Abstract
Maternal trauma is a complex risk factor that has been linked to adverse child outcomes, yet the mechanisms underlying this association are not well understood. This study, which included adoptive and biological families, examined the heritable and environmental mechanisms by which maternal trauma and associated depressive symptoms are linked to child internalizing and externalizing behaviors. Path analyses were used to analyze data from 541 adoptive mother–adopted child (AM–AC) dyads and 126 biological mother–biological child (BM–BC) dyads; the two family types were linked through the same biological mother. Rearing mother’s trauma was associated with child internalizing and externalizing behaviors in AM–AC and BM–BC dyads, and this association was mediated by rearing mothers’ depressive symptoms, with the exception of biological child externalizing behavior, for which biological mother trauma had a direct influence only. Significant associations between maternal trauma and child behavior in dyads that share only environment (i.e., AM–AC dyads) suggest an environmental mechanism of influence for maternal trauma. Significant associations were also observed between maternal depressive symptoms and child internalizing and externalizing behavior in dyads that were only genetically related, with no shared environment (i.e., BM–AC dyads), suggesting a heritable pathway of influence via maternal depressive symptoms.
Keywords: maternal trauma, internalizing behaviors, externalizing behaviors, maternal depressive symptoms, adoption design
Early exposure to adverse experiences has consistently been linked to long-term negative physical and mental health outcomes (e.g., Danese et al., 2009; Reuben et al., 2016; Scott, Smith, & Ellis, 2010), including the development of internalizing and externalizing behaviors in children (Greeson et al., 2014). Maternal trauma exposure is one type of early adversity that can increase risk for maternal depression (e.g., Mayou, Bryant, & Ehlers, 2001; O’Donnell, Creamer, Pattison, & Atkin, 2004) and child internalizing and externalizing behaviors (Bifulco, Moran, Ball, & Bernazzani, 2002; Lambert, Holzer, & Hasbun, 2014). Nevertheless, little is known about whether the mechanisms linking maternal trauma and depressive symptoms with child internalizing and externalizing behaviors result from biological influences, environmental influences, or both.
We used a linked sample of adoptive and biological mother–child dyads to disentangle the environmental and biological mechanisms by which maternal trauma and depressive symptoms are associated with child internalizing and externalizing behaviors. The two family types were linked through the biological mother, who reared one biological child and placed another child for adoption. This study design allows for a novel examination of biological and environmental mechanisms because heritable influences can be traced through the biological mother’s depressive symptoms across both family types, while shared genetic influences are not present in the adoptive mother-adopted child dyads, thereby isolating environmental risk factors in these dyads. Although maternal trauma has been linked to higher rates of maternal depressive symptoms (e.g., Kinderman, Schwannauer, Pontin, & Tai, 2013), and maternal depressive symptoms have in turn been associated with child internalizing and externalizing behaviors (Goodman et al., 2011), previous research has not tested these pathways together in the same model. Our study addressed this gap by examining maternal depressive symptoms as a mediator of the relationship between maternal trauma and child internalizing and externalizing behaviors at child age 7 years in adoptive and biological families.
Theories of Intergenerational Effects of Trauma
Prominent theories of intergenerational effects of trauma (e.g., Kellermann, 2001; Klein-Parker, 1988; Sotero, 2006) posit that maternal trauma and its adverse consequences are passed on to children through exposure to the mother’s stress, emotional numbing and detachment, and overall limited psychosocial functioning that can negatively influence the quality of the rearing environment (Schwerdtfeger & Goff, 2007; Thompson, 2007; Wiseman, 2008). These theories posit that child internalizing and externalizing behaviors are linked to maternal trauma through children’s direct exposure to, and/or modeling of, their mother’s trauma symptoms (Walker, 1999), mental health problems (e.g., depression; Felsen, 1998), and adaptation patterns (Fraiberg, Adelson, & Shapiro, 1975). Rearing environments provided by mothers who experience ongoing emotional difficulties as a result of trauma are characterized by low responsivity and lack of emotional availability, more coercive interactions, and less parental monitoring (Felsen, 2017; Reich, Earls, & Powell, 1988), all of which increase the risk of internalizing and externalizing behaviors in children (Loukas, Piejak, Bingham, Fitzgerald, & Zucker, 2001). Exposure to such rearing environments during early childhood can be particularly detrimental to the socioemotional development of children (Cicchetti & Toth, 1998a; Goodman & Gotlib, 2002; Murray, Halligan, Adams, Patterson, & Goodyer, 2006).
The effects of maternal trauma on child developmental outcomes can be especially pronounced in contexts of socioeconomic risk. Low socioeconomic status (SES) contexts can exacerbate the negative effects of trauma on depression (Lorant, Deliege, & Eaton, 2003) and child internalizing behavior (Krauss, Wilson, Padrón, & Samuelson, 2016). Therefore, we hypothesized that maternal trauma and associated depressive symptoms would have stronger behavioral consequences in children reared in low SES backgrounds. We tested this hypothesis by comparing the associations between maternal trauma, maternal depressive symptoms, and child internalizing and externalizing behavior across two family types that differed significantly in their socioeconomic backgrounds.
Environmental and Heritable Pathways From Maternal Depressive Symptoms to Child Behavior
Past studies suggest a mediational role of maternal depressive symptoms in the link between maternal trauma and child behavior problems (e.g., Dubowitz et al., 2001; Min, Singer, Minnes, Kim, & Short, 2013). However, maternal depressive symptoms can affect child behavior through environmental influences (e.g., Natsuaki et al., 2014), heritable factors (e.g., Thapar, Collishaw, Pine, & Thapar, 2012), or an interplay of the two. Several prominent theories suggest that the effects of maternal depressive symptoms on child behaviors are driven by environmental mechanisms (e.g., Cicchetti, Rogosch, & Toth, 1998; Cummings & Davies, 1994; Shaw, Dishion, Connell, Wilson, & Gardner, 2009). Findings from these studies have been further validated by adoption and children-of-twins study designs that include tests of environmental mechanisms above and beyond genetically driven effects. A recent review of these studies demonstrates a consistent link between maternal depressive symptoms and child internalizing and externalizing behaviors in early and middle childhood (Natsuaki et al., 2014). Previous research that used the adoptive families in our study (Leve et al., 2013) has illustrated effects of adoptive mothers’ depressive symptoms on children’s internalizing and externalizing behaviors at age 18 months, and externalizing behaviors at 27 months, controlling for birth mothers’ major depressive disorder (Kerr et al., 2013; Pemberton et al., 2010). Similar findings have been reported in children-of-twins studies in the United States (Silberg, Maes, & Eaves, 2010), Australia (Singh et al., 2011), and Sweden (Class et al., 2012), indicating an environmental mechanism of influence for maternal depressive symptoms.
Other reviews (e.g., McGuffin & Katz, 1989; Rice, Harold, & Thapar, 2002; Sullivan, Neale, & Kendler, 2000; Thapar et al., 2012) and twin studies (e.g., Rice et al., 2002) suggest low to moderate heritability of depressive symptoms. Consequently, children of mothers with elevated depressive symptoms may have a genetic propensity toward internalizing behaviors (Ferentinos et al., 2015). Similar findings by Goodman and colleagues (2011) in children of depressed mothers suggest an inherited vulnerability for externalizing behaviors in first-degree relatives (Kovacs, Devlin, Pollock, & Mukerji, 1997; Williamson et al., 1995). In consideration of these findings, we examined both environmental and heritable pathways from maternal depressive symptoms to child behaviors in our models.
Novel Study Design
By using a parent–child adoption design that included linked biological and adoptive mother–child dyads, we were able to examine the mediating role of maternal depressive symptoms on the relationship between maternal trauma and child internalizing and externalizing behaviors while differentiating inherited and rearing environmental pathways of influence. The inclusion of the adoption sample allowed for elimination of passive gene–environment correlation (rGE) in the proposed associations between rearing mothers’ trauma and depressive symptoms, and child behaviors. Passive rGE is one way in which children’s inherited qualities are associated with their environment; it occurs when genes are shared between a rearing parent and a child, thus confounding the effects of the rearing environment with heritable influences (Harold et al., 2011; Jaffee & Price, 2007; Price & Jaffee, 2008). Therefore, in the adoption sample, similarities between the adoptive mother’s trauma and depressive symptoms and the adopted child’s behavior would suggest an environmental mechanism of influence, due to the influence of the shared rearing environment and the lack of shared genes (Leve et al., 2017). Our study also included data from the adopted child’s biological mother, which enabled us to examine the heritable effects of a biological mother’s depressive symptoms on the adopted child’s internalizing and externalizing behaviors. Similarities between a biological mother and the adopted child reflect heritable influences and/or influences of the biological mother’s prenatal environment, given the lack of a shared postnatal rearing environment between the biological mother and adopted child.
We included a second sample that was linked to the adoption sample via the biological mother. This sample included dyads of the biological mother and the biological child she was rearing. Together, this set of study samples enabled us to test for replication of the effects across two samples that varied in terms of the child’s genetic relatedness to the mother (related or unrelated) and allowed us to compare path coefficients between rearing mother depressive symptoms and child externalizing and internalizing behaviors when passive rGE was, or was not, a design element.
Study Hypotheses
Our study used a multilevel approach by examining internalizing and externalizing behaviors as two separate outcomes, investigating heritable and environmental pathways of influence of maternal trauma via the effects of maternal depressive symptoms on child internalizing and externalizing behaviors, and comparing these associations across the two family types (i.e., biological mother–biological child families and adoptive mother–adopted child families) that also varied in terms of their socioeconomic background.
First, we hypothesized that rearing mother trauma would be related to child internalizing and externalizing behaviors assessed at child age 7 years in both family types. Given our study design, particularly the lack of measurement of epigenetic processes, we did not hypothesize a heritable association between biological mother trauma and adopted child behaviors, because this association was unlikely to be captured at the behavioral level.
Second, we hypothesized that rearing mother depressive symptoms would mediate the association between rearing mother trauma and child internalizing and externalizing behaviors in both samples. Maternal depressive symptoms were expected to have both behavioral and biological pathways of influence. Specifically, in adoptive families, we hypothesized that adoptive mother depressive symptoms would act as an environmental mediator of the association between adoptive mother trauma and adopted child externalizing and internalizing behaviors; in biological families, we hypothesized that biological mother depressive symptoms would act as both an environmental and biological mediator of the association between biological mother trauma and biological child externalizing and internalizing behaviors. Given the genetic relatedness of the biological family dyads, the environmental and heritable effects of maternal depressive symptoms cannot be disentangled.
Third, we hypothesized that biological mother depressive symptoms would operate as a heritable mechanism of influence that would be associated with adopted child externalizing and internalizing behaviors. Fourth, we hypothesized that the direct and mediated associations between rearing mother trauma and child internalizing and externalizing behaviors would be stronger in the biological families in our sample, given their lower SES as compared with SES of adoptive families.
Methods
Participants
We used data from two linked studies of mother–child dyads that varied on whether the rearing mother was the biological parent or not. Study 1 included adoptive mother–adopted child dyads enrolled in the Early Growth and Development Study (EGDS), which is an ongoing, multisite, longitudinal adoption study designed to examine family, peer, and other social context factors that affect child development (Leve et al., 2013). The biological mother of the adoptee also participated in Study 1. Children were adopted within 3 months postpartum, with the median child age at adoption placement being 2 days (M = 6.2 days, SD = 12.45; range = 0–91 days). The eligibility criteria for the EGDS sample included the following: domestic and nonrelative adoption placement; both biological and adoptive parents able to understand English at the eighth-grade level; and no known major medical conditions, such as extensive medical surgeries, extreme prematurity, or any condition that required the child to be in the neonatal intensive care unit for more than 1 week (for more detail, see Leve et al., 2013). For our study, we included data across seven waves, from adopted child age 5 months to 7 years (n = 541). Child internalizing and externalizing behaviors were assessed at approximately age 7. Adoptive mother trauma and depressive symptoms were assessed during the span of 6.25 years, beginning at child age 9 months. Biological mother depressive symptoms were assessed from adopted child age 5 to 54 months to index heritable influences on adopted child behavior. For child internalizing and externalizing behaviors and one of our control variables (adoption openness), data from biological fathers (BF; n = 49) and adoptive fathers (AF; n = 330), when available, were used to create average scores based on maternal and paternal reports. In all other cases, only maternal reports were used.
Study 2 included a linked subsample of EGDS biological mothers who were rearing a biological child (i.e., a biological sibling to an adopted child in EGDS). Children in Study 2 were assessed at around age 7 (n = 126) as part of the ongoing Early Parenting of Children (EPoCh) study (Leve et al., 2017). Biological mother trauma was assessed over the lifetime, and her depressive symptoms were assessed from adopted child age 5 to 54 months. For biological child internalizing and externalizing behavior, when available, data from biological fathers (n = 49) were also included to create average scores based on maternal and paternal reports.
Biological mothers represented in the EPoCh subsample are a subset of biological mothers in the EGDS sample and were predominantly Caucasian (EGDS: 73.8%, EPoCh: 69.0%) and from low SES (annual household income less than $25,000 for EGDS and EPoCh), with a median education of high school diploma (EGDS and EPoCh). Adoptive mothers in EGDS tended to be middle class (annual household income more than $70,000) and college educated. There was a significant difference between biological mother and adoptive mother household income, t(226) = 27.85, p < .001, and education level, t(170) = 19.67, p < .001. The average age of the EGDS and EPoCh children at the time of child outcome assessment was 7.12 years and 7.98 years, respectively, with similar distributions of gender (56.9% male for EGDS and 46.0% for EPoCh). Additional demographic information is available in Table 1.
Table 1.
Sample Demographics
| Biological mothers (n EGDS/EPoCh = 541/126) |
Adoptive mothers (n = 541) |
Biological children (n = 126) |
Adopted children (n = 541) |
|||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Variables | N | % | N | % | N | % | N | % |
| Sex | ||||||||
| Male | 58 | 46.0 | 308 | 56.9 | ||||
| Race | ||||||||
| White | 399/87 | 73.8/69.0 | 503 | 93.0 | 78 | 61.0 | 337 | 62.3 |
| Black | 74/26 | 13.7/20.6 | 19 | 3.5 | 27 | 21.4 | 72 | 13.3 |
| Asian | 1.8/0 | 5 | 0.9 | 0 | 0 | 1 | 0.2 | |
| American Indian/Alaskan | 13/1 | 2.4/0.8 | 1 | 0.2 | 1 | 0.8 | 3 | 0.6 |
| More than one race | 33/10 | 6.1/7.9 | 9 | 1.7 | 20 | 15.9 | 126 | 23.3 |
| Unknown | 4/2 | 0.7/1.6 | 4 | 0.7 | 0 | 0 | 1 | 0.2 |
| Education level | ||||||||
| < High school degree | 80/20 | 14.8/15.9 | 0 | 0.0 | - | - | - | - |
| GED degree | 63/19 | 11.6/15.1 | 4 | 0.7 | - | - | - | - |
| High school degree | 194/35 | 35.9/27.8 | 44 | 8.1 | - | - | - | - |
| Trade school | 76/24 | 14.0/19.0 | 19 | 3.5 | - | - | - | - |
| 2-yr college degree | 60/22 | 11.1/17.5 | 45 | 8.3 | - | - | - | - |
| 4-yr college degree | 45/6 | 8.3/4.8 | 214 | 39.6 | - | - | ||
| Graduate program | 12/0 | 2.2/0 | 202 | 37.3 | - | - | - | - |
| Household income | ||||||||
| < $15,000 | 156/47 | 28.8/37.3 | 4 | 0.7 | - | - | - | - |
| $15,001–$25,000 | 88/23 | 16.3/18.3 | 5 | 0.9 | - | - | - | - |
| $25,001–$40,000 | 95/24 | 17.6/19.0 | 11 | 2.0 | - | - | - | - |
| $40,001–$55,000 | 55/11 | 10.2/8.7 | 14 | 2.5 | - | - | - | - |
| $55,001–$70,000 | 45/13 | 8.3/10.3 | 54 | 10.0 | - | - | - | - |
| $70,001–$100,000 | 39/4 | 7.2/3.2 | 106 | 19.6 | - | - | - | - |
| > $100,000 | 20/3 | 3.7/2.4 | 335 | 61.9 | - | - | - | - |
Measures
Maternal trauma frequency
Seven items from the Trauma Questionnaire (Norris, 1990) were used to assess trauma frequency in biological mothers, and seven matched items from the Negative Life Events Scale (NLS; Dohrenwend, Krasnoff Askenasy, & Dohrenwend, 1978; see Table 2) were used for adoptive mothers. The 13-item Trauma Questionnaire was administered to biological mothers as part of a telephone interview when adopted children were approximately 5 years old (M = 4.67; SD = 0.86; range = 2.82–7.25 years). Items assessed highly stressful events during the lifetime, with a yes/no response option (e.g., “Did anyone ever beat you up or attack you as an adult?”). For each positive response, the mother was asked whether she was pregnant when the event occurred. Given the impact of maternal psychological distress on fetal development and subsequent, long-lasting outcomes in children (Kinsella & Monk, 2009; O’Connor, Heron, Golding, Beveridge, & Glover, 2002; Pawlby, Hay, Sharp, Waters, & O’Keane, 2009; Talge, Neal, & Glover, 2007), traumatic events occurring during pregnancy with either the adopted child or the biological child were not included to partially account for any trauma experienced in utero. We selected seven items from this scale that matched with the items from the NLS that was administered to adoptive mothers. The scores on this variable ranged from 0 to 7 [M(SD) = 2.19(2.00)]. The NLS (Dohrenwend et al., 1978), administered to adoptive mothers, includes 31 items that assess important negative changes that the adoptive mother may have experienced in the past year, using a dichotomous (yes/no) response option (e.g., “Did you get beaten up, physically attacked, or sexually assaulted?”). To make the assessment of trauma in adoptive mothers comparable to the lifetime assessment of trauma in biological mothers, we averaged five waves of NLS data for adoptive mothers, collected at adopted child ages 9 months, 27 months, 4.5 years, 6 years, and 7 years. The composite score ranged from 0 to 3.33 [M(SD) = 0.50(0.49)] (see Table 3). Given that the individual items used to measure trauma frequency in these scales were not necessarily expected to correlate (i.e., the experience of one trauma is not necessarily related to the experience of another trauma), we did not compute inter-item alphas for these measures.
Table 2.
Trauma Items (n = 7) Matched Across the Trauma Questionnaire (Biological Mother) and the Negative Life Events Scale (Adoptive Mother)
| Trauma Questionnaire items (biological mother) | Negative Life Events Scale items (adoptive mother) |
|---|---|
| Have you ever had a life-threatening illness? | Have a serious illness or injury? |
| Were you ever in a life-threatening accident? | Have an automobile accident in which someone was injured? |
| Did anyone ever take something from you by force or threat of force, such as in a robbery, mugging, or holdup? | Get robbed? |
| Did anyone ever beat you up or attack you as an adult? | Get beaten up, physically attacked, or sexually assaulted? |
| Did you ever suffer injury or property damage because of fire, severe weather, or a natural or manmade disaster? | Suffer injury or property damage from a fire, severe weather, or other disaster? |
| Did a close friend or family member ever die because of an accident, homicide, or suicide? | Have a close friend who died? |
| Did you ever have some other extremely frightening, terrifying, or shocking experience that I haven’t mentioned? | Have some other terrifying or shocking experience? |
Note. For the Trauma Questionnaire, items were assessed for the biological mother’s lifetime and at one time point in the study in spring 2009, when adopted children were approximately age 5 years (M = 4.67; SD = 0.86; range = 2.82–7.25). For the Negative Life Events Scale, items were assessed for the past year and at five time points in the study at adopted child ages 9 months, 27 months, 4.5 years, 6 years, and 7 years.
Table 3.
Means, Standard Deviations, Ranges, and Correlations for Study Variables
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1.BMTr | - | ||||||||||||||||
| 2.BMDep | .30* | - | |||||||||||||||
| 3.BMInc | −.10 | −.21* | - | ||||||||||||||
| 4.BMEdu | −.01 | −.09* | .29* | - | |||||||||||||
| 5.BCSex | −.08 | −.09 | .16 | .01 | - | ||||||||||||
| 6.BCInt | .31* | .35* | −.08 | −.18 | −.14 | - | |||||||||||
| 7.BCExt | .33* | .25* | −.06 | −.17 | −.11 | .69* | - | ||||||||||
| 8.AMTr | .01 | .00 | −.07 | .01 | .16 | .14 | .16 | - | |||||||||
| 9.AMDep | −.10 | −.05 | .02 | −.02 | .15 | −.01 | .02 | .20* | - | ||||||||
| 10.AMInc | −.01 | −.10* | .12* | .01 | .22* | −.11 | −.12 | −.07 | −.06 | - | |||||||
| 11.AMEdu | −.03 | −.11* | .07 | −.02 | −.02 | −.13 | −.11 | .05 | −.05 | .24* | - | ||||||
| 12.Risk | .22* | −.21* | .00 | −.06 | −.06 | .10 | −.05 | .10* | −.07 | −.05 | .01 | - | |||||
| 13.Open | .04 | −.04* | .12* | .03 | .03 | .18 | .17 | −.01 | .07 | −.02 | .06 | .02 | - | ||||
| 14.ACSex | −.01 | −.01 | −.05 | .00 | .00 | .04 | .00 | .04 | −.03 | .07 | .04 | .00 | −.06 | - | |||
| 15.ACInt | −.04 | .14* | −.11* | −.07 | −.07 | .09 | .02 | .14* | .15* | −.12* | .06 | −.01 | −.02 | −.06 | - | ||
| 16.ACExt | .01 | .19* | −.09 | −.06 | −.06 | −.01 | .08 | .10* | .14* | −.12* | .07 | .06 | .00 | −.08 | .54* | - | |
| 17.BMTm | −.07 | −.03 | −.03 | −.10 | −.04 | −.14 | −.12 | −.08 | −.06 | .18 | .25* | −.18 | −.17 | .19 | −.03 | −.13 | - |
| M | 2.19 | 9.53 | 2.55 | 3.21 | - | 48.08 | 49.19 | 0.50 | 4.10 | 7.33 | 5.95 | 2.20 | 0.03 | - | 47.45 | 51.94 | - |
| SD | 2.00 | 7.23 | 1.67 | 1.44 | - | 9.73 | 10.52 | 0.49 | 3.29 | 2.05 | 1.22 | 1.30 | 0.93 | - | 8.14 | 8.91 | - |
| Range | 0–7 | 0–37 | 1–7 | 1–6 | 0–1 | 33–71 | 33–76 | 0–3.33 | 0–17 | 1–11 | 2–7 | 0–6 | −2–2 | 0–1 | 33–73 | 33–79 | 0–1 |
Note. BMTr = biological mother trauma, BMDep = biological mother depressive symptoms, BMInc = household income in biological families, BMEdu = biological mother education, BCSex = biological child sex, BCInt = biological child internalizing behaviors, BCExt = biological child externalizing behaviors, AMTr = adoptive mother trauma, AMDep = adoptive mother depressive symptoms, AMInc = household income in adoptive families, AMEdu = adoptive mother education, Risk = perinatal risk, Open = adoption openness, ACSex = adopted child sex, ACInt = adopted child internalizing behaviors, ACExt = adopted child externalizing behaviors, BMTm = biological mother trauma assessment timing.
Mean and standard deviations for child sex and biological mother trauma assessment timing were not provided due to the dichotomous nature of the variables.
p < .05.
Maternal depressive symptoms
Depressive symptoms in both biological and adoptive mothers were assessed using the Beck Depression Inventory (BDI; Beck, Steer, & Brown, 1996). The BDI consists of 21 items, each with a group of statements that describe possible feelings experienced in the past week (e.g., “I do not feel sad,” “I feel sad,” “I am sad all the time and I can’t snap out of it,” “I am so sad or unhappy that I can’t stand it”). Participants were asked to select the statement that best described their feelings in the past week. Biological mothers were assessed at three times (adopted child ages 5 months [a = 0.92], 18 months [a = 0.91], and 54 months [a = 0.90; rs range = .39–.62, p < .001]); adoptive mothers were assessed at six times (adopted child ages 9 months [a = 0.70], 18 months [a = 0.79], 27 months [a = 0.84], 4.5 years [a = 0.82], 6 years [a = 0.82], and 7 years [a = 0.88], rs range = .49–.62, p < .001). BDI scores for each participant were averaged across the individual assessments to create a composite score. Item 9, which assessed suicidal thoughts, was not administered to the first 361 families enrolled into the study because of limited resources for making clinical referrals. The scale composite scores and the reported alphas do not include this item.
Child behaviors
Child internalizing and externalizing behaviors at age 7 years were measured using the Parent version of the Child Behavior Checklist: Ages 6–18 (CBCL; Achenbach & Rescorla, 2001). Parents were asked to indicate whether a series of child behaviors was “not true,” “sometimes true,” or “very true” for their child. Mother and father reports were collected to calculate a mean of both parents’ reports, when both reports were available (EGDS AM–AF pair total: 59.0%; EPoCh BM–BF pair total: 50.8%). We used the standardized internalizing and externalizing T-scores for this study (EGDS internalizing [AM: a = 0.82; AF: a = 0.82]; EPoCh internalizing [BM: a = 0.82; BF: a = 0.84]; EGDS externalizing [AM: a = 0.89; AF: a = 0.89]; EPoCh externalizing [BM: a = 0.90; BF: a = 0.93]).
Control variables
We controlled for SES, child sex, and timing of trauma assessment in EPoCh models, and SES, child sex, perinatal risk, and adoption openness in EGDS models. However, we did not include SES as a control variable in multigroup path analysis models comparing associations across biological and adoptive families (Hypothesis 4) because we were interested in examining its contribution to between-family variation. SES was measured using annual household income (i.e., “What was your total household income from all sources last year?”; range = less than $15,000–greater than $100,000) and maternal education level (i.e., “What is the highest level of education that you have completed?”; range = less than high school degree–graduate program).
Child sex was coded 0 for boys and 1 for girls and was included as a control variable because of potential gender differences in risk for internalizing and externalizing behaviors. For example, several studies have illustrated a greater likelihood of internalizing behaviors among prepubescent boys than among prepubescent girls, with the direction of this association reversed following puberty (Cyranowski, Frank, Young, & Shear, 2000; McGee, Feehan, Williams, & Anderson, 1992). Boys also tend to have higher rates of externalizing behaviors than do girls (Miner & Clarke-Stewart, 2008).
Biological mother report of pregnancy complications (e.g., prenatal illness) was used to assess biological mothers’ perinatal risk at adopted child age 3–6 months, a pregnancy screener was used to assess prenatal drug use, and a pregnancy calendar was used to enhance recall. (Caspi, Moffitt, Newman, & Silva, 1996). Scoring was modified based on the McNeil-Sjöström Scale for Obstetric Complications (see Marceau et al., 2016, and McNeil & Sjöström, 1995, for more details). Responses were assigned a score on a scale of 1 (not harmful or relevant) to 6 (very great harm to or deviation in offspring), indicating level of perinatal risk. Perinatal risk is linked to child developmental outcomes, such as cognitive functions, mental health, and behavior (e.g., Barker, 1990; Coussons-Read, 2013; Irner, 2012; Raznahan, Greenstein, Lee, Clasen, & Giedd, 2012), and was prevalent in our biological mother sample [range: 0–6, M(SD) = 2.20 (1.30)].
We included the timing of assessment of biological mother’s trauma with regards to the biological child’s birth as an additional covariate in the EPoCH models (i.e., those predicting biological child outcomes). This variable was coded 0 if the trauma assessment occurred before the birth of the biological child (11.2% of sample), and 1 if assessment occurred after the birth of the biological child (88.8% of sample), regardless of whether or not the biological mother indicated any exposure to trauma. As previously mentioned, items in which biological mothers endorsed experiencing trauma while pregnant were not included in the final analyses.
Openness in adoption (i.e., contact between biological and adoptive parents) was used to control for similarities between biological parents and adopted children that might have been influenced by contact between the two parties. An adoption design rests on the assumption that similarities between the biological parent and adopted child are the result of genetic factors once intrauterine risk is controlled for, and contact between biological and adoptive families can challenge this assumption and bias model estimates. Adoption openness was measured at adopted child age 3–9 months by using a composite of biological mother, biological father, adoptive mother, and adoptive father ratings of perceived adoption openness (Ge et al., 2008), rated on a 7-point scale ranging from 1 (very closed: “you have no information about the adoptive parents”) to 7 (very open: “you have visits with the family at least once a month and communicate several times a month by phone, letters, or emails”). Interrater agreement based on correlations across the four reporters was high (r range .66–.81, p < .001).
Analytic Plan
The goals of this study were to (a) examine the association between rearing mother trauma and children’s internalizing and externalizing behaviors at child age 7, (b) test whether rearing mother depressive symptoms would mediate the association between rearing mother trauma and child internalizing and externalizing behaviors in both samples, (c) test whether biological mother depressive symptoms would operate as a heritable mechanism of influence that would be associated with adopted child externalizing and internalizing behaviors, and (d) examine whether the direct and mediated associations between rearing mother trauma and child internalizing and externalizing behaviors would be stronger in biological families (biological mother–biological child = BM–BC) than in adoptive families (adoptive mother–adopted child = AM–AC), given the lower SES in biological families. Bivariate analyses were conducted in IBM SPSS version 21.0 for Windows (IBM, 2012). Independent samples t-tests were conducted in SPSS to analyze mean differences in rearing mother trauma frequency, rearing mother depressive symptoms, and child internalizing/externalizing behavior across the two family types (AM–AC and BM–BC dyads). We used path analysis models in Mplus v7 (Muthén & Muthén, 1998–2012) to test the direct and mediated effects of rearing mother trauma frequency on child internalizing and externalizing behavior. Confidence intervals for mediated effects were obtained using the bias-corrected bootstrap resampling method (MacKinnon, Lockwood, & Williams, 2004). Robust maximum likelihood estimation procedures were used to account for any violations of normality.
Model fit was evaluated using multiple global fit indices and examination of residual diagnostics. The criteria for a good fit included a nonsignificant chi-square test statistic, root mean square error of approximation (RMSEA) value less than 0.05, and comparative fit index (CFI) value greater than 0.90. We used multigroup path analyses in Mplus to test whether the key pathways of influence operated similarly across the two samples. Testing involved comparing two nested models: (a) a baseline, fully unconstrained model, and (b) a model in which pathways of interest were systematically constrained to be invariant across the groups. Model fit change was assessed using chi-square difference testing.
Missing data
In the EGDS sample, variables with missing data included biological mother education level (2.0%), household income in biological families (7.9%), biological mother depressive symptoms (1.1%), adoptive mother education level (2.4%), household income in adoptive families (2.2%), adoptive mother trauma (0.9%), adopted child internalizing behaviors (26.6%), and adopted child externalizing behaviors (26.6%). Little’s (1988) missing completely at random (MCAR) test demonstrated that missingness on these variables was completely at random, χ2(17) = 26.77, p = .06. Variables with missing data in EPoCh included biological mother trauma frequency (22.2%), household income (0.8%), and timing of trauma assessment (22.2%). Missingness on biological mother trauma frequency and timing of trauma assessment were present because the trauma measure was not administered to all participants. Little’s MCAR test was used to test whether the missingness on these variables was completely at random, χ2(1) = 3.40, p = .07. Because the study focus was on maternal trauma, we excluded 20 adoptive families in which the father was the primary respondent, which resulted in an EGDS analytic sample size of 541. We used full information maximum likelihood in Mplus to account for missing data.
Results
A correlation matrix of the key study variables is included in Table 3. In the EGDS sample, adopted child internalizing/externalizing behaviors were significantly associated with adoptive mother trauma frequency and adoptive mother depressive symptoms. Household income in adoptive families was negatively correlated with adopted child internalizing and externalizing behaviors. Biological mother depressive symptoms were also significantly associated with adopted child internalizing and externalizing behaviors. In the EPoCh sample, significant bivariate associations were observed between biological child internalizing/externalizing behaviors and biological mother trauma frequency and depressive symptoms.
Independent samples t-tests were conducted to compare mean scores of rearing mother trauma, her depressive symptoms, and child internalizing and externalizing behaviors across the EGDS and EPoCh samples. Biological mothers (M = 2.19, SD = 2.00) reported significantly greater frequency of trauma than did adoptive mothers (M = 0.50, SD = 0.49), t(99) = −8.31, p < .001, and more depressive symptoms (M = 9.53, SD = 7.23) than did adoptive mothers (M = 4.10, SD = 3.29), t(137) = −8.24, p < .001. Adopted children (M = 51.94, SD = 8.91) had significantly higher externalizing scores than did biological children (M = 49.19, SD = 10.52), t(185) = 2.65, p = .009). There were no significant differences in child internalizing scores across the two samples.
Models Predicting Adopted Child Internalizing and Externalizing Behaviors (EGDS)
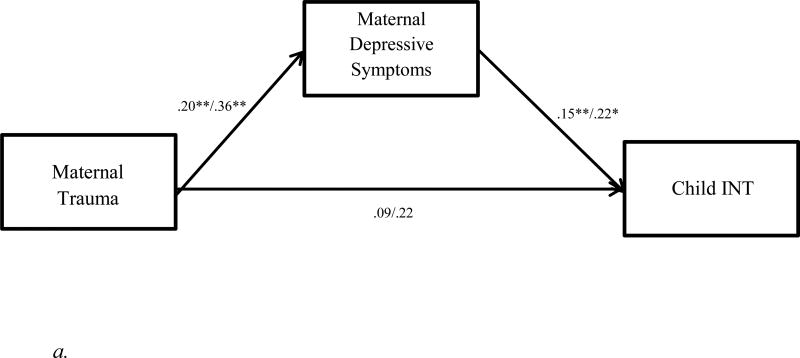
For models examining adopted child internalizing behavior, we observed a significant direct effect of adoptive mother trauma frequency, B(SE) = 2.47 (0.89), p = .005, controlling for household income, maternal education, child sex, perinatal risk, and adoption openness. Adoptive mother depressive symptoms were a significant predictor of child internalizing behavior, B(SE) = 0.36 (0.33), p = .005, and its inclusion as a mediator resulted in the direct effect of adoptive mother trauma becoming nonsignificant, B(SE) = 1.56 (0.97), p = .11. The total mediated effect of adoptive mother trauma on child internalizing behavior was significant, B(95% CI) = 0.49 (0.16, 0.94). In addition, we found significant relationships between child internalizing behavior and household income, B(SE) = −0.47 (0.20), p = .02, and adoptive mother education level, B(SE) = 0.82 (0.35), p = .02. Regression coefficients associated with model pathways are reported in Table 4, and standardized coefficients for the internalizing model are provided in Figure 1a.
Table 4.
Regression Coefficients for Final Models Predicting Child Internalizing and Externalizing Behaviors
| Outcomes | Pathway of influence | B(SE) | β | p |
|---|---|---|---|---|
| AC INT | ||||
| AM Trauma → AC INT | 1.56(0.97) | .09 | .11 | |
| AM Depression → AC INT | 0.36(0.33) | .15 | .005 | |
| BM Depression → AC INT | 0.17(0.05) | .16 | .001 | |
| AM Income → AC INT | −0.47(0.20) | −.12 | .02 | |
| AM Education → AC INT | 0.82(0.35) | .12 | .02 | |
| AC Sex → AC INT | −0.88(0.78) | −.05 | .37 | |
| BM Perinatal Risk → AC INT | −0.24(0.28) | −.05 | .41 | |
| Adoption Openness → AC INT | −0.36(0.44) | −.04 | .44 | |
| AM Trauma → AM Depression | 1.35(0.33) | .20 | < .001 | |
| AM Trauma → AM Depression → AC INT (95%CI) | 0.49 (0.16, 1.03) | |||
| AC EXT | ||||
| AM Trauma → AC EXT | 0.98(0.97) | .05 | .31 | |
| AM Depression → AC EXT | 0.40(0.14) | .15 | .004 | |
| BM Depression → AC EXT | 0.22(0.06) | .20 | < .001 | |
| AM Income → AC EXT | −0.51(0.23) | −.12 | .02 | |
| AM Education → AC EXT | 1.02(0.38) | .14 | .008 | |
| AC Sex → AC EXT | −1.20(0.88) | −.07 | .17 | |
| BM Perinatal Risk → AC EXT | 0.20(0.32) | .03 | .53 | |
| Adoption Openness → AC EXT | −0.22(0.49) | −.02 | .66 | |
| AM Trauma → AM Depression | 1.35(0.33) | .20 | < .001 | |
| AM Trauma → AM Depression → AC EXT (95%CI) | 0.54 (0.16, 1.10) | |||
| BC INT | ||||
| BM Trauma → BC INT | 1.05(0.56) | .22 | .06 | |
| BM Depression → BC INT | 0.29(0.13) | .22 | .02 | |
| BM Income → BC INT | −0.17(0.57) | −.03 | .76 | |
| BM Education → BC INT | −0.94(0.54) | −.14 | .08 | |
| BC Sex → BC INT | −1.73(1.59) | −.09 | .28 | |
| BM Trauma Assessment Timing → BC INT | −5.05(3.05) | −.17 | .10 | |
| BM Trauma → BM Depression | 1.28(0.36) | .36 | < .001 | |
| BM Trauma → BM Depression → BC INT (95% CI) | 0.37 (0.08, 0.89) | |||
| BC EXT | ||||
| BM Trauma → BC EXT | 1.35(0.48) | .26 | .005 | |
| BM Depression → BC EXT | 0.17(0.13) | .11 | .21 | |
| BM Income → BC EXT | −0.34(0.56) | −.05 | .54 | |
| BM Education → BC EXT | −1.03(0.62) | −.14 | .10 | |
| BC Sex → BC EXT | −2.41(1.84) | −.12 | .19 | |
| BM Trauma Assessment Timing → BC EXT | −2.96(3.42) | −.09 | .39 | |
| BM Trauma → BM Depression | 1.28(0.36) | .36 | < .001 | |
| BM Trauma → BM Depression → BC EXT (95% CI) | 0.21 (−0.06, 0.62) |
Note. Bolded pathways indicate statistical significance, p < .05. AM = adoptive mother; AC = adopted child; BM = biological mother; BC = biological child; INT = internalizing behaviors; EXT = externalizing behaviors. Regression estimates reported here are from full models, including all covariates. Separate models were tested for AC INT, AC EXT, BC INT and BC EXT outcomes.
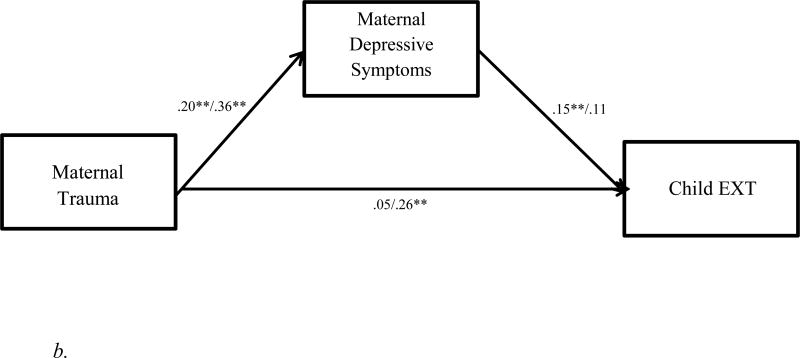
Figure 1.
a. Path analysis model of effects of maternal trauma and depressive symptoms on child internalizing behaviors in EGDS/EPoCh samples (standardized estimates). INT = internalizing behaviors. * p < .05. ** p < .01.
b. Path analysis model of effects of maternal trauma and depressive symptoms on child externalizing behaviors in EGDS/EPoCh samples (standardized estimates). EXT = externalizing behaviors. * p < .05. ** p < .01.
We also examined the effect of biological mother depressive symptoms on adopted child internalizing and externalizing behaviors. In the case of adopted child internalizing behavior, we found a direct effect of biological mother depressive symptoms, B(SE) = 0.17 (0.05), p = .001. The effects of adoptive mother trauma, mediated by her depressive symptoms, remained significant when the effects of biological mother depressive symptoms were included in the model. The model explained 8.8% of the variance associated with child internalizing behavior and had an adequate fit: χ2(6) = 11.45, p = .08; CFI = 0.90; RMSEA (90% CI) = 0.04 (0.00, 0.08).
Adoptive mother trauma was also a significant predictor of child externalizing behavior, B(SE) = 2.05 (0.95), p = .03, controlling for household income, maternal education, child sex, perinatal risk, and adoption openness. When added to the model, adoptive mother depressive symptoms had a significant effect on child externalizing behavior, B(SE) = 0.40 (0.14), p = .004, controlling for household income, maternal education, child sex, perinatal risk, and adoption openness. Furthermore, its inclusion as a mediator resulted in the direct effect of adoptive mother trauma becoming nonsignificant, B(SE) = 0.98 (0.97), p = .31. The total mediated effect of adoptive mother trauma on child externalizing behavior was significant, B(95% CI) = 0.54 (0.16, 1.10). We also found significant relationships between child externalizing behavior and household income, B(SE) = −0.51 (0.23), p = .02, and adoptive mother education level, B(SE) = 1.02 (0.38), p = .008.
Biological mother depressive symptoms were significantly associated with adoptive child externalizing behavior, B(SE) = 0.22 (0.06), p < .001. When including this effect in the full model, the effect of adoptive mother trauma mediated by adoptive mother depressive symptoms still remained significant. Overall, the model explained 10.2% of the variance in child externalizing behavior and had an adequate fit: χ2(6) = 11.38, p = .07; CFI = 0.91; RMSEA (90% CI) = 0.04 (0.00, 0.08).
Models Predicting Biological Child Internalizing and Externalizing Behaviors (EPoCh Sample)
For biological child internalizing behavior, biological mother trauma had a significant direct effect, B(SE) = 1.45 (0.53), p = .006, controlling for the effects of household income, maternal education, child sex, and timing of trauma assessment. Biological mother depressive symptoms were a significant predictor of biological child internalizing behavior, B(SE) = 0.29 (0.13), p = .02, and its inclusion in the model resulted in the direct effect of biological mother trauma becoming nonsignificant, B(SE) = 1.05 (0.56), p = .06, suggesting that the effect of biological mother trauma on child internalizing behavior was mediated by biological mother depressive symptoms. The total mediated effect of biological mother trauma on child internalizing behavior was significant, B(95% CI) = 0.37 (0.08, 0.89). The model explained 18.9% of the variance in child internalizing behavior, and had a good fit: χ2(4) = 2.07, p = .72; CFI = 1.00; RMSEA (90% CI) = 0.00 (0.00, 0.10).
For biological child externalizing behavior, there was a significant direct effect of biological mother trauma, B(SE) = 1.65 (0.47), p < .001, after accounting for effects of household income, maternal education, child sex, and timing of trauma assessment. Biological mother depressive symptoms were not a significant predictor of child externalizing behavior, B(SE) = 0.17 (0.13), p = .21, controlling for the effect of maternal trauma, and did not mediate the effect of trauma on child externalizing behavior (see Table 4). Overall, the model explained 16.2% of the variance in child externalizing behavior and had a good fit: χ2(4) = 1.81, p = .77; CFI = 1.00; RMSEA (90% CI) = 0.00 (0.00, 0.09). Standardized coefficients for the externalizing model are provided in Figure 1b.
Multigroup Path Analysis
To test if the pathways of influence operated similarly across the two samples, we tested multigroup models with sample type (EGDS vs. EPoCh) as the grouping variable. We controlled for child sex in the multigroup model. The key pathways of influence, i.e., the direct effect of rearing mother trauma on child internalizing/externalizing behavior and the mediated pathway involving rearing mother depressive symptoms, were constrained to be equal across the two groups. Examination of model fit for the unconstrained and constrained models suggested a nonsignificant drop in model fit for internalizing behavior (Δχ2 = 0.814, df = 3; p = .85) and externalizing behavior (Δχ2 = 0.299, df = 3; p = .96), suggesting that the magnitude of the associations between rearing mother trauma, rearing mother depressive symptoms, and child internalizing and externalizing behaviors was similar across the two samples.
Discussion
Using a parent–child adoption design that included linked biological mother–biological child dyads, we sought to examine environmental and biological mechanisms underlying associations from maternal trauma, to maternal depressive symptoms, to child internalizing and externalizing behaviors at age 7. We found evidence for the environmental transmission hypothesis whereby the association between maternal trauma and child internalizing and externalizing behavior was significant in cases of mother–child dyads living together, and in particular, among dyads with no shared genetic influences (i.e., AM–AC dyads). The effect of maternal trauma was mediated by rearing mother depressive symptoms, with the exception of the effect of maternal trauma on child externalizing behavior in BM–BC dyads. In this model, biological mother depressive symptoms were significantly associated with her exposure to trauma and the biological child’s externalizing behavior, respectively, but failed to predict child externalizing behavior when included in combination with maternal trauma, possibly because of competing effects. It is possible that other variables not included in our models, such as negative parenting, may be stronger mediators of the effects of maternal trauma.
Overall, the findings were significant when controlling for the effects of household income, maternal education, and child sex in both samples, in addition to controlling for openness in adoption and perinatal risk in adoptive families and timing of trauma assessment in biological families. Given our novel adoption design, we were also able to control for the confounding effects of passive rGE in our AM–AC models. In addition, the presence of significant associations between biological mother depressive symptoms and adopted child internalizing and externalizing behaviors suggests a heritable transmission of risk. This finding is consistent with those from previous studies (Natsuaki et al., 2014), and suggests both heritable and environmental transmission mechanisms from maternal depressive symptoms to child internalizing and externalizing behaviors.
The positive association between maternal depressive symptoms and child internalizing and externalizing behaviors is consistent with findings reported in the literature (e.g., Cicchetti & Toth, 1995; Cicchetti & Toth, 1998b; Cummings & Davies, 1994; Kovacs & Devlin, 1998). Because of the overlapping operational definitions of depressive symptoms and internalizing behaviors, it is not surprising that rearing mothers’ internalizing symptoms tend to be related to children’s internalizing behaviors cross-generationally (Kim, Capaldi, Pears, Kerr, & Owens, 2009). In addition, longitudinal studies suggest that children of depressed mothers have an increased risk for depressive symptoms through other environmental risk factors, such as marital conflict, stress, and compromised parenting (Natsuaki et al., 2014; Weissman et al., 2006).
Maternal depression has also been linked to child emotional and behavioral adjustment through interruption of attachment between mother and child (Cicchetti et al., 1998; Cohn & Tronick, 1989). Although not directly examined in our study, children raised by mothers who are distant, rejecting, or inconsistent in their parenting as a consequence of their traumatic past and associated depressive symptoms are more likely to develop an insecure attachment (Iyengar, Kim, Martinez, Fonagy, & Strathearn, 2014), which in turn increases their risk for internalizing and externalizing behaviors (Cowan, Cowan, Cohn, & Pearson, 1996; Groh, Fearon, van Ijzendoorn, Bakermans-Kranenburg, & Roisman, 2017).
Parents can play an important role in the development of a child’s emotion regulation strategies through modeling (e.g., Cassidy, 1994). A parent who experiences depressive symptoms as a result of exposure to trauma is more likely to neglect or reject a child’s distress signals, perpetuating a stressful emotional state in the child. In such a scenario, the child may have difficulty developing internal strategies to modulate emotions in response to the distress (Izard & Kobak, 1991), which may manifest in the form of internalizing or externalizing behavior (Cicchetti, Toth, Cole, & Zahn-Waxler, 1992). It is also possible that children adapt to an unresponsive parent by developing coping strategies that may be maladaptive in other settings. Externalizing behaviors, for instance, may be a way to elicit attention from a depressed caregiver (Hersen & Thomas, 2007). Externalizing behaviors may also be an outcome of the social learning process, wherein a child who witnesses a traumatic event (e.g., domestic violence) may be more likely to model aggressive behaviors in other contexts (Campbell, Woods, Chouaf, & Parker, 2000).
We also found evidence for a heritable pathway of influence through biological mother depressive symptoms. Specifically, adopted children with biological mothers who reported higher levels of depressive symptoms had significantly higher levels of internalizing and externalizing behaviors, even after controlling for the effects of adoptive mother trauma and depressive symptoms. This biological pathway is important in that some children may be more susceptible to the negative effects of maternal trauma and depressive symptoms because of their inherited propensities. In other words, the combined environmental exposure to maternal trauma and heritable risk for depressive symptoms may place some children at greater risk for developing internalizing or externalizing behaviors. This is consistent with prior research that has demonstrated that children of mothers with comorbid symptoms of trauma and depression are significantly more likely to display internalizing and externalizing behaviors than are children of mothers with depression only (Chemtob et al., 2010).
Interestingly, we found that adoptive mothers in our sample reported higher rates of externalizing behaviors in their adopted children than biological mothers reported about their biological children. This may be because externalizing behaviors (e.g., aggression) are easier to observe than internalizing behaviors (e.g., social withdrawal, depressive symptoms), and thus may be overreported by adoptive mothers who may be more vigilant to their child’s behaviors. Adoptive mothers may also be more likely to perceive disruptive behaviors in their children as more problematic than biological mothers do. Similar trends have been observed in studies of parent–child conflict in adoptive families, in which parents reported their adopted child to be more conflictual than their nonadopted child (Reuter, Keyes, Iacono, & McGue, 2009).
Regardless of the differences in the levels of risk across the two samples, with biological mothers reporting significantly greater trauma exposure and depressive symptoms and lower SES, our findings indicated that the strength of the relationships between rearing mother trauma, rearing mother depressive symptoms, and child externalizing and internalizing behaviors was consistent across samples. This finding runs counter to our hypothesis that children in more adverse, low-SES environments with higher exposure to trauma would be more strongly affected by maternal trauma. Instead, our findings suggest that associations between rearing mother trauma and child internalizing and externalizing behaviors are present across all levels of SES. Our findings also indicate that trauma exposure and associated depressive symptoms can have a negative impact on child internalizing and externalizing behaviors, regardless of whether trauma involves a single incident or multiple exposures. The findings suggest that early interventions targeting both parents and children in the family system, and not just the behaviors of the children, may be beneficial in preventing longer term individual and intergenerational consequences. Research and clinical prevention work could benefit from a better understanding of the rearing environment influences in addition to the biological mechanisms of influence of maternal depressive symptoms.
Limitations
The following limitations should be noted when interpreting the results. First, although our study included a large sample of adopted children, our sample of biological children was relatively small (n = 126) because of ongoing data collection for the EPoCh study. This may have affected our ability to detect mediational effects of maternal depressive symptoms in the model predicting biological child externalizing behavior. Second, although we matched items across scales to similarly assess maternal trauma in biological and adoptive mothers, the two scale scores were not perfectly correlated. In the case of biological mothers, lifetime trauma was assessed using phone interviews, but for adoptive mothers, trauma was assessed over a period of 6.25 years using self-report surveys. In addition, minor variations in the specific wording of questions may have created unintended measurement differences between the two samples. We also did not have measures of trauma type (e.g., interpersonal vs. non-interpersonal) or posttraumatic stress disorder symptoms, which may have revealed a more nuanced understanding of the biological and environmental effects of maternal trauma on child internalizing and externalizing behavior (Chemtob et al., 2010). Third, informant bias may have been an issue given that maternal trauma, maternal depressive symptoms, and child behavior problems were reported by the same individual, that is, either the biological or adoptive mother. We attempted to mitigate this limitation by using a combined mother–father rating of child behavior, when data from fathers were available. In addition, maternal depressive symptoms could have heightened the tendency of mothers to over-report past trauma and child behavior problems (Colman et al., 2016; Gartstein, Bridgett, Dishion, & Kaufman, 2009; Richters & Pellegrini, 1989). Given the mean differences in depressive symptoms in our two samples, this potential bias may have disproportionately affected our BM–BC models. Finally, recent studies have called into question the validity of adult self-reports of childhood adversity (e.g., Reuben et al., 2016), which could have been an issue in the maternal self-reports of trauma in our study.
Future Directions
Research that has examined the effects of maternal trauma on child behavioral outcomes has typically measured trauma retrospectively. Future studies could benefit from incorporating a mixture of additional subjective and objective methods to supplement self-report records of maternal trauma exposure and depressive symptoms, such as clinical assessments, physiological measures, and/or multiple informants. Similarly, a multi-informant approach would strengthen the measurement of child behavioral outcomes (e.g., teacher reports of child behavior). It would also be beneficial to assess these pathways longitudinally and at younger ages, given that internalizing and externalizing behaviors tend to be relatively stable from toddlerhood and beyond (e.g., Pierce, Ewing, & Campbell, 1999). Our study examined maternal depressive symptoms as one biological and environmental mechanism in the intergenerational influence of maternal trauma. Other potential mediators, such as parenting behaviors and caregiving quality, should be examined to better understand the environmental mechanisms of influence of maternal trauma.
A useful next step for research would be to explore other gene–environment influences, such as gene–environment interaction and evocative rGE. Longitudinal studies observing nontwin siblings or, to extend our current design, nonrelated (e.g., adopted and nonadopted) siblings raised in the same environment, may provide insights about how children with dissimilar genes but exposed to the same early environmental adversity may or may not differ in their internalizing and externalizing behavioral outcomes. Finally, intergenerational transmission of trauma and its consequences should be examined through an epigenetics lens to better understand heritable and environmental pathways underlying the development of psychopathology (Cicchetti, 2016).
Acknowledgments
This project was supported by grant R01 and R56 HD042608 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development and NIDA, NIH, U.S. PHS; R01 DA020585 from NIDA, NIMH, and OBSSR, NIH, U.S. PHS; R01 MH092118 from NIMH, and R01 DA035062 from NIDA. Additional support for the writing of this report was provided by P50 DA035763, NIDA and by 1UG3 OD023389, Office of the Director, U.S. PHS. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Child Health & Human Development or the National Institutes of Health. We would like to thank the birth parents and adoptive families who participated in this study and the adoption agencies who helped with the recruitment of study participants. We would also like to thank the EGDS team for their work with participants, especially the contributions of data manager Sally Guyer. We gratefully acknowledge Rand Conger and Laura Scaramella who contributed to the larger study.
References
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- Barker DJ. The fetal and infant origins of adult disease. BMJ. 1990;301:1111. doi: 10.1136/bmj.301.6761.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory–II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Bifulco A, Moran PM, Ball C, Bernazzani O. Adult attachment style: Its relationship to clinical depression. Social Psychiatry and Psychiatric Epidemiology. 2002;37:50–59. doi: 10.1007/s127-002-8215-0. doi: http://dx.doi.org/10.1007/s127-002-8215-0. [DOI] [PubMed] [Google Scholar]
- Campbell JC, Woods AB, Chouaf KL, Parker B. Reproductive health consequences of intimate partner violence: A nursing research review. Clinical Nursing Research. 2000;9:217–237. doi: 10.1177/10547730022158555. doi: http://dx.doi.org/10.1177/10547730022158555. [DOI] [PubMed] [Google Scholar]
- Caspi A, Moffitt TE, Newman DL, Silva PA. Behavioral observations at age 3 years predict adult psychiatric disorders: Longitudinal evidence from a birth cohort. Archives of General Psychiatry. 1996;53:1033–1039. doi: 10.1001/archpsyc.1996.01830110071009. [DOI] [PubMed] [Google Scholar]
- Cassidy J. The development of emotion regulation: Biological and behavioral considerations. Monographs of the Society for Research in Child Development. 1994;59:228–249. doi: 10.1111/j.1540-5834.1994.tb01287.x. [DOI] [PubMed] [Google Scholar]
- Chemtob CM, Nomura Y, Rajendran K, Yehuda R, Schwartz D, Abramowitz R. Impact of maternal posttraumatic stress disorder and depression following exposure to the September 11 attacks on preschool children’s behavior. Child Development. 2010;81:1129–1141. doi: 10.1111/j.1467-8624.2010.01458.x. doi: http://dx.doi.org/10.1111/j.1467-8624.2010.01458.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D. Introduction to the special section. Development and Psychopathology. 2016;28:1217–1217. doi: 10.1017/S0954579416000791. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Toth SL. Maternal depressive disorder and contextual risk: Contributions to the development of attachment insecurity and behavior problems in toddlerhood. Developmental Psychopathology. 1998;10:283–300. doi: 10.1017/s0954579498001618. doi: http://dx.doi.org/10.1017/S0954579498001618. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL. Developmental psychopathology and disorders of affect. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology: Vol. 2. Risk, disorder, and adaptation. New York, NY: Wiley; 1995. pp. 369–420. [Google Scholar]
- Cicchetti D, Toth SL. Perspectives on research and practice in developmental psychopathology. In: Damon W, Sigel IE, Renninger KA, editors. Handbook of child psychology. Vol. 4: Child psychology in practice. New York, NY: John Wiley & Sons, Inc.; 1998a. pp. 479–583. [Google Scholar]
- Cicchetti D, Toth SL. The development of depression in children and adolescents. American Psychologist. 1998b;53:221–241. doi: 10.1037//0003-066x.53.2.221. doi: http://dx.doi.org/10.1037/0003-066X.53.2.221. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL, Cole PM, Zahn-Waxler C. Emotional dysregulation in disruptive behavior disorders. In: Cicchetti D, Toth SL, editors. Rochester symposium on developmental psychopathology: Vol 4. Developmental perspectives on depression. Rochester, NY: University of Rochester; 1992. pp. 173–210. [Google Scholar]
- Class AQ, D’Onforio BM, Singh AL, Ganiban JM, Spotts EL, Lichtenstein P, Neiderhiser JM. Current parental depression and offspring perceived self-competence: A quasi-experimental examination. Behavioral Genetics. 2012;42:787–797. doi: 10.1007/s10519-012-9550-1. doi: http://dx.doi.org/10.1007/s10519-012-9550-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohn JF, Tronick E. Specificity of infants’ response to mothers’ affective behavior. Journal of the American Academy of Child and Adolescent Psychiatry. 1989;28:242–248. doi: 10.1097/00004583-198903000-00016. doi: http://dx.doi.org/10.1097/00004583-198903000-00016. [DOI] [PubMed] [Google Scholar]
- Colman I, Kingsbury M, Garad Y, Zeng Y, Naicker K, Pattern S, Thompson AH. Consistency in adult reporting of adverse childhood experiences. Psychological Medicine. 2016;46:543–549. doi: 10.1017/S0033291715002032. doi: http://dx.doi.org/10.1017/S0033291715002032. [DOI] [PubMed] [Google Scholar]
- Coussons-Read ME. Effects of prenatal stress on pregnancy and human development: Mechanisms and pathways. Obstetric Medicine: The Medicine of Pregnancy. 2013;6:52–57. doi: 10.1177/1753495X12473751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowan PA, Cowan CP, Cohn DA, Pearson JL. Parents’ attachment histories and children’s externalizing and internalizing behaviors: Exploring family systems models of linkage. Journal of Consulting and Clinical Psychology. 1996;64:53–63. doi: 10.1037//0022-006x.64.1.53. doi: http://dx.doi.org/10.1037/0022-006X.64.1.53. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Davies PT. Maternal depression and child development. Journal of Child Psychology and Psychiatry. 1994;35:73–112. doi: 10.1111/j.1469-7610.1994.tb01133.x. doi: http://dx.doi.org/10.1111/j.1469-7610.1994.tb01133.x. [DOI] [PubMed] [Google Scholar]
- Cyranowski JM, Frank E, Young E, Shear MK. Adolescent onset of the gender difference in lifetime rates of major depression: A theoretical model. Archives of General Psychiatry. 2000;57:21–27. doi: 10.1001/archpsyc.57.1.21. doi: http://dx.doi.org/10.1001/archpsyc.57.1.21. [DOI] [PubMed] [Google Scholar]
- Danese A, Moffitt TE, Harrington H, Milne BJ, Polanczyk G, Pariante CM, Caspi A. Adverse childhood experiences and adult risk factors for age-related disease: Depression, inflammation, and clustering of metabolic risk markers. Archives of Pediatric and Adolescent Medicine. 2009;163:1135–1143. doi: 10.1001/archpediatrics.2009.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dohrenwend BS, Krasnoff L, Askenasy AR, Dohrenwend BP. Exemplification of method for scaling life events: The PERI life events scale. Journal of Health and Social Behavior. 1978;19:205–229. [PubMed] [Google Scholar]
- Dubowitz H, Black MM, Kerr M, Hussey J, Morrel T, Everson M, Starr RH. Type and timing of mothers’ victimization: Effects on mothers and children. Pediatrics. 2001;107:728–735. doi: 10.1542/peds.107.4.728. [DOI] [PubMed] [Google Scholar]
- Felsen I. Transgenerational transmission of effects of the Holocaust: The North American research perspective. In: Danieli Y, editor. International handbook of multigenerational legacies of trauma. New York & London: Plenum Press; 1998. pp. 43–68. doi: http://dx.doi.org/10.1007/978-1-4757-5567-1_3. [Google Scholar]
- Felsen I. Adult-onset trauma and intergenerational transmission: Integrating empirical data and psychoanalytic theory. Psychoanalysis, Self and Context. 2017;12:60–77. http://dx.doi.org/10.1080/15551024.2017.1251185. [Google Scholar]
- Ferentinos P, Koukounari A, Power R, Rivera M, Uher R, Craddock N, Lewis CM. Familiality and SNP heritability of age at onset and episodicity in major depressive disorder. Psychological Medicine. 2015;45:2215–2225. doi: 10.1017/S0033291715000215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraiberg S, Adelson E, Shapiro V. Ghosts in the nursery: A psychoanalytic approach to the problems of impaired infant-mother relationships. Journal of the American Academy of Child and Adolescent Psychiatry. 1975;14:387–421. doi: 10.1016/s0002-7138(09)61442-4. https://doi.org/10.1016/S0002-7138(09)61442-4. [DOI] [PubMed] [Google Scholar]
- Gartstein MA, Bridgett DJ, Dishion TJ, Kaufman NK. Depressed mood and maternal report of child behavior problems: Another look at the depression-distortion hypothesis. Journal of Applied Developmental Psychology. 2009;30:149–160. doi: 10.1016/j.appdev.2008.12.001. doi: http://dx.doi.org/10.1016/j.appdev.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ge X, Natsuaki MN, Martin DM, Leve LD, Neiderhiser JM, Shaw DS, Reiss D. Bridging the divide: Openness in adoption and postadoption psychosocial adjustment among birth and adoptive parents. Journal of Family Psychology. 2008;22:529–540. doi: 10.1037/a0012817. doi: http://dx.doi.org/10.1037/a0012817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH. Children of depressed parents: Mechanisms of risk and implications for treatment. Washington, DC: American Psychological Association; 2002. [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review. 2011;14:1–27. doi: 10.1007/s10567-010-0080-1. doi: http://dx.doi.org/10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- Greeson JK, Briggs EC, Layne CM, Belcher HM, Ostrowski SA, Kim S, Fairbank JA. Traumatic childhood experiences in the 21st century: Broadening and building on the ACE studies with data from the National Child Traumatic Stress Network. Journal of Interpersonal Violence. 2014;29:536–556. doi: 10.1177/0886260513505217. doi: http://dx.doi.org/10.1177/0886260513505217. [DOI] [PubMed] [Google Scholar]
- Groh AM, Fearon RM, van Ijzendoorn MH, Bakermans-Kranenburg MJ, Roisman GI. Attachment in the early life course: Meta-analytic evidence for its role in socioemotional development. Child Development Perspectives. 2017;11:70–76. doi: http://dx.doi.org/10.1111/cdep.12213. [Google Scholar]
- Harold GT, Rice F, Hay DF, Boivin J, van den Bree M, Thapar A. Familial transmission of depression and antisocial behavior symptoms: Disentangling the contribution of inherited and environmental factors and testing the mediation role of parenting. Psychological Medicine. 2011;41:1175–1185. doi: 10.1017/S0033291710001753. doi: http://dx.doi.org/10.1017/S0033291710001753. [DOI] [PubMed] [Google Scholar]
- Hersen M, Thomas JC. Handbook of clinical interviewing with children. Los Angeles, CA: SAGE Publications; 2007. [Google Scholar]
- IBM Corporation. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp.; 2012. [Google Scholar]
- Irner TB. Substance exposure in utero and developmental consequences in adolescence: A systematic review. Child Neuropsychology: A Journal on Normal and Abnormal Development in Childhood and Adolescence. 2012;18:521–549. doi: 10.1080/09297049.2011.628309. doi: http://dx.doi.org/10.1080/09297049.2011.628309. [DOI] [PubMed] [Google Scholar]
- Iyengar U, Kim S, Martinez S, Fonagy P, Strathearn L. Unresolved trauma in mothers: Intergenerational effects and the role of reorganization. Frontiers in Psychology. 2014;5:20–28. doi: 10.3389/fpsyg.2014.00966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izard C, Kobak R. Emotions system functioning and emotion regulation. In: Garber J, Dodge K, editors. The development of affect regulation. New York, NY: Cambridge University Press; 1991. pp. 303–321. doi: http://dx.doi.org/10.1017/CBO9780511663963.014. [Google Scholar]
- Jaffee SR, Price TS. Gene-environment correlations: A review of the evidence and implications for prevention of mental illness. Molecular Psychiatry. 2007;12:432–442. doi: 10.1038/sj.mp.4001950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kellermann NP. Transmission of Holocaust trauma - An integrative view. Israel Journal of Psychiatry. 2001;64:256–267. doi: 10.1521/psyc.64.3.256.18464. doi: http://dx.doi.org/10.1521/psyc.64.3.256.18464. [DOI] [PubMed] [Google Scholar]
- Kerr DC, Leve LD, Harold GT, Natsuaki MN, Neiderhiser JM, Shaw DS, Reiss D. Influences of biological and adoptive mothers’ depression and antisocial behavior on adoptee’s early behavior trajectories. Journal of Abnormal Child Psychology. 2013;41:723–734. doi: 10.1007/s10802-013-9711-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HK, Capaldi DM, Pears KC, Kerr DC, Owen LD. Intergenerational transmission of internalising and externalising behaviours across three generations: Gender-specific pathways. Criminal Behaviour and Mental Health. 2009;19:125–141. doi: 10.1002/cbm.708. doi: http://dx.doi.org/10.1002/cbm.708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinderman P, Schwannauer M, Pontin E, Tai S. Psychological processes mediate the impact of familial risk, social circumstances and life events on mental health. PLoS ONE. 2013;8:e76564. doi: 10.1371/journal.pone.0076564. doi: http://dx.doi.org/10.1371/journal.pone.0076564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinsella MT, Monk C. Impact of maternal stress, depression and anxiety on fetal neurobehavioral development. Clinical Obstetrics Gynecology. 2009;52:425–440. doi: 10.1097/GRF.0b013e3181b52df1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein-Parker F. Dominant attitudes of adult children of Holocaust survivors toward their parents. In: Wilson JP, Kahana B, editors. Human Adaptation to Extreme Stress. New York, NY: Plenum; 1988. pp. 193–217. [Google Scholar]
- Kovacs M, Devlin B. Internalizing disorders in childhood. Journal of Child Psychology and Psychiatry. 1998;39:47–63. doi: http://dx.doi.org/10.1017/S0021963097001765. [PubMed] [Google Scholar]
- Kovacs M, Devlin B, Pollock M, Mukerji P. A controlled family history study of childhood-onset depressive disorder. Archives of General Psychiatry. 1997;54:613–623. doi: 10.1001/archpsyc.1997.01830190033004. doi: http://dx.doi.org/10.1001/archpsyc.1997.01830190033004. [DOI] [PubMed] [Google Scholar]
- Krauss LA, Wilson CK, Padrón E, Samuelson KW. Maternal trauma and children’s functioning: The role of kinship social support. Journal of Aggression, Maltreatment & Trauma. 2016;25:421–435. doi: http://dx.doi.org/10.1080/10926771.2016.1145161. [Google Scholar]
- Lambert JE, Holzer J, Hasbun A. Association between parents’ PTSD severity and children’s psychological distress: A meta-analysis. Journal of Traumatic Stress. 2014;27:9–17. doi: 10.1002/jts.21891. doi: http://dx.doi.org/10.1002/jts.21891. [DOI] [PubMed] [Google Scholar]
- Leve LD, Neiderhiser JM, Harold GT, Natsuaki MN, Bohannan BJ, Cresko WA. Naturalistic experimental designs as tools for understanding the role of genes and the environment in prevention research. Prevention Science. 2017 doi: 10.1007/s11121-017-0746-8. [ePub ahead of print]. doi: http://dx.doi.org/10.1007/s11121-017-0746-8. [DOI] [PMC free article] [PubMed]
- Leve LD, Neiderhiser JM, Shaw DS, Ganiban J, Natsuaki MN, Reiss D. The Early Growth and Development Study: A prospective adoption study from birth through middle childhood. Twin Research and Human Genetics. 2013;16:412–423. doi: 10.1017/thg.2012.126. doi: http://dx.doi.org/10.1017/thg.2012.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little RJ. A test of missing completely at random for multivariate data with missing values. Journal of the American Statistical Association. 1988;83:1198–1202. [Google Scholar]
- Lorant V, Deliege D, Eaton W. Socioeconomic inequalities in depression: A meta-analysis. American Journal of Epidemiology. 2003;157:98–112. doi: 10.1093/aje/kwf182. doi: https://doi.org/10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- Loukas A, Piejak LA, Bingham CR, Fitzgerald HE, Zucker RA. Parental distress as a mediator of problem behaviors in sons of alcohol-involved families. Family Relations. 2001;50:293–301. doi: http://dx.doi.org/10.1111/j.1741-3729.2001.00293.x. [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect. Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. doi: http://dx.doi.org/10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marceau K, De Araujo-Greecher M, Miller ES, Massey SH, Mayes LC, Ganiban JM, Neiderhiser JM. The Perinatal Risk Index: Early risks experienced by domestic adoptees in the United States. PLOS One. 2016;11(3):e150486. doi: 10.1371/journal.pone.0150486. doi.org/10.1371/journal.pone.0150486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayou RA, Bryant BM, Ehlers A. Prediction of psychological outcomes one year after a motor vehicle accident. The American Journal of Psychiatry. 2001;158:1231–1238. doi: 10.1176/appi.ajp.158.8.1231. doi: http://dx.doi.org/10.1176/appi.ajp.158.8.1231. [DOI] [PubMed] [Google Scholar]
- McGee R, Feehan M, Williams S, Anderson J. DSM-III disorders from age 11 to age 15 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:50–59. doi: 10.1097/00004583-199201000-00009. doi: http://dx.doi.org/10.1097/00004583-199201000-00009. [DOI] [PubMed] [Google Scholar]
- McGuffin P, Katz R. The genetics of depression and manic-depressive disorder. British Journal of Psychiatry. 1989;155:294–304. doi: 10.1192/bjp.155.3.294. [DOI] [PubMed] [Google Scholar]
- McNeil TF, Sjostrom K. The McNeil-Sjostrom Scale for Obstetric Complications. Malmo, Sweden: Department of Psychiatry, University Hospital, Lund University; 1995. [Google Scholar]
- Min MO, Singer LT, Minnes S, Kim H, Short E. Mediating links between maternal childhood trauma and preadolescent behavioral adjustment. Journal of Interpersonal Violence. 2013;28:831–851. doi: 10.1177/0886260512455868. doi: http://dx.doi.org/10.1177/0886260512455868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miner JL, Clarke-Stewart A. Trajectories of externalizing behaviour from age 2 to age 9: Relations with gender, temperament, ethnicity, parenting, and rater. Developmental Psychology. 2008;44:771–786. doi: 10.1037/0012-1649.44.3.771. doi: http://dx.doi.org/10.1037/0012-1649.44.3.771. [DOI] [PubMed] [Google Scholar]
- Murray L, Halligan SL, Adams G, Patterson P, Goodyer IM. Socioemotional development in adolescents at risk for depression: The role of maternal depression and attachment style. Development and Psychopathology. 2006;18:489–516. doi: 10.1017/S0954579406060263. doi: https://doi.org/10.1017/S0954579406060263. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user's guide. 6. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- Natsuaki MN, Shaw DS, Neiderhiser JM, Ganiban JM, Harold GT, Reiss D, Leve LD. Raised by depressed parents: Is it an environmental risk? Clinical Child and Family Psychology Review. 2014;17:357–367. doi: 10.1007/s10567-014-0169-z. doi: http://dx.doi.org/10.1007/s10567-014-0169-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris FH. Screening for traumatic stress: A scale of use in the general population. Journal of Applied Social Psychology. 1990;20:1704–1718. doi: http://dx.doi.org/10.1111/j.1559-1816.1990.tb01505.x. [Google Scholar]
- O'Connor TG, Heron J, Golding J, Beveridge M, Glover V. Maternal antenatal anxiety and children's behavioural/emotional problems at 4 years: Report from the Avon Longitudinal Study of Parents and Children. The British Journal of Psychiatry. 2002;180(6):502–508. doi: 10.1192/bjp.180.6.502. doi: http://dx.doi.org/10.1192/bjp.180.6.502. [DOI] [PubMed] [Google Scholar]
- O’Donnell ML, Creamer M, Pattison P, Atkin C. Psychiatric morbidity following injury. The American Journal of Psychiatry. 2004;161:507–514. doi: 10.1176/appi.ajp.161.3.507. doi: http://dx.doi.org/10.1176/appi.ajp.161.3.507. [DOI] [PubMed] [Google Scholar]
- Pawlby S, Hay DF, Sharp D, Waters CS, O’Keane V. Antenatal depression predicts depression in adolescent offspring: Prospective longitudinal community-based study. Journal of Affective Disorders. 2009;113:236–243. doi: 10.1016/j.jad.2008.05.018. doi: http://dx.doi.org/10.1016/j.jad.2008.05.018. [DOI] [PubMed] [Google Scholar]
- Pemberton CK, Neiderhiser JM, Leve LD, Natsuaki MN, Shaw DS, Reiss D, Ge X. Influence of parental depressive symptoms on adopted toddler behaviors: An emerging developmental cascade of genetic and environmental effects. Development and Psychopathology. 2010;22:803–818. doi: 10.1017/S0954579410000477. doi: http://dx.doi.org/10.1017/S0954579410000477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce EW, Ewing LJ, Campbell SB. Diagnostic status and symptomatic behavior of hard-to-manage preschool children in middle childhood and early adolescence. Journal of Clinical Child Psychology. 1999;28:44–57. doi: 10.1207/s15374424jccp2801_4. doi: http://dx.doi.org/10.1207/s15374424jccp2801_4. [DOI] [PubMed] [Google Scholar]
- Price TS, Jaffee SR. Effects of the family environment: Gene-environment interaction and passive gene-environment correlation. Developmental Psychology. 2008;44:305–315. doi: 10.1037/0012-1649.44.2.305. doi: http://dx.doi.org/10.1037/0012-1649.44.2.305. [DOI] [PubMed] [Google Scholar]
- Raznahan A, Greenstein D, Lee NR, Clasen LS, Giedd JN. Prenatal growth in humans and postnatal brain maturation into late adolescence. Proceedings of the National Academy of Sciences. 2012;109:11366–11371. doi: 10.1073/pnas.1203350109. doi: http://dx.doi.org/10.1073/pnas.1203350109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reich W, Earls F, Powell J. A comparison of the home and social environments of children of alcoholic and non-alcoholic parents. British Journal of Addiction. 1988;83:831–839. doi: 10.1111/j.1360-0443.1988.tb00518.x. doi: http://dx.doi.org/10.1111/j.1360-0443.1988.tb00518.x. [DOI] [PubMed] [Google Scholar]
- Reuben A, Moffitt TE, Caspi A, Belsky DW, Harrington H, Schroeder F, Danese A. Lest we forget: Comparing retrospective and prospective assessments of adverse childhood experiences in the prediction of adult health. Journal of Child Psychology and Psychiatry. 2016;57:1103–1112. doi: 10.1111/jcpp.12621. doi: http://dx.doi.org/10.1111/jcpp.12621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reuter MA, Keyes MA, Iacono WG, McGue M. Family interactions in adoptive compared to nonadoptive families. Journal of Family Psychology. 2009;23:58–66. doi: 10.1037/a0014091. doi: http://dx.doi.org/10.1037/a0014091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice F, Harold G, Thapar A. The genetic aetiology of childhood depression: A review. Journal of Child Psychology and Psychiatry. 2002;43:65–79. doi: 10.1111/1469-7610.00004. doi: http://dx.doi.org/10.1111/1469-7610.00004. [DOI] [PubMed] [Google Scholar]
- Richters J, Pellegrini D. Depressed mothers’ judgment about their children: An examination of depression-distortion hypothesis. Child Development. 1989;50:1068–1075. doi: 10.2307/1130780. [DOI] [PubMed] [Google Scholar]
- Schwerdtfeger KL, Goff BS. Intergenerational transmission of trauma: Exploring mother-infant prenatal attachment. Journal of Traumatic Stress. 2007;20:39–51. doi: 10.1002/jts.20179. doi: http://dx.doi.org/10.1002/jts.20179. [DOI] [PubMed] [Google Scholar]
- Scott KM, Smith DR, Ellis PM. Prospectively ascertained child maltreatment and its association with DSM-IV mental disorders in young adults. Archives of General Psychiatry. 2010;67:712–719. doi: 10.1001/archgenpsychiatry.2010.71. doi: http://dx.doi.org/10.1001/archgenpsychiatry.2010.71. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Dishion TJ, Connell A, Wilson MN, Gardner F. Improvements in maternal depression as a mediator of intervention effects on early child problem behavior. Development and Psychopathology. 2009;21:417–439. doi: 10.1017/S0954579409000236. doi: http://dx.doi.org/10.1017/S0954579409000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silberg J, Maes H, Eaves LJ. Genetic and environmental influences on the transmission of parental depression to children’s depression and conduct disturbance: An extended children of twins study. The Journal of Child Psychology and Psychiatry. 2010;51:734–744. doi: 10.1111/j.1469-7610.2010.02205.x. doi: http://dx.doi.org/10.1111/j.1469-7610.2010.02205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh AL, D’Onforio BM, Slutske WS, Turkheimer E, Emery RE, Harden KP, Martin NG. Parental depression and offspring psychopathology: A children of twins study. Psychological Medicine. 2011;41:1385–1395. doi: 10.1017/S0033291710002059. doi: http://dx.doi.org/10.1017/S0033291710002059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sotero MA. A conceptual model of historical trauma: Implications for public health practice and research. Journal of Health Disparities Research and Practice. 2006;1:93–108. [Google Scholar]
- Sullivan PF, Neale MC, Kendler KS. Genetic epidemiology of major depression: Review and meta-analysis. American Journal of Psychiatry. 2000;157:1552–1562. doi: 10.1176/appi.ajp.157.10.1552. doi: http://dx.doi.org/10.1176/appi.ajp.157.10.1552. [DOI] [PubMed] [Google Scholar]
- Talge NM, Neal C, Glover V. Antenatal maternal stress and long-term effects on child neurodevelopment: How and why? Journal of Child Psychology and Psychiatry. 2007;48:245–261. doi: 10.1111/j.1469-7610.2006.01714.x. doi: http://dx.doi.org/10.1111/j.1469-7610.2006.01714.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thapar A, Collishaw S, Pine DS, Thapar AK. Depression in adolescence. The Lancet. 2012;379:1056–1067. doi: 10.1016/S0140-6736(11)60871-4. doi: http://dx.doi.org/10.1016/S0140-6736(11)60871-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson R. Mothers’ violence victimization and child behavior problems: Examining the link. American Journal of Orthopsychiatry. 2007;77:306–315. doi: 10.1037/0002-9432.77.2.306. doi: http://dx.doi.org/10.1037/0002-9432.77.2.306. [DOI] [PubMed] [Google Scholar]
- Walker M. The inter-generational transmission of trauma: The effects of abuse on the survivor’s relationship with their children and on the children themselves. European Journal of Psychotherapy & Counseling. 1999;2:281–296. http://dx.doi.org/10.1080/13642539908400813. [Google Scholar]
- Weissman MM, Wickramaratne P, Nomura Y, Warner V, Pilowsky D, Verdeli H. Offspring of depressed parents: 20 years later. American Journal of Psychiatry. 2006;163:1001–1008. doi: 10.1176/ajp.2006.163.6.1001. doi: http://dx.doi.org/10.1176/appi.ajp.163.6.1001. [DOI] [PubMed] [Google Scholar]
- Williamson DE, Ryan ND, Birmaher B, Dahl RE, Kaufman J, Rao U, Puig-Antich J. A case-control family history study of depression in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:1596–1607. doi: 10.1097/00004583-199512000-00010. doi: http://dx.doi.org/10.1097/00004583-199512000-00010. [DOI] [PubMed] [Google Scholar]
- Wiseman H. On failed intersubjectivity: Recollections of loneliness experiences in offspring of Holocaust survivors. American Journal of Orthopsychiatry. 2008;78:350–358. doi: 10.1037/a0014197. doi: http://dx.doi.org/10.1037/a001419. [DOI] [PubMed] [Google Scholar]