Abstract
Sudden gains (SGs) are defined as abrupt and significant improvements in mental health symptoms that occur between two psychotherapy sessions. Preliminary evidence suggests that SGs may be an important pattern of symptom reduction in the treatment of alcohol use disorder (AUD) (i.e., a steep between-session reduction in drinking or alcohol craving frequency or intensity) (Drapkin et al., 2015). The current study examined SGs within two randomized clinical trials (RCTs) testing female-specific cognitive behavior therapy (CBT) protocol for AUD (n = 146). We tested a priori hypotheses about whether women’s baseline depression, anxiety, and confidence to be abstinent while in a negative emotional state would predict attainment of SGs after attending sessions that addressed depression, anxiety, and emotion regulation (i.e., sessions five and six of the 12-session protocol). Data were collected at baseline, within treatment, and 15 months after baseline. Results showed that women with high levels of depression and/or anxiety and low confidence to be abstinent in a negative emotional state at baseline were more likely to experience a SG (steep decrease in drinking) after sessions five and six (p=.02). Further, among women with high levels of depression and/or anxiety at baseline, those who experienced both a SG in drinking after session five/six and had higher confidence to remain abstinent in a negative emotional state at the end of treatment reported lower drinking frequency at 9- but not 15-month follow-up [95% CI = (−2.65, −0.86)]. Findings support the value of providing interventions targeting mood and emotion regulation in AUD treatment for women.
Keywords: Alcohol, Women, Depression, Anxiety, Sudden Gains
1. Introduction
Defined as steep and significant improvements in mental health symptoms that occur between two psychotherapy sessions, sudden gains (SGs) are hypothesized to be the result of what occurred in the first of the two sessions (Tang & DeRubeis, 1999). SGs in psychotherapy treatment were first described by Tang and DeRubeis (1999) among patients with depression receiving Cognitive Therapy (CT). Cognitive changes after a particular session were associated with a SG, which was then associated with positive short- and long-term therapeutic outcomes (Tang & DeRubeis, 1999; Tang et al., 2005). The authors operationalized SGs as improvements in symptoms that meet three criteria: (a) large in absolute magnitude, (b) large relative to pre-gain symptom severity, and (c) large relative to symptom fluctuation before and after the gain (Tang & DeRubeis, 1999). The SG phenomenon has been replicated by multiple research teams across different types of treatment including CT, cognitive behavioral therapy (CBT), supportive-expressive therapy, behavioral activation, and interpersonal psychotherapy; it has also spanned several psychological conditions, including depressive and anxiety disorders (post-traumatic stress disorder, social anxiety, panic, generalized anxiety disorders) (Aderka, Nickerson, Bøe, & Hofmann, 2012; Kelly, Rizvi, Monson & Resick, 2009; Stiles et al., 2003), and alcohol use disorders (AUD) (Drapkin, Epstein, McCrady, & Eddie, 2015).
Because SGs are operationalized as a dichotomous construct, they enable researchers to empirically examine discontinuous change in targeted symptoms during therapy. Behavior change researchers emphasize the importance of using non-linear methods to understand patients’ improvement in therapeutic settings, given that such improvement often does not occur in a linear fashion (Hayes, Laurenceau, Feldman, Strauss, & Cardaciotto, 2007; Hildebrandt, McCrady, Epstein, Cook, & Jensen, 2010; Resnicow & Page, 2008). SGs are a useful way to identify patterns of symptom change, patterns that may elucidate mechanisms of change in psychotherapy, helping us to understand which therapeutic interventions may act as active ingredients in treatment. Studying the association between interventions and SGs (e.g., decrease in depression or frequency of alcohol use) meets many of the criteria for establishing mechanisms of change because studying SGs can help establish strong association, temporal relation, specificity, and consistency (Nock, 2007) between the intervention and symptom improvement. Examining SGs in response to specific interventions may illuminate how a treatment works (i.e., mechanisms of change), and examining which sub-groups of patients experience SGs (i.e., moderators of change) may identify individuals for whom specific interventions works, thus allowing for tailoring of treatment interventions to meet specific client clinical presentations.
1.1 Sudden Gains in Treatment for Alcohol Use Disorders (AUD)
Mechanisms of change in CBT for AUD are an important research area (Magill, Kiluk, McCrady, Tonigan, & Longabaugh, 2015), and examining SGs may advance these efforts. For instance, in their study of SGs in CBT for women with AUD, Drapkin et al. (2015) found that one-third of the sample experienced SGs in at least one drinking domain (alcohol use frequency, frequency of urges for alcohol, and/or intensity of alcohol urges) during treatment. Additionally, SGs in the frequency of urges were associated with less drinking during follow-up. However, as the study did not test a priori hypotheses about the timing of SGs during treatment, the SGs were not examined in relation to specific interventions; as such, specific interventions that triggered SGs (or moderators of SG attainment) were not examined.
1.2 Identifying Moderators of SGs in Female-Specific CBT for AUD
Some researchers have argued that SG research carries the potential for elevated rates of Type I statistical errors due to the number of analyses necessary to calculate SGs for each session-to-session period (Vittengl, Clark, Thase, & Jarrett, 2015). Therefore, having an a priori hypothesis about when a SG is expected (i.e., which sessions might precipitate SGs) would not only provide further theoretical grounding for patients’ attainment of SGs and help identify potential mechanisms of change, but might also reduce the necessary number of statistical tests. The current study took this a priori approach by examining SGs after two sessions that specifically address depression, anxiety, and emotion regulation in a 12-session female-specific CBT protocol for AUD. These two sessions - five and six - teach skills for coping with and managing co-occurring symptoms of depression and/or anxiety.
In a community sample of alcohol-dependent women (in the National Epidemiological Survey on Alcohol and Related Conditions [NESARC]), 62% were diagnosed with a comorbid mood disorder, and 63% were diagnosed with a comorbid anxiety disorder. Women with AUD are 2.1 times as likely to be diagnosed with a mood disorder and 1.5 times as likely to be diagnosed with an anxiety disorder compared to women without any AUD (Goldstein, Dawson, Chou & Grant, 2012). Further, negative emotion has been found to be both a momentary trigger for alcohol use (Rubonis et al., 1994) and a trigger for relapse after a period of abstinence among women to an even greater extent than men (Karpyak et al., 2016; Walitzer & Dearing, 2006).
Given this research, sessions that directly target mood/negative emotion in a female-specific AUD protocol may be associated with subsequent SGs in drinking, particularly for women with high levels of co-occurring depression or anxiety. However, not all women drink to alleviate negative emotion. Among some women, higher self-efficacy to deal with negative emotions (perhaps because they have other ways of coping with negative emotion) may attenuate the negative emotion-drinking relationship, as these women may have other ways of dealing with negative emotion. Enhancing general self-efficacy for alcohol abstinence is a well-established mechanism of action in CBT for AUD (Magill et al., 2015); however enhancing self-efficacy not to drink when stressed or in a negative emotional state by providing alternative skills for coping with negative emotion is not necessarily standard in AUD treatment protocols. Interventions directly focused on regulating emotions may be particularly beneficial for women who have high levels of depression and/or anxiety, as their goal is to reduce depression and anxiety, decreasing or eliminating a common trigger to drink.
1.3 Current Study
Two randomized clinical trials (RCTs) (McCrady, Epstein, Hallgren, Cook, & Jensen, 2016; Epstein et al., under review) from which data were drawn for the current study provided a unique opportunity to examine moderators of change after particular treatment sessions. In the clinical trials, specific manual-guided interventions were administered consistently in each session, across participants, so that the effect of specific interventions (i.e., identifying and reducing depression/anxiety symptoms in sessions five and six) on drinking in the following days and weeks could be examined (Epstein & McCrady, 2009).
Two hypotheses were tested: (a) women who, at baseline, reported severe depression/anxiety symptoms and low levels of confidence to be abstinent when experiencing negative emotion would be more likely to experience a SG (i.e., steep decrease) in their drinking frequency after therapy sessions that addressed depression/anxiety and emotion regulation (i.e., sessions five and six of the 12 session outpatient female-specific CBT protocol for AUD); (b) among women with high levels of depression/anxiety at baseline, those who experienced a SG in drinking after sessions five or six and had high confidence to be abstinent in a negative emotional state at the end of therapy would have better drinking outcomes at 9 and 15 months follow-up.
2. Method
2.1 Design
Data were collected in two RCTs testing a 12-session Female-Specific CBT (FS-CBT) protocol for women with AUD. In one RCT (Study 1, total n=158 women), participants chose either an individual or couple CBT study arm, within which they were then randomized to one of two conditions (McCrady, Epstein, Hallgren, Cook, & Jensen, 2016). For the current secondary analyses, we drew data from women who were randomized to the individual FS-CBT condition (n=35; other conditions were not female-specific). The second RCT (Study 2) randomized women to either individual FS-CBT or group FS-CBT (Epstein et al., under review). Data from 111 women in Study 2 were used for the current analyses (see below for details), for a total sample of 146 women in the current analyses.
2.2 Participants
For both studies, women were at least 18 years of age, consumed alcohol in the past 30 days, and met criteria for DSM-IV current alcohol abuse or dependence. Exclusion criteria included psychotic symptoms in the past six months or evidence of gross cognitive impairment. In Study 1, one additional inclusion criterion was that women were in a committed heterosexual relationship (defined as married, separated with hopes of reconciliation, cohabitating for at least six months, or in a committed dating relationship of at least one year’s duration). Study 1 also excluded women who met criteria for physiological dependence on drugs other than marijuana or nicotine. In Study 2, one additional exclusion criterion was for women who were simultaneously involved in any other group therapy for their alcohol problem. See participant characteristics in Table 1, by study.
Table 1.
Participant Information by Study
| Study 1 n=35 (24.0%) |
Study 2 n=111 (76.0%) |
p-value from t- test or χ2 comparing two studies |
|
|---|---|---|---|
| Age M (SD) | 48.17 (9.86) | 50.01 (11.39) | .64 |
| Education – total years M (SD) | 15.29 (2.37) | 15.87 (3.07) | .31 |
| Race n (% of each study n) | .16 | ||
| White | 34 (97.1%) | 95 (85.6%) | |
| Black/African American | 1 (2.9%) | 10 (9.0%) | |
| Mixed Race/Not Hispanic or Latino | 0 (0%) | 6 (5.4%) | |
| Employment n (% of each study n) | .38 | ||
| Full-time or Part-time | 21 (60.0%) | 66 (59.4%) | |
| Student | 2 (5.7%) | 3 (2.7%) | |
| Retired | 3 (8.6%) | 8 (7.2%) | |
| Unemployed | 5 (14.3%) | 27 (24.3%) | |
| Disability | 0 (0%) | 2 (1.8%) | |
| Homemaker | 2 (5.7%) | 4 (3.6%) | |
| Other | 2 (5.7%) | 1 (0.9%) | |
|
| |||
| BL Percent Days Drinking M (SD) | 67.94 (28.72) | 68.99 (28.17) | .85 |
| BL Percent Days Heavy Drinking M (SD) | 46.95 (32.55) | 63.88 (29.59) | .01** |
| BL Mean Drinks Drinking Day M (SD) | 6.11 (3.30) | 6.93 (3.57) | .23 |
| BL BDI M (SD) | 16.20 (7.90) | 20.24 (11.18) | .02* |
| BL BAI M (SD) | 10.88 (7.52) | 13.74 (11.31) | .09 |
| Summed BL BDI-II/BAI M (SD) | 27.08 (13.61) | 33.98 (20.60) | .03* |
|
| |||
| Baseline DSM-IV Mood Disorder Diagnoses n (% of each study n) | |||
| Major Depression (Lifetime) | 14 (40.0%) | 39 (35.1%) | .32 |
| Dysthymia | 4 (11.4%) | 14 (12.6%) | .43 |
| Panic Disorder | 7 (20.0%) | 5 (4.5%) | .01* |
| Social Phobia | 0 (0%) | 10 (9.0%) | .16 |
| Obsessive-Compulsive Disorder | 0 (0%) | 1 (0.9%) | .71 |
| Generalized Anxiety Disorder | 5 (14.3%) | 18 (16.2%) | .57 |
| Post-Traumatic Stress Disorder | 2 (2.9%) | 7 (6.3%) | .51 |
| Any of above Mood Disorders | 14 (40.0%) | 64 (57.7%) | .48 |
Notes: BL = Baseline; BDI = Beck Depression Inventory; BAI = Beck Anxiety Inventory.
p<.05;
p<.01
2.3 Measures
2.3.1 Situational Confidence Questionnaire (SCQ-8; Breslin et al., 2000)
The SCQ is an 8-item self-report measure of confidence in one’s ability to not drink alcohol in eight separate situations. Each item is rated on a scale from 0% (not at all confident) to 100% (totally confident). For this study, the Negative Affect subscale (SCQ-NA) was used. This subscale measures confidence to resist urges to drink when in a negative emotional state and reflects the average confidence for three items: Confidence to avoid drinking: 1…when experiencing negative emotions (e.g., feeling depressed), 2.…when in physical discomfort (e.g., trouble sleeping, feeling tense), and 3.…when in conflict with others (e.g., had an argument with a friend). Internal consistency for the SCQ-NA subscale was high for the current sample, with a Cronbach alpha of 0.78 at baseline and 0.84 at post-treatment.
2.3.2 Beck Depression Inventory-II (BDI-II; Beck, Steer, & Garbin, 1988) and Beck Anxiety Inventory (BAI; Beck, Epstein, Brown, & Steer, 1988)
The BDI-II and BAI are both 21-item measures that assess the severity of depression and anxiety symptoms, respectively. For both measures, each item is rated on a scale from 0 (non-presence of symptom) to 3 (worst severity of symptom) and total scores range from 0–63. To examine how depression and anxiety symptom severity predicted SGs after our sessions of interest, we created a composite score of symptom severity by summing baseline BDI-II and BAI (total score ranging from 0–126). The rationale for creating a composite score was three-fold: 1. We wanted to look at total severity of these often co-occurring symptoms and how they collectively were associated with SG attainment (i.e., it did not matter for our study goals whether participants were high in depression, anxiety, or both); 2. There was high co-occurrence in this sample of anxiety and depression (correlation between baseline BDI and BAI scores was r=0.34, p=0.00), and amelioration in anxiety or depression can be reciprocal (Wilamowska, Tompson-Hollands, Fairholme, Ellard, Farchione, & Barlow, 2010); 3. Anxiety and depression were addressed across both sessions 5 and 6 in the FS-CBT protocol. Therapists potentially would have focused on the symptoms most relevant to the patient (i.e., if the patient had depression and not anxiety, both may be discussed but the focus would be on depression), and symptom improvement in depression, anxiety, or both may have occurred after either session of interest; 4. To increase the power of our moderation analyses (particularly given small sample size), and due to the theoretical reasons listed, we wanted to reduce the number of predictors in our model. If we had tested BAI and BDI scores separately and with their independent interactions with situational confidence, we would have unnecessarily increased the number of predictors and decreased power for our analyses. Cronbach alphas in the current sample were 0.90 for BDI-II, 0.93 for BAI, and 0.95 for combined BDI-II and BAI items. To test concurrent validity of the summed score, a logistic regression was done to examine whether summed BAI/BDI-II score predicted presence of a depression (major depression, dysthymia) or anxiety disorder (panic disorder, agoraphobia, social phobia, obsessive compulsive disorder, generalized anxiety disorder, and/or post-traumatic stress disorder) diagnosis at baseline. The regression results suggested that the summed BDI-II/BAI reliably predicted presence of a depressive disorder χ2(1)=26.32, p=.000 and anxiety disorder, χ2(1)=34.78, p=.000, lending support to the use of this summed score to reflect clinical symptom severity in this sample.
2.3.3 Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I; First et al., 2002)
The SCID-I is a semi-structured interview to assess current and lifetime Axis I disorders using DSM-IV (APA, 2000) criteria. Good inter-rater reliabilities have been reported for the SCID, with a mean reported kappa in a previous study (Epstein et al., 2002) of 0.87. The SCID was used to diagnose current DSM-IV Axis I conditions, including AUD, in our sample.
2.3.4 Psychiatric Research Interview for Substance and Mental Disorders (PRISM; Hasin et al., 2006)
The PRISM is a semi-structured diagnostic interview that assesses DSM-IV diagnoses. It was administered specifically to assess co-occurring PTSD, as reported in Table 1.
2.3.5 Timeline Follow-Back (TLFB; Sobell & Sobell, 1996)
The TLFB uses a calendar and other memory aids to determine an individual’s drinking over a specified time period. At baseline, participants were interviewed about their drinking on each of the 90 days prior to last drink before baseline; the TLFB was also administered at the 3 month, 9 months, and 15 month post-baseline research assessments. The TLFB has excellent reliability (Sobell & Sobell, 1978) and validity for alcohol use (Sobell, Maisto, Sobell & Copper, 1980). TLFB data were used to calculate pre-treatment and monthly post-treatment percent days drinking (PDD).
2.3.6 Daily Drinking Log (DDL)
Women kept daily records of drinking during the 12 session treatment period. Data from the follow-up TLFB were used to supplement within-treatment drinking data when DDL data were missing, to yield weekly, within-treatment PDD. 17.7% of all daily within-treatment data was missing from DDLs, and therefore supplemented by TLFB data.
2.4 Procedures
Participants completed an initial telephone screen for study eligibility and were scheduled for an in-person clinical intake. At the intake, study clinicians conducted semi-structured interviews, determined study eligibility, administered self-report questionnaires, and obtained informed consent from participants. Women were then scheduled for a baseline research assessment one week after the intake. At this baseline assessment, the participants met with a trained research assistant, completing additional self-report questionnaires and interviews to establish baseline measures of the outcome variables. They then were randomized to treatment condition (see parent RCT references for additional details, Epstein et al., under review; McCrady et al., 2016).
2.4.1 Treatment
Research has shown that women with AUD have a distinct clinical presentation and course of the disorder from men with AUD (Epstein & Menges, 2013), and gender differences exist in antecedents of relapse and mediators of treatment change (Epstein et al., under review). For instance, issues related to interpersonal functioning, emotion and mood regulation, and self-care have been shown to be particularly prevalent and relevant among women with AUD compared to men with AUD (Walitzer & Dearing, 2006; Timko, Finney, & Moos, 2005). The data used for the current study were from two clinical trials in which the second and fifth authors developed and tested a female-specific, cognitive behavioral treatment (FS-CBT) for AUD (Epstein et al., under review). In Study 1, FS-CBT was derived from and compared to an evidence-based, gender-neutral CBT (Epstein & McCrady, 2009); the data used in the current analyses were collected from women randomized to the female-specific CBT condition. The FS-CBT differed from the gender-neutral CBT as it included treatment components that explicitly addressed empirically-based issues salient for women with AUD, including social support, self-confidence, interpersonal functioning, and mood/emotion regulation (see Table 2). Study 2 then compared the individual modality FS-CBT to a group modality of the FS-CBT for AUD, and the current analyses used data from women in both conditions of this study. Women in all three of these conditions, across the two studies, received the same manual-guided interventions (see Table 2 for examples of session-by-session interventions).
Table 2.
Participants’ Sudden Gains (SGs) during Treatment
| Number of women experiencing SGs after individual sessions:
| |||
|---|---|---|---|
| Session preceding SG |
Main interventions in session (Female-specific interventions bolded) |
# of women with SG/ # women with eligible data (n) |
% experienced SG |
| 1 | Psychoeducation on female alcoholism | ||
| Self-monitoring and recording of alcohol use | |||
| Developing an abstinence plan | |||
| 2 | Functional analysis of drinking behavior | 24/63 | 38.1% |
| 3 | Stimulus control | 19/50 | 38.0% |
| Self-management planning | |||
| Problem solving for heavy drinkers in social network | |||
| 4 | Enhancing motivation | 12/45 | 26.7% |
| Decisional matrix | |||
| 5 | Coping with anxiety | 14/40 | 35.0% |
| Coping with depression | |||
| Dealing with urges | |||
| 6 | Management of emotions and moods | 9/41 | 22.0% |
| 7 | Improving social support for abstinence | 12/32 | 37.5% |
| Dealing with alcohol-related thoughts | |||
| 8 | Assertiveness training | 7/31 | 22.6% |
| Drink refusal | |||
| 9 | Anger management | 6/28 | 21.4% |
| Relapse prevention I | |||
| 10 | Problem solving skills | ||
| Relapse prevention II | |||
| 11 | Relapse prevention III: Lapse and relapse | ||
| 12 | Relapse prevention IV: Planning for maintenance | ||
Note: SG = Sudden Gain; as the calculation of SGs requires data from two between-session periods before and two after the between-session gap of interest, SGs could only be computed for sessions 2–9 of the 12 total sessions.
See Method for more detail.
Treatments were manual-guided, outpatient, female-specific, 12-session CBT protocols with a goal of abstinence from alcohol (Epstein et al., under review). As mentioned, the FS-CBT protocol integrates interventions that target topics that have been empirically shown to be common and associated with alcohol use among women with AUD. These three targeted topics include social support network for abstinence (Rice & Longabaugh, 1996; Davis & Jason, 2005), coping with co-morbid depression/anxiety and emotion regulation (Grant & Harford, 1995; Goldstein, Dawson, Chou & Grant, 2012), and psycho-education about the ways in which women uniquely use, process, and suffer from heavy drinking (Mann et al., 2005). These topics were covered via seven modules of content. These modules of content included female-specific interventions such as “problem-solving for presence of heavy drinkers in social network”, “coping with anxiety”, “coping with depression”, “assertiveness training”, and “psychoeducation on female alcoholism”. The manual also included core CBT, motivational enhancement (MET), and relapse prevention (RP) components, and employed a non-confrontational, collaborative therapist style (Epstein & McCrady, 2009). All language, examples, vignettes, worksheets, and illustrations were female relevant. Individual FS-CBT sessions were 60 minutes except session one, which was 90 minutes; group FS-CBT sessions lasted 90 minutes except session one, which lasted 120 minutes.
The sessions of interest for this study were sessions five and six, focused on topic 2, coping with depression/anxiety and emotion regulation. In session five, women worked with their therapists to identify their symptoms of depression, symptoms of and type of anxiety, and personal triggers for feelings of anxiety and/or depression. Women were taught to log their depression/anxiety thoughts between sessions five and six. In session six, women were taught to use cognitive restructuring, behavioral strategies, and relaxation (e.g., paced breathing) to reduce depression, anxiety, and emotion dysregulation. For session six homework, women continued logging negative thoughts leading to anxiety and depression and practiced cognitive restructuring, behavioral and relaxation skills for depression and anxiety.
2.4.2 Follow-up
Women were assessed 3, 9, and 15 months after baseline in both studies. The 3 month (immediate post-treatment) assessment was delayed to the end of treatment (up to 16 weeks after baseline) for women who were still in treatment beyond the scheduled 12. For Study 1, 3-, 9- and 15-month follow-up rates were 91%, 85%, and 80%, respectively. For Study 2, these follow-up rates for the individual condition were 94%, 94%, and 87% (respectively), and for the group condition were 92%, 88%, and 84% (respectively).
2.5 Data Analytic Plan
2.5.1 Calculating a Sudden Gain (decrease) in drinking frequency
We use the term “session(s) of interest” to refer to the sessions in which the emotion regulation/mood management interventions were delivered (sessions 5 and 6). Therefore, to examine SGs, we looked at how the percent of days that the women drank alcohol changed from the weeks before these sessions of interest to the weeks directly after these sessions of interest. To establish stability in the change (i.e., to show that a decrease in drinking was sustained), calculation of a SG requires data from two successive weeks before and after the session of interest. Additionally, the woman needs to have consumed alcohol on at least one day in the week prior to the session of interest (i.e., if the prior week had zero drinking days, there would be no potential for a decrease in her drinking). Because of these requirements, the number of women with eligible data for calculating a SG was 40 for session five and 41 for session six.
To calculate whether a woman experienced a SG after the sessions of interest, we established whether the criteria that defined a SG (Tang & DeRubeis, 1999) were met for sessions five or six (i.e., the change in PDD from the weeks prior to session 5 to the weeks after session 5, OR the change in PDD from the weeks prior to session 6 to the weeks after session 6). The first criterion for establishing a SG (as originally defined by Tang and DeRubeis, 1999) is that the therapeutic gain (in our case, decrease in PDD) is large in absolute magnitude. However, Tang & DeRubeis (1999, p. 895) identified their first criterion (i.e., at least seven points on the BDI) as arbitrary, and there is no specific criterion for PDD that would constitute “large in absolute magnitude.” Since we do not have a standard decrease in PDD that would definitively be considered “large,” we did not include an absolute criterion (following Drapkin et al., 2015). Therefore, we relied on the other two more specific criteria from Tang & DeRubeis to establish a SG: (a) Large relative to pre-gain symptom severity: We calculated the change score before and after sessions of interest (“pre-gain” session, e.g., week prior to session 5, to “post-gain” session, e.g., week after session 5). If there was a therapeutic gain (i.e., any decrease in PDD), we then established the percentage of change that was attained. Women who did not achieve at least 25% of a gain were excluded from the rest of the SG calculations and marked as not having attained a SG – a threshold adopted from prior work (Drapkin et al., 2015, following Tang & DeRubeis, 1999). (b) Large relative to symptom fluctuation before and after the gain: We used a modified version of the calculation (Tang et al., 2007, Drapkin et al., 2015) to establish this criterion. Note that this criterion establishes stability of the decrease in PDD. Specifically, we calculated the pooled standard error of the mean (SEM) PDD across four weeks – two weeks pre-gain (e.g., in establishing SG after session 5, this would be two weeks preceding session 5), and two weeks post-gain (e.g., two weeks’ PDD following session 5). We multiplied the pooled SEM of the four sessions by 2.78 [retained to maintain compatibility with the original criteria of Tang and DeRubeis (1999), when this criterion was used as a t-score calculation], and then used this value as a threshold for the difference between mean scores of pre- and post-gain sessions. We differed from the original Tang and DeRubeis (1999) equation in that we used the pooled SEM of the four weeks, rather than the pooled SD of the four weeks, given the larger scale and greater variability in PDD as an outcome variable (compared to BDI score). It is important to note that our SG calculations do not include women who could have progressed from a low level of drinking to abstinence during the week. Although women may improve slightly after the sessions of interest, or may maintain already established abstinence during this time, neither situation would constitute as SG if the percent change was less than 25%. Therefore, slight decreases in drinking to abstinence or maintenance of abstinence (while still positive occurrences) are not the focus of SG research, which instead focuses explicitly on patients who experience sudden and steep gains between sessions.
2.5.2 Data analytic plan
Descriptive statistics were first run to examine the presence of general SGs in our sample followed by SGs experienced after the sessions of interest (5 and/or 6). We then ran a hierarchical binary logistic regression to test whether baseline depression and anxiety symptoms, confidence to be abstinent in a negative affect situation (SCQ-NA) (in Step 1), and the interaction of depression/anxiety with SCQ-NA (in Step 2) would differentiate women who experienced a SG from those who did not after our sessions of interest. The variables in Step 2 address our first hypothesis. Lastly, we conducted a moderation model in SPSS 22 using PROCESS software (Hayes, 2012), using 20,000 bootstrap samples and a bias-corrected CI method. The moderation model tested hypothesis two among women with a summed BDI-II/BAI score above the median score. After controlling for baseline SCQ-NA, baseline PDD, and study, we entered mean-centered values for SCQ-NA at post-treatment follow-up as the predictor, presence of SG after session 5 and/or 6 as the moderator, and PDD at 9-month post-baseline as the outcome; a second moderation model with 15-month post-baseline PDD also was run.
3. Results
3.1 Sudden Gains
See Table 2 for information on SGs throughout treatment. Of all 146 women, 45.9% (n=67) did not attain a SG at any point during treatment; 41.8% (n=61) attained one SG; 9.6% (n=14) attained two SGs;1.4% (n=2) attained three SGs; and 1.4% (n=2) attained four SGs. 35.0% of women (14/40) experienced a SG after session 5 and 22.0% (9/41) experienced a SG after session 6, with 2 of those women experiencing a SG after both sessions 5 and 6. Among women who did not achieve a SG after session 5 or 6, their PDD increased by an average of 7.63% days drinking (SD=23.35) from session 5 to session 6 (representing a slight increase in PDD between sessions/slight worsening of symptoms) and decreased by an average of 0.70% days drinking (SD=19.81) from session 6 to 7. Among women who did achieve a SG after session 5 or 6, their average change in PDD was 18.0% decrease in days drinking (SD=13.62) from session 5 to 6 (representing a decrease in PDD between sessions/improvement of symptoms) and 7.59% (SD=14.84) average decrease from session 6 to 7.
3.2 Hypothesis 1: Predictors of Sudden Gains
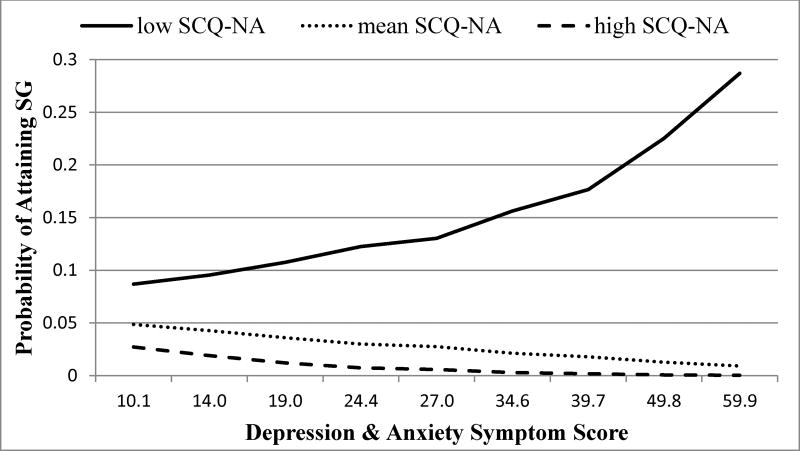
Women who, at baseline, report high levels of depression/anxiety and low levels of confidence to be abstinent in a negative emotional state will be more likely to experience a SG in their drinking (i.e., sudden decrease) after therapy sessions that address emotion/mood regulation (i.e., sessions 5 and 6). Results showed that, although the overall odds of attaining a SG were low, women with more severe anxiety/depression symptoms and low confidence to be abstinent when in a negative emotional state had the greatest odds of attaining a SG after sessions 5 and/or 6. A test of the full model against a constant-only model indicated that the depression + anxiety symptoms by confidence (SCQ-NA) interaction term in step 2 successfully predicted which women did and did not have SGs after session 5 and/or 6 (χ2=5.19, p=.02). Nagelkerke’s R2 was .13. Prediction success overall was 70.9% (94.6% for no sudden gain and 22.2% for sudden gain). The Wald criterion demonstrated that although depression/anxiety symptoms only trended toward significance as an independent predictor (p=.08), the interaction of anxiety and depression symptoms and SCQ-NA was a significant predictor of a SG after session 5 and/or 6 (p=.04) (see Table 3). To interpret the interaction effect, the probability of attaining a SG after sessions of interest was graphed for women with low, average, and high levels of situational confidence (mean, +/− 1 SD; see Figure 1). The highest probability of attaining a SG was among women with high depression/anxiety and low situational confidence, estimating that, among these women, one of every three women would experience a SG which represents significantly greater odds of a SG than women with higher situational confidence and/or lower depression and anxiety.
Table 3.
Hierarchical Logistic Regression for Variables Predicting SG after Session 5 and/or 6 (n=55)
| Block 1 | Block 2 | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Variable | B | SEB | eB |
p-value for B |
B | SEB | eB |
p-value for B |
| Negative emotion symptoms | −.007 | .016 | .993 | .66 | .065 | .037 | 1.07 | .08 |
| Baseline SCQ-NA | −.005 | .012 | .995 | .67 | .043 | .025 | 1.04 | .09 |
| Negative emotion symptoms by SCQ-NA interaction | -- | -- | -- | -- | −.002* | .001 | .998 | .04 |
| Constant | −.25 | −2.69 | ||||||
| χ2 | .28 | 5.19* | ||||||
| df | 2 | 1 | ||||||
Note: SCQ-NA = Situational Confidence Questionnaire, Negative Affect subscale; Negative emotion symptoms = summed BDI-II and BAI (see methods section for details); eB = exponentiated B. Sudden Gain (SG) coded as 1 for yes, achieved SG after session 5 and/or 6 and 0 as no, did not achieve SG.
p < .05
Figure 1.
Results from Logistic Regression, testing the interaction of negative emotion symptom score (summed BDI and BAI) with SCQ-NA (situational confidence-negative affect) subscale. Outcome reflects the odds ratio of attaining Sudden Gain after Session 5 and/or 6 (SG). X-axis shows scores for ten percentile groups (i.e., lowest 10% of women scored a 10.1 or lower; highest 10% scored 59.9 or higher). SCQ-NA reflects women at mean score, +/− one standard deviation.
To examine the specificity of our significant logistic regression finding, we explored whether having a SG after any session (other than 5 and/or 6) was also predicted by the interaction of baseline depression/anxiety and low situational confidence. The goal was to establish whether these women were simply more likely to have a SG overall, given the possibility that women with worse depression/anxiety and low situational confidence may have had greater opportunity to improve (and not necessarily due to the specific interventions in sessions 5 and 6). The overall logistic regression models and individual predictor parameters were not significant (p>.05) when run with other sessions as the dependent variable (i.e., sessions other than 5 or 6), suggesting that depression/anxiety and confidence not to drink when in a negative mood state were significant predictors of SG specifically after sessions 5 and/or 6.
3.3 Hypothesis 2: Sudden Gains and Situational Confidence as Predictors of Drinking Outcomes
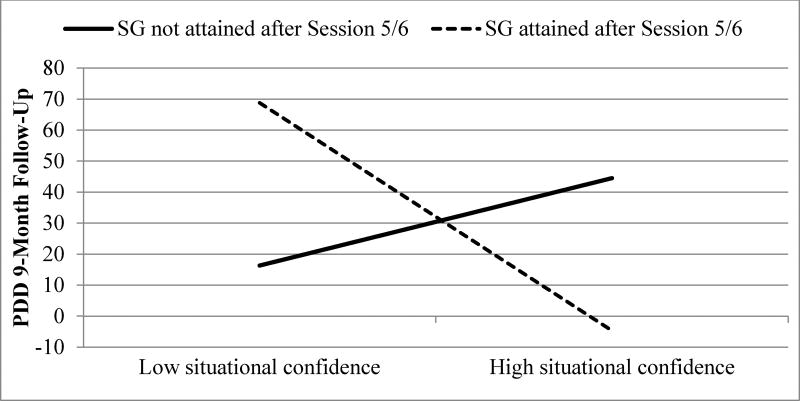
Among women with high levels of depression and/or anxiety at baseline, those who experience a SG after sessions 5 and/or 6 and have high confidence to be abstinent when in a negative emotional state at the end of therapy will have better drinking outcomes at 9 and 15 months follow-up. To examine whether SGs and confidence to be abstinent when in a negative emotional state translated into long-term gains, we tested a moderation model (Hayes, 2013). Results showed that, among women with high depression and/or anxiety at baseline, achievement of a SG after session 5 and/or 6 and high confidence (SCQ-NA) at end of treatment were together associated with significantly lower PDD at 9 month follow-up, compared to those with low SCQ-NA at end of treatment (Table 4, Figure 2). Although neither SGs after session 5 and/or 6 [95% CI = (−17.17, 20.46)] nor score on SCQ-NA at the end of treatment [95% CI = (−0.41, 0.26)] were independently significant predictors of post treatment drinking outcome, their interaction was a significant predictor [95% CI = (−2.65, −0.86)]. Women who experienced a SG after session 5 and/or 6 and had high confidence at the end of treatment had significantly lower PDD at 9-month follow-up, compared to women who did not achieve a SG after these sessions and to women who achieved a SG but had low confidence at the end of treatment. A post-hoc power analysis of this model showed sufficient power at 0.95.
Table 4.
Interaction of Sudden Gain (SG) after Session 5 and/or 6 and Situational Confidence at End of Treatment to Predict Drinking Frequency (PDD) 9- (n=25) and 15-months (n=23) post baseline among Women with High Levels of Depression and/or Anxiety
| Variable | B | SEB | R2 | ΔR2 | F | p |
|---|---|---|---|---|---|---|
| Dependent: Percent Days Drinking 9 month follow-up | ||||||
|
| ||||||
| 0.51* | 3.15 | 0.03 | ||||
| Covariate: Study | 2.41 | 9.70 | ||||
| Covariate: Baseline PDD | −0.13 | 0.16 | ||||
| Covariate: Baseline SCQ-NA | −0.69* | 0.24 | ||||
| Sudden Gain Session 5/6 (SG) | 1.65 | 8.95 | ||||
| SCQ-NA 3-mth follow-up (SCQ-NA3) | −0.08 | 0.16 | ||||
| SG* SCQ-NA3 interaction | −1.76** | 0.43 | 0.46** | 18.00 | 0.00 | |
|
| ||||||
| Dependent: Percent Days Drinking 15 month follow-up | ||||||
|
| ||||||
| 0.51 | 2.74 | 0.05 | ||||
| Covariate: Study | 1.41 | 9.10 | ||||
| Covariate: Baseline PDD | 0.03 | 0.16 | ||||
| Covariate: Baseline SCQ-NA | −0.70 | 0.23 | ||||
| Sudden Gain Session 5/6 (SG) | −8.05 | 12.26 | ||||
| SCQ-NA 3-mth follow-up (SCQ-NA) | 0.49 | 0.32 | ||||
| SG*SCQ-NA interaction | −0.20 | 0.99 | 0.001 | 0.04 | 0.84 | |
Note: Model tests the interaction of Sudden Gain and situational confidence at the end of treatment (i.e., 3 month follow-up) to predict Percent Days Drinking during follow-up among women with high depression and/or anxiety symptoms.
p < .05;
p<.001
Figure 2.
Predicted y-values for moderation model testing Hypothesis 2, with sudden gain (SG) status interacting with SCQ-NA (Situational Confidence Questionnaire, Negative Affect Scale) at post-treatment to predict PDD (Percent Days Drinking) at 9-month follow-up. Values for predictor variables were mean centered; graph represents the mean and plus/minus one standard deviation from the mean for SCQ-NA.
Results were not significant when run with PDD at 15-month follow-up as the outcome variable. Although the overall model was significant (p=.050), the interaction term was not significant [95% CI = (−2.29, 1.90)] (Table 4). The moderating (conditional) effect of situational confidence on PDD at 15 month follow-up was significant, but only for women who did not experience a SG (resulting in a non-significant interaction term). A post-hoc power analysis of this model showed insufficient power at 0.05.
Note that these moderation models were also run controlling for delivery modality of FS-CBT (group vs. individual) as a covariate. The results/significance testing for overall model, interaction terms, and each parameter did not change, with the exception that the overall model R2 for the 15-month follow-up model became significant (p=0.03, controlling for therapy modality, vs. p=0.05 when controlling for study only).
To examine the specificity of our significant 9-month follow-up finding, we tested whether having a SG after any session (other than 5 and/or 6) also interacted with situational confidence at the end of treatment to predict PDD during follow-up; was it merely the presence of any SGs that interacted with situational confidence to predict long-term drinking? Given that we expected to see long-term benefit of SGs among women for whom these sessions were targeted toward (i.e., women with high anxiety/ depression), we did not expect that the attainment of SGs after other sessions would be significantly associated with long-term drinking. The model testing SGs after sessions other than 5 and/or 6 were not significant at either 9- or 15-month follow-up (interaction term p>.05), suggesting that SGs specifically after our sessions of interest interacted with end of treatment situational confidence to predict lower PDD.
4. Discussion
In the current study we examined the presence and moderators of sudden gains (SGs) in female-specific CBT for AUD, as well as the association between SGs and long-term drinking outcomes. Our hypotheses were largely supported. Women with high levels of depression and/or anxiety at baseline and low confidence about being abstinent in a negative emotional state at baseline were more likely to experience a SG after sessions 5 or 6 - that is, after sessions that addressed depression and anxiety - compared to women with lower depression/anxiety. Among the women with high levels of depression/anxiety, those who both experienced the SG and then had high confidence to abstain in a negative emotional state at the end of treatment reported less frequent drinking at 9 month follow-up compared to women who did not achieve a SG, and to women who did have a SG but also had lower confidence at the end of treatment. These findings suggest a particular type of successful patient-treatment matching that was the goal of designing a female specific CBT protocol: some anxious and/or depressed women seeking treatment for AUD improved (i.e. reduced their drinking frequency) when provided skills targeted at their baseline clinical presentation and the function of their drinking, left therapy with high levels of confidence to be abstinent even when feeling distressed, and reported better overall drinking outcomes in the six months following treatment, compared with women who did not have this combination of symptoms, function of drinking, and improvements during therapy. However, it is apparent that not all women drink in order to cope with depression/anxiety – thus, while anxiety/depression alone do not necessarily predict utility or results from sessions targeting these symptoms, we predicted that it would be a combination of having these symptoms and also having poor self-efficacy for being abstinent. In this way, the analyses and results unearthed individual differences among these women, helping to indicate those who are most likely to benefit from the sessions of interest.
It is notable that these findings were not significant when examining the predictive ability of SGs and high confidence to abstain by the 15-month follow-up. It is possible that statistical insignificance may have been due to a loss of power with the smaller sample size (post-hoc power analyses showed insufficient power for the 15-month analyses), or a deterioration of gains during the longer follow-up period. This adds to the importance of study replication, particularly given the associations found between SGs and long-term improvement (up to 18 months) in the depression literature (Tang & DeRubeis, 1999).
Although this study was a secondary analysis of data from two clinical trials, we designed this study by articulating a priori hypotheses about the specific sessions that could possibly evoke quick changes in alcohol use among women. This was made possible by the fact that the manual-guided, well-specified treatments delivered specific interventions in each session consistently across participants. Additionally, the larger studies from which the data were derived were developing and testing female-specific interventions based on experimental and clinical research findings about gender differences in AUD. Depression and anxiety were specifically targeted in these treatments for women. Thus, this research extends the SG literature in multiple ways, by testing the effect of specific sessions and by examining this effect in a lesser-explored population of women with AUD. As discussed in the introduction, there is a need for psychotherapy research that examines mechanisms of change and that moves the field more towards a personalized approach to treatment for various disorders. This type of research holds promise, as it examines the efficacy of specific interventions for specific sub-groups of patients. This approach to psychotherapy research may be particularly important among individuals with substance use disorders, who have widely varying clinical presentations, clinical needs, and pathways to recovery.
4.1 Limitations
The results of this study must be interpreted within light of its limitations. Although we were able to compare women with and without SGs, our study was not experimental in design. The hypotheses were based on the idea that the provision of emotion-related skills would decrease intensity and frequency of depression and anxiety symptoms, thus eliminating a trigger that could precipitate drinking, as well as increasing confidence about maintaining abstinence in these situations. As the directionality of these constructs was not tested in this study - i.e., whether SGs lead to increased confidence, or whether increased confidence leads to SGs in drinking - we cannot infer that the interventions in the sessions of interest caused the women’s SGs, or that their SGs drove long-term benefits. We additionally cannot entirely rule out that women with high depression/anxiety and low situational confidence at baseline were “more severe” and therefore had greater opportunity to improve or experience a SG. This concern is, however, minimized by the secondary analyses for both hypotheses one and two, which tested the specificity of our findings to the sessions of interest (5 and 6). Additionally, it is notable that bivariate correlations showed negative, non-significant relationships between pre-treatment drinking and both BAI and BDI (p>0.05) scores. That is, women with higher depression/anxiety at baseline did not necessarily have greater frequency of alcohol use. Therefore, at baseline there was not a direct relationship between our predictor variables (BDI/BAI) and frequency of alcohol use, suggesting (as proposed in the introduction) that women with high anxiety or depression did not necessarily have heavier drinking patterns. An additional, important challenge of SG research is the low odds of attaining a SG, which provided us with a small sample size and should be considered when interpreting the results – replication is an important next step. This is particularly the case for the longer-term follow-up analyses (i.e., the moderation model with 15-month PDD as the outcome) given that post-hoc tests showed insufficient power. Finally, we cannot definitively pinpoint the mechanism of change underlying the SGs that we observed. This is an area for future research as well – not only to demonstrate SGs in treatment and their relation to long-term gains, but also to examine the exact mechanisms that lead to these SGs.
4.2 Conclusions
The current study provides important information for the growing population of women with AUD (Ruiz & Oscar-Berman, 2013; White et al., 2015). Women with AUD very often experience co-occurring mood disorders, and these individuals with comorbid conditions have been found in many studies to have poorer treatment retention and/or long-term outcomes after treatment (Epstein & Menges, 2013). For women with co-occurring conditions and low confidence to be abstinent when in a negative emotional state, directly addressing emotion regulation, anxiety, and depression may lead to sudden improvements in drinking behavior, which may then translate into longer-term maintenance of decreased drinking. Clinicians working with women with alcohol misuse may want to pay particular attention to completing a detailed assessment of depression and anxiety before starting treatment, something that can be overlooked in the field of substance abuse treatment, particularly in health care systems where substance use treatment and mental health care are siloed in different settings (Flynn & Brown, 2008). For women with high levels of depression and/or anxiety, integrating skills training around emotion regulation and mood management may be an integral element of treatment planning that contributes significantly to clinical outcomes. Additionally, addressing anxiety and depression among women with AUD may help the patient to understand the “whole picture” of her drinking and develop a cohesive understanding of her mental health.
Substantial research has identified the important role of negative emotion in drinking among women with AUD. Therefore, research that examines the extent to which enhancing mood and emotion regulation is an efficacious element of treatment for this population is an important step. Although past research has examined this with mixed gender samples with AUD (e.g., Monti et al., 1990; Berking et al., 2008; Stasiewicz et al., 2013), less research has focused on the efficacy of this approach for women or for women with co-occurring AUD and anxiety and/or depression. Additionally, future research examining the mechanisms that underlie behavior change in certain sub-populations of individuals with AUD will further our ability to provide personalized therapeutic interventions that are well-targeted and empirically validated. For example, further research on SGs in treatment for women with AUD could provide evidence for specific, efficacious interventions that elicit behavior change; understanding the mechanisms that account for the efficacy of an empirically-based intervention (e.g., situational confidence for maintaining abstinence) will benefit psychotherapy research for AUD.
Highlights.
Examined sudden therapeutic gains (SGs) among women in treatment for alcohol use
Analyses focused on SGs after sessions that addressed depression/anxiety
High depression/anxiety and low confidence were associated with greater odds of SG
For those with high depression/anxiety, SGs translated to lower long term use
Implications for women with AUD and AUD psychotherapy research discussed
Acknowledgments
This study was supported by Grants NIAAA R01 AA017163 and NIAAA R01 AA07070;
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Authors’ declarations of competing interests: None
References
- Aderka IM, Nickerson A, Bøe HJ, Hofmann SG. Sudden gains during psychological treatments of anxiety and depression: a meta-analysis. Journal of Consulting and Clinical Psychology. 2012;80(1):93–101. doi: 10.1037/a0026455. [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56(6):893–89. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8(1):77–100. [Google Scholar]
- Berking M, Wupperman P, Reichardt A, Pejic T, Dippel A, Znoj H. Emotion-regulation skills as a treatment target in psychotherapy. Behavior Research & Therapy. 2008;46:1230–1237. doi: 10.1016/j.brat.2008.08.005. [DOI] [PubMed] [Google Scholar]
- Breslin FC, Sobell LC, Sobell MB, Agrawald S. A comparison of a brief and long version of the Situational Confidence Questionnaire. Behaviour Research and Therapy. 2000;38(12):1211–1220. doi: 10.1016/s0005-7967(99)00152-7. [DOI] [PubMed] [Google Scholar]
- Davis MI, Jason LA. Sex differences in social support and self-efficacy within a recovery community. American Journal of Community Psychology. 2005;36(3–4):259–274. doi: 10.1007/s10464-005-8625-z. [DOI] [PubMed] [Google Scholar]
- Drapkin M, Epstein EE, McCrady BS, Eddie D. Sudden gains among women receiving treatment for alcohol use disorders. Addiction Research and Theory. 2015;23(4):1–7. doi: 10.3109/16066359.2014.981809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein EE, McCrady BS. Treatments That Work: Individual Cognitive Behavioral Therapy for Alcohol Use Problems. Therapist Manual. New York: Oxford University Press; 2009. [Google Scholar]
- Epstein EE, Menges D. Women and addiction. In: McCrady BS, Epstein EE, editors. Addictions: A comprehensive guidebook. 2. New York, NY: Oxford University Press; 2013. pp. 788–818. [Google Scholar]
- Epstein EE, McCrady BS, Hallgren KA, Cook SM, Jensen NK, Hildebrandt T. A randomized trial of female-specific cognitive behavior therapy for alcohol dependent women. doi: 10.1037/adb0000330. (under review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein EE, McCrady BS, Hallgren KA, Gaba A, Cook SM, Holzhauer CG, Hildebrandt T, Jensen NK. Individual versus group female-specific cognitive behavior therapy for alcohol use disorder. doi: 10.1016/j.jsat.2018.02.003. (under review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for the DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Flynn PM, Brown BS. Co-occurring disorders in substance abuse treatment: issues and prospects. Journal of Substance Abuse Treatment. 2008;34(1):36–47. doi: 10.1016/j.jsat.2006.11.013. http://doi.org/10.1016/j.jsat.2006.11.013Gol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein RB, Dawson DA, Chou, Grant BF. Sex differences in prevalence and comorbidity of alcohol and drug use disorders: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Studies on Alcohol and Drugs. 2012;73(6):938–950. doi: 10.15288/jsad.2012.73.938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Harford TC. Co-morbidity between DSM-IV alcohol use disorders and major depression: Results of a national survey. Drug and Alcohol Dependence. 1995;39:197–206. doi: 10.1016/0376-8716(95)01160-4. [DOI] [PubMed] [Google Scholar]
- Hasin D, Samet S, Nunes E, Meydan J, Matsoane K, Waxman R. Diagnosis of comorbid psychiatric disorders in substance users assessed with the Psychiatric Disorders Research Interview for Substance and Mental Disorders for DSM-IV. American Journal of Psychiatry. 2006;16(4):689–696. doi: 10.1176/ajp.2006.163.4.689. [DOI] [PubMed] [Google Scholar]
- Hayes AM, Laurenceau JP, Feldman G, Strauss JL, Cardaciotto L. Change is not always linear: the study of nonlinear and discontinuous patterns of change in psychotherapy. Clinical Psychology Review. 2007;27(6):715–723. doi: 10.1016/j.cpr.2007.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling (White paper) 2012 Retrieved from http://www.afhayes.com/public/process2012.pdf.
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A Regression-based approach. New York: The Guilford Press; 2013. [Google Scholar]
- Hildebrant T, McCrady B, Epstein EE, Cook S, Jensen N. When should clinicians switch treatments? An application of signal detection theory to two treatments for women with alcohol use disorders. Behavior Research and Therapy. 2010;48(6):524–530. doi: 10.1016/j.brat.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karpyak VM, Biernacka JM, Geske JR, Abulseoud OS, Brunner MD, Chauhan M, Mrazek DA. Gender-specific effects of comorbid depression and anxiety on the propensity to drink in negative emotional states. Addiction. 2016;111(8) doi: 10.1111/add.13386. E-pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly KA, Rizvi SL, Monson CM, Resick PA. The impact of sudden gains in cognitive behavioral therapy for Posttraumatic Stress Disorder. Journal of Traumatic Stress. 2009;22(4):287–293. doi: 10.1002/jts.20427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the national co-morbidity survey. Archives General Psychiatry. 1997;54:313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- Lemmens LHJM, DeRubeis RJ, Arntz A, Peeters FPML, Huibers MJH. Sudden gains in Cognitive Therapy and Interpersonal Psychotherapy for adult depression. Behaviour Research and Therapy. 2016;77:170–176. doi: 10.1016/j.brat.2015.12.014. [DOI] [PubMed] [Google Scholar]
- Magill M, Kiluk BD, McCrady BS, Tonigan JS, Longabaugh R. Active ingredients of treatment and client mechanisms of change in behavioral treatments for Alcohol Use Disorders: Progress 10 years later. Alcoholism: Clinical and Experimental Research. 2015;39(10):1852–1862. doi: 10.1111/acer.12848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann K, Ackermann K, Croissant G, Mundle H, Nakovics H, Diehl A. Neuroimaging of gender differences in alcohol dependence: Are women more vulnerable? Alcoholism: Clinical and Experimental Research. 2005;29:896–901. doi: 10.1097/01.alc.0000164376.69978.6b. [DOI] [PubMed] [Google Scholar]
- Marlatt GA. Relapse prevention: Theoretical rationale and overview of the model. Relapse Prevention. 1985:3–70. [Google Scholar]
- McCrady BS, Epstein EE, Hallgren KA, Cook S, Jensen NK. Women with alcohol dependence: A randomized trial of couple versus individual plus couple therapy. Psychology of Addictive Behaviors, E-pub ahead of print. 2016 doi: 10.1037/adb0000158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monti PM, Abrams DB, Binkoff JA, Zwick WR, Liepman MR, Nirenberg TD, Rohsenow DJ. Communication skills training, communication skills training with family and cognitive behavioral mood management training for alcoholics. Journal of Studies on Alcohol. 1990;51:263–270. doi: 10.15288/jsa.1990.51.263. [DOI] [PubMed] [Google Scholar]
- Nock MK. Conceptual and design essentials for evaluating mechanisms of change. Alcoholism: Clinical and Experimental Research. 2007;31(S3):4S–12S. doi: 10.1111/j.1530-0277.2007.00488.x. [DOI] [PubMed] [Google Scholar]
- Resnicow K, Page SE. Embracing chaos and complexity: A quantum change for public health. American Journal of Public Health. 2008;98(8):1382–1389. doi: 10.2105/AJPH.2007.129460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice C, Longabaugh R. Measuring general social support in alcoholic patients: Short forms for perceived social support. Psychology of Addictive Behaviors. 1996;10(2):104–114. [Google Scholar]
- Rubonis AV, Colby SM, Monti PM, Rohsenow DJ, Gulliver SB, Sirota AD. Alcohol cue reactivity and mood induction in male and female alcoholics. Journal of Studies on Alcohol. 1994;55:487–494. doi: 10.15288/jsa.1994.55.487. [DOI] [PubMed] [Google Scholar]
- Ruiz SM, Oscar-Berman M. Closing the gender gap: The case for gender-specific alcoholism research. Alcoholism & Drug Dependence. 2013;1(6):e106. doi: 10.4172/2329-6488.1000e106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Validity of self-reports in three populations of alcoholics. Journal of Consulting and Clinical Psychology. 1978;46:901–907. doi: 10.1037//0022-006x.46.5.901. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Maisto SA, Sobell MB, Cooper AM. Reliability of alcohol abusers’ self-reports of drinking behavior. Behavior Research and Therapy. 1980;17:157–160. doi: 10.1016/0005-7967(79)90025-1. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline followback user’s guide: a calendar method for assessing alcohol and drug use. Toronto, Ontario, Canada: Addiction Research Foundation; 1996. [Google Scholar]
- Stasiewicz PR, Bradizza CM, Schlauch RC, Coffey SF, Gulliver SB, Gudleski GD, Bole CW. Affect regulation training (ART) for alcohol use disorders: Development of a novel intervention for negative affect drinkers. Journal of Substance Abuse Treatment. 2013;45:433–443. doi: 10.1016/j.jsat.2013.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stiles WB, Leach C, Barkham M, Lucock M, Iveson S, Shapiro DA, Iveson M, Hardy GE. Early sudden gains in psychotherapy under routine clinic conditions: Practice-based evidence. Journal of Consulting and Clinical Psychology. 2003;71(1):14–21. [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. 5. Boston, MA: Allyn & Bacon; 2007. [Google Scholar]
- Tang TZ, DeRubeis RJ. Sudden gains and critical sessions in cognitive-behavioral therapy for depression. Journal of Consulting and Clinical Psychology. 1999;67:894–904. doi: 10.1037//0022-006x.67.6.894. [DOI] [PubMed] [Google Scholar]
- Tang TZ, DeRubeis RJ, Beberman R, Pham T. Cognitive changes, critical sessions, and sudden gains in cognitive-behavioral therapy for depression. Journal of Consulting and Clinical Psychology. 2005;73:168–172. doi: 10.1037/0022-006X.73.1.168. [DOI] [PubMed] [Google Scholar]
- Tang TZ, DeRubeis RJ, Hollon SD, Amsterdam J, Shelton R. Sudden gains in Cognitive Therapy of depression and depression relapse/recurrence. Journal of Consulting and Clinical Psychology. 2007;75(3):404–408. doi: 10.1037/0022-006X.75.3.404. [DOI] [PubMed] [Google Scholar]
- Timko C, Finney JW, Moos RH. The 8-year course of alcohol abuse: Gender differences in social context and coping. Alcoholism: Clinical and Experimental Research. 2005;29:612–621. doi: 10.1097/01.alc.0000158832.07705.22. [DOI] [PubMed] [Google Scholar]
- Vittengl JR, Clark LA, Thase ME, Jarrett RB. Detecting sudden gains during treatment of Major Depressive Disorder: Cautions from a Monte Carlo analysis. Current Psychiatry Review. 2015;11(1):19–31. doi: 10.2174/1573400510666140929195441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walitzer KS, Dearing RL. Gender differences in alcohol and substance use relapse. Clinical Psychology Review. 2005;26:128–148. doi: 10.1016/j.cpr.2005.11.003. [DOI] [PubMed] [Google Scholar]
- White A, Castle IJ, Chen CM, Shirley M, Roach D, Hingson R. Converging patterns of alcohol use and related outcomes among females and males in the United States, 2002 to 2012. Alcoholism: Clinical and Experimental Research. 2015;39(9):1712–26. doi: 10.1111/acer.12815. [DOI] [PubMed] [Google Scholar]
- Wilamowska ZA, Thompson-Hollands J, Fairholme CP, Ellard KK, Farchione TJ, Barlow DH. Conceptual background, development, and preliminary data from the unified protocol for transdiagnostic treatment of emotional disorders. Depression and Anxiety. 2010;27(10):882–890. doi: 10.1002/da.20735. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Villarroel N. Dynamic association between negative affect and alcohol lapses following alcohol treatment. Journal of Consulting and Clinical Psychology. 2009;77:633–644. doi: 10.1037/a0015647. [DOI] [PMC free article] [PubMed] [Google Scholar]