez LA, et al. . Preoperative hemoglobin levels and the need for transfusion after prosthetic hip and knee surgery: analysis of predictive factors. J Bone Joint Surg Am 2002;84-A:216–20. 10.2106/00004623-200202000-00008 [DOI] [PubMed] [Google Scholar]
- 31. Carling MS, Jeppsson A, Eriksson BI, et al. . Transfusions and blood loss in total hip and knee arthroplasty: a prospective observational study. J Orthop Surg Res 2015;10:48 10.1186/s13018-015-0188-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Whitlock EL, Kim H, Auerbach AD. Harms associated with single unit perioperative transfusion: retrospective population based analysis. BMJ 2015;350:h3037 10.1136/bmj.h3037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jung DH, Lee HJ, Han DS, et al. . Impact of perioperative hemoglobin levels on postoperative outcomes in gastric Cancer surgery. Gastric Cancer 2013;16:377–82. 10.1007/s10120-012-0196-8 [DOI] [PubMed] [Google Scholar]
- 34. Zhang L, Yin P, Lv H, et al. . Anemia on admission is an independent predictor of Long-Term Mortality in hip fracture Population: a prospective study with 2-Year Follow-Up. Medicine 2016;95:e2469 10.1097/MD.0000000000002469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Goodnough LT, Maniatis A, Earnshaw P, et al. . Detection, evaluation, and management of preoperative anaemia in the elective orthopaedic surgical patient: nata guidelines. Br J Anaesth 2011;106:13–22. 10.1093/bja/aeq361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Froessler B, Palm P, Weber I, et al. . The important role for intravenous iron in Perioperative Patient Blood Management in Major abdominal surgery: a Randomized Controlled Trial. Ann Surg 2016;264:41–6. 10.1097/SLA.0000000000001646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Frew N, Alexander D, Hood J, et al. . Impact of a blood management protocol on transfusion rates and outcomes following total hip and knee arthroplasty. Ann R Coll Surg Engl 2016;98:380–6. 10.1308/rcsann.2016.0139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kopanidis P, Hardidge A, McNicol L, et al. . Perioperative blood management programme reduces the use of allogenic blood transfusion in patients undergoing total hip and knee arthroplasty. J Orthop Surg Res 2016;11:28 10.1186/s13018-016-0358-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Muñoz M, Gómez-Ramírez S, Kozek-Langeneker S, et al. . 'Fit to fly': overcoming barriers to preoperative haemoglobin optimization in surgical patients. Br J Anaesth 2015;115:15–24. 10.1093/bja/aev165 [DOI] [PubMed] [Google Scholar]
- 40. Muñoz M, Acheson AG, Auerbach M, et al. . International consensus statement on the peri-operative management of anaemia and iron deficiency. Anaesthesia 2017;72:233–47. 10.1111/anae.13773 [DOI] [PubMed] [Google Scholar]
- 41. Schairer WW, Vail TP, Bozic KJ. What are the rates and causes of hospital readmission after total knee arthroplasty? Clin Orthop Relat Res 2014;472:181–7. 10.1007/s11999-013-3030-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Brown NM, Sheth NP, Davis K, et al. . Total knee arthroplasty has higher postoperative morbidity than unicompartmental knee arthroplasty: a multicenter analysis. J Arthroplasty 2012;27:86–90. 10.1016/j.arth.2012.03.022 [DOI] [PubMed] [Google Scholar]
- 43. Huddleston JI, Maloney WJ, Wang Y, et al. . Adverse events after total knee arthroplasty: a national Medicare study. J Arthroplasty 2009;24:95–100. 10.1016/j.arth.2009.05.001 [DOI] [PubMed] [Google Scholar]
- 44. Callaghan JJ, Spitzer AI. Blood management and patient specific transfusion options in total joint replacement surgery. Iowa Orthop J 2000;20:36–45. [PMC free article] [PubMed] [Google Scholar]
- 45. Robinson S, McGonigle O, Volin S, et al. . Comprehensive look at Blood Transfusion utilization in Total Joint Arthroplasty at a Single Academic Medical Center under a Single Surgeon. J Blood Transfus 2013;2013:1–6. 10.1155/2013/983250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. FAQ: leucodepletion of red cells and platelets from Australian Red Cross Blood Service. https://www.transfusion.com.au/blood_products/components/leucodepletion (accessed 16 Mar2017).
- 47. Murphy GJ, Reeves BC, Rogers CA, et al. . Increased mortality, postoperative morbidity, and cost after red blood cell transfusion in patients having cardiac surgery. Circulation 2007;116:2544–52. 10.1161/CIRCULATIONAHA.107.698977 [DOI] [PubMed] [Google Scholar]
- 48. McQuilten ZK, Andrianopoulos N, van de Watering L, et al. . Introduction of universal prestorage leukodepletion of blood components, and outcomes in transfused cardiac surgery patients. J Thorac Cardiovasc Surg 2015;150:216–22. 10.1016/j.jtcvs.2015.03.015 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-016403supp001.doc (80.5KB, doc)


