Abstract
The rendezvous approach is a salvage technique after failure of endoscopic retrograde cholangiography (ERC). In certain circumstances, percutaneous-endoscopic rendezvous (PE-RV) is preferred, and endoscopic ultrasound-guided rendezvous (EUS-RV) is difficult to perform. We aimed to evaluate PE-RV outcomes, describe the PE-RV techniques, and identify potential indications for PE-RV over EUS-RV.
Retrospective analysis was conducted of a prospectively designed ERC database between January 2005 and December 2016 at a tertiary referral center including cases where PE-RV was used as a salvage procedure after ERC failure.
During the study period, PE-RV was performed in 42 cases after failed therapeutic ERC; 15 had a surgically altered enteric anatomy. The technical success rate of PE-RV was 92.9% (39/42), with a therapeutic success rate of 88.1% (37/42). Potential indications for PE-RV over EUS-RV were identified in 23 cases, and either PE-RV or EUS-RV could have effectively been used in 19 cases. Endoscopic bile duct access was successfully achieved with PE-RV in 39 cases with accessible biliary orifice using one of PE-RV cannulation techniques (classic, n = 11; parallel, n = 19; and adjunctive maneuvers, n = 9).
PE-RV uses a unique technology and has clinical indications that distinguish it from EUS-RV. Therefore, PE-RV can still be considered a useful salvage technique for the treatment of biliary obstruction after ERC failure.
Keywords: endoscopic retrograde cholangiopancreatography, endoscopic ultrasound guided rendezvous, percutaneous endoscopic rendezvous
1. Introduction
Endoscopic approach to the biliary orifice, selective biliary cannulation, and guidewire (GW) passage through a biliary stricture are essential prerequisites for therapeutic endoscopic retrograde cholangiography (ERC) in patients with biliary diseases.[1–3] However, many anatomical factors, such as surgically altered anatomy, duodenal diverticulum, or a tight biliary stricture, can affect the above-mentioned technical steps leading to therapeutic failure of ERC.[3] Endoscopic ultrasound-guided rendezvous (EUS-RV) has recently been performed as a salvage technique after ERC failure, with its technical feasibility and safety demonstrated in several studies.[4–9] In contrast, percutaneous-endoscopic rendezvous (PE-RV) has been relatively less investigated, in part because of the rapid expansion of EUS-guided technology as well as some concerns regarding percutaneous transhepatic biliary drainage (PTBD)-related morbidity and patient discomfort.[10,11] However, based on our experience, there are certain circumstances in which PE-RV is preferred, and EUS-RV is difficult to perform. Therefore, this study aimed to evaluate the outcomes of PE-RV, provide a description of PE-RV, and identify potential indications for PE-RV over EUS-RV.
2. Methods
2.1. Patients
From January 2005 to December 2016, 8147 ERCs were attempted at our tertiary referral center, Ajou University Hospital, Suwon, South Korea. We retrospectively reviewed a prospectively designed ERC database to identify patients in whom PE-RV was used as a salvage procedure after failure of ERC for the treatment of biliary diseases. This study was approved by our institutional review board (AJIRB-MED-MDB-14–149), and informed consent was obtained from each patient for PE-RV.
2.2. Percutaneous-endoscopic rendezvous procedure
After failed ERC, a PTBD was performed on the same day in the targeted intrahepatic bile duct by an experienced interventional radiologist (J.H.W.) who performs more than 100 PTBDs per year and has performed more than 2000 cases in total. For patients with an existing PTBD tube, for a septic condition or because of the local hospital's preference, the preformed percutaneous tract was used for PE-RV.
PE-RV was done 3 to 7 days after ERC according to the patient's condition. All PE-RV procedural steps were performed by an experienced endoscopist (J.H.K.), trained in endoscopic and interventional radiology, who performs more than 400 ERCP procedures yearly and has performed over 8000 ERCP procedures in total.
A 450 cm long 0.035-inch GW (Jagwire; Boston Scientific Corp., Natick, MA) or 0.035-inch J-shaped hydrophilic GW (Terumo Guidewire; Terumo Corp., Tokyo, Japan) was inserted into the duodenum or jejunum under fluoroscopic guidance with the patient conscious and supine. If proper GW manipulation was difficult, the PTBD tube was exchanged for a hydrophilic-coated guiding catheter (GLIDECATH; Terumo Corp., Tokyo, Japan) that was used to support the GW shaft and reverse the GW tip toward the ampulla or anastomotic site (Fig. 1). When the endoscopic approach to the biliary orifice failed because of surgically altered anatomy, the GW was advanced further distally, as far as possible from the papilla or anastomotic site (Fig. 1), to act as a guide for the subsequent retrograde endoscopic approach. Patients were then placed in a prone position and sedated with standard doses of midazolam, propofol, and meperidine. A side-viewing duodenoscope (JF-260V; Olympus Corp., Tokyo, Japan) or cap-fitted forward viewing endoscope (GIF-2TQ260M or CF-Q260AI; Olympus, Tokyo, Japan) was advanced orally. For patients with surgically altered enteric anatomy, if the endoscope did not reach the biliary orifice alongside the antegrade GW (AGW), a snare or basket was inserted through the working channel of the endoscope to capture the AGW. The endoscope was then pushed from the oral side by the operator, while the guidewire and snare connected to it were gently pulled toward the biliary orifice by the assistant nurse (Push-pull technique-1, Fig. 1). Endoscopic biliary cannulation was attempted using one of the PE-RV cannulation techniques (Figs. 2–6).
Figure 1.
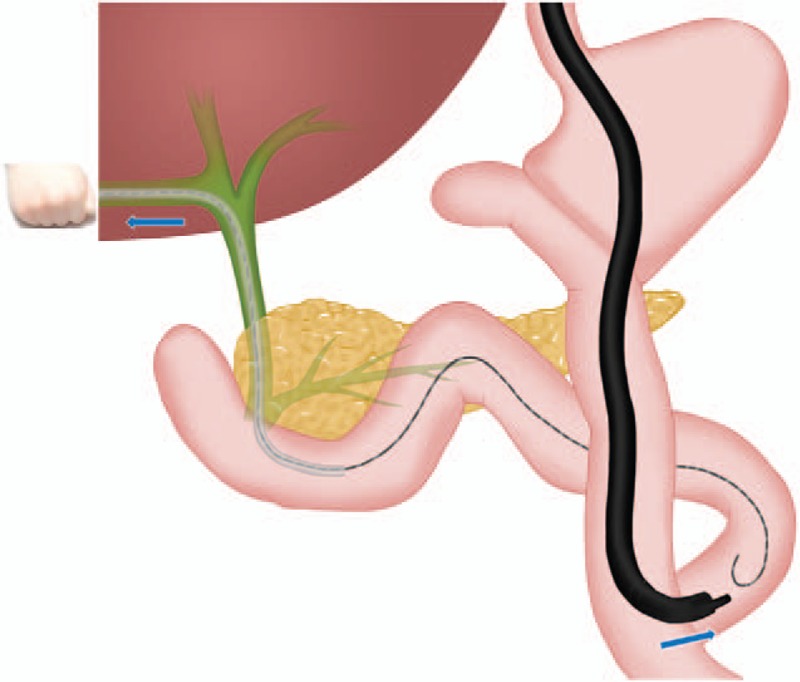
Push-pull technique-1 in a patient with a Roux-en-Y anastomosis. The distal tip of the antegrade guidewire (AGW) is grasped with a snare and passed through the working channel of the endoscope in the Y limb, near the Treitz ligament. The endoscope is then pushed from the oral side, while the guidewire and snare connected to it are gently pulled toward the biliary orifice. A percutaneous hydrophilic-coated guiding catheter (GLIDECATH) over the AGW can be useful to facilitate advancement of the guidewire further distally. AGW = antegrade guidewire.
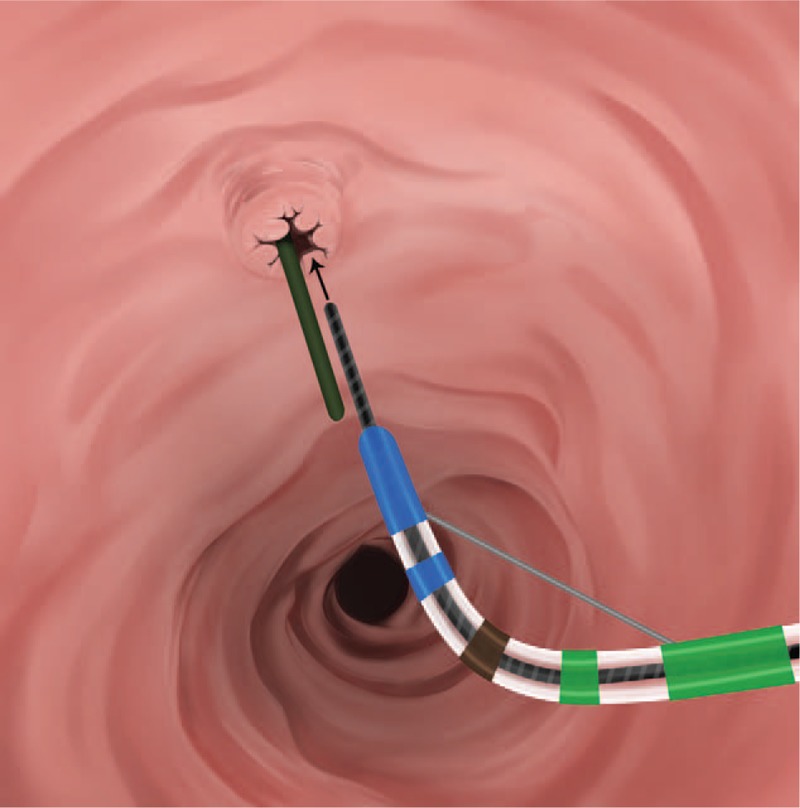
Figure 2.
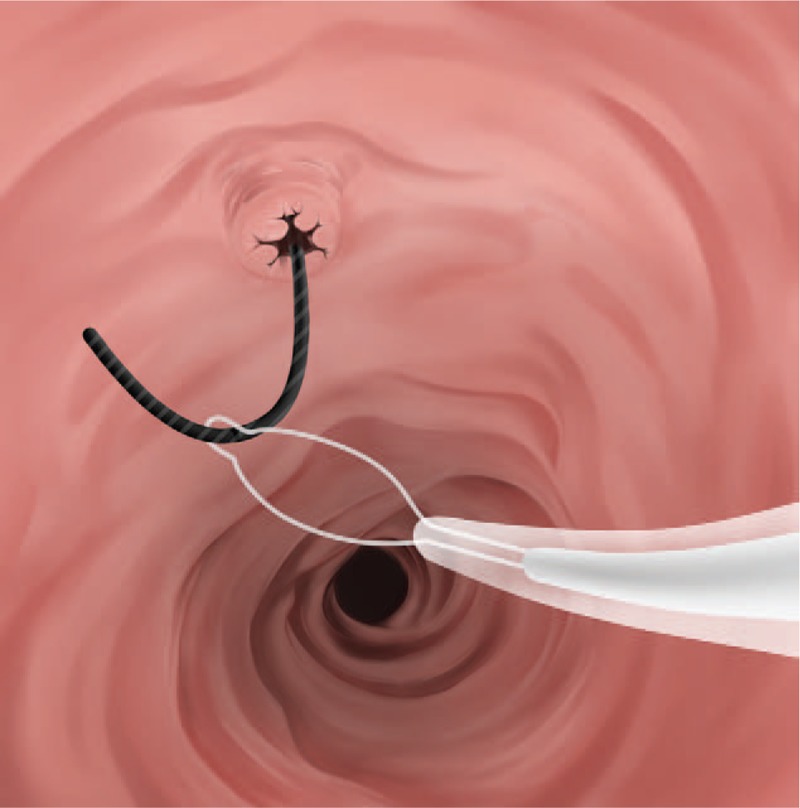
Classic technique. The distal tip of the antegrade guidewire (AGW) is grasped with a snare and passed through the working channel of the duodenoscope. Then, the snare and AGW are withdrawn through the working channel of the duodenoscope. Retrograde cannulation is attempted over the AGW. AGW = antegrade guidewire.
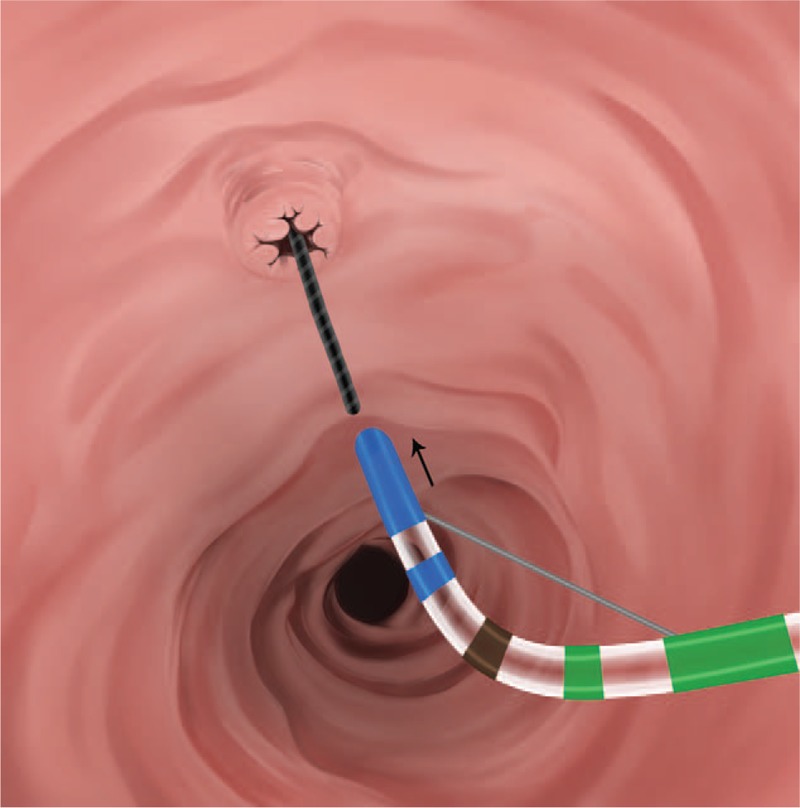
Figure 6.
Retrograde guidewire insertion after antegrade balloon dilation of the biliary orifice. Percutaneous balloon dilation of the biliary orifice is performed over the antegrade guidewire, and conventional retrograde cannulation is attempted through the dilated orifice.
For a tight hilar biliary stricture that could only accommodate a GW and not the dilating devices or stent assembly, simultaneous pulling via the AGW and pushing of the endoscope toward the percutaneous side was used to advance the dilating device through the stricture (Push-pull technique-2, Fig. 7). After all PE-RV procedures, a new PTBD tube was finally inserted over the AGW by the endoscopist to prevent bile leakage from an immature fistula tract, which was removed 1 week after the PE-RV procedure.
Figure 7.
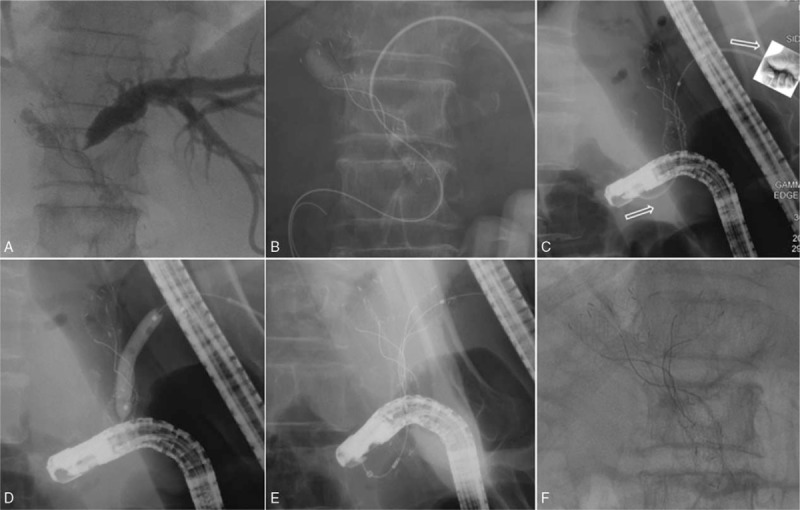
Push-pull technique-2 in a patient with inoperable Bismuth type IIIa malignant hilar cholangiocarcinoma. (A) Left percutaneous transhepatic biliary drainage tube and a stent-in-stent in the right anterior and posterior intrahepatic ducts. (B) Percutaneous dilator could not be passed through the tight hilar stricture; only the antegrade guidewire (AGW) could be passed. (C) Retrograde advancement of a balloon dilating catheter through the stricture was performed by simultaneously pulling the AGW and pushing the endoscope toward the percutaneous side. (D) Successful balloon dilation of the stricture. (E and F) Completed triple hilar stenting.
2.3. Measurements
ERC failure was defined if at least one of following 3 steps failed: endoscopic approach, selective biliary cannulation, or GW passage through the biliary stricture. In cases of surgically altered anatomy, failure of the endoscopic approach was defined as failure of both a duodenoscope and colonoscope. Balloon-assisted ERCP was not performed in this study. Cannulation failure in Billroth-II patients was defined as biliary access failure despite wire-guided cannulation using a rotatable sphincterotome or biliary cannula as well as needle-knife precut papillotomy.
Baseline clinical outcomes of PE-RV, including technical success, therapeutic success, adverse events, and cannulation technique were evaluated. Technical success of PE-RV was defined as achieving: AGW placement in the small bowel; retrograde endoscopic approach; and retrograde deep cannulation to the targeted bile duct. To identify potential indications for PE-RV over EUS-RV, we theoretically evaluated whether PE-RV could have been replaced by EUS-RV in patients in whom PE-RV had been already performed.
2.4. Statistical analyses
Mean and standard deviation (SD) were used to describe continuous variables, while percentages were used for categorical variables. Statistical analyses were performed in an intention-to-treat manner, using SPSS version 18.0 (SPSS Inc., Chicago, IL).
3. Results
During the study period, PE-RV was performed after therapeutic ERC failure in 42 cases, 15 of whom had surgically altered enteric anatomy. Relevant baseline demographics and indications for initial ERC are summarized in Table 1. Causes of ERC failure included (Table 2): failed endoscopic approach to the biliary orifice (n=7), failed selective biliary cannulation (n = 25), and failed selective GW insertion into intrahepatic duct (n = 10). A technical success rate of 92.9% (39/42) and a therapeutic success rate of 88.1% (37/42) were achieved with the PE-RV procedure (Table 3). The technical success rate was 71.4% (5/7) for cases of ERC failure due to a failed endoscopic approach to the biliary orifice, 96.0% for cases of failed biliary cannulation, and 100% for cases of selective GW penetration into the intrahepatic bile duct.
Table 1.
Baseline characteristics.

Table 2.
Anatomic reasons for failed therapeutic endoscopic retrograde cholangiography.
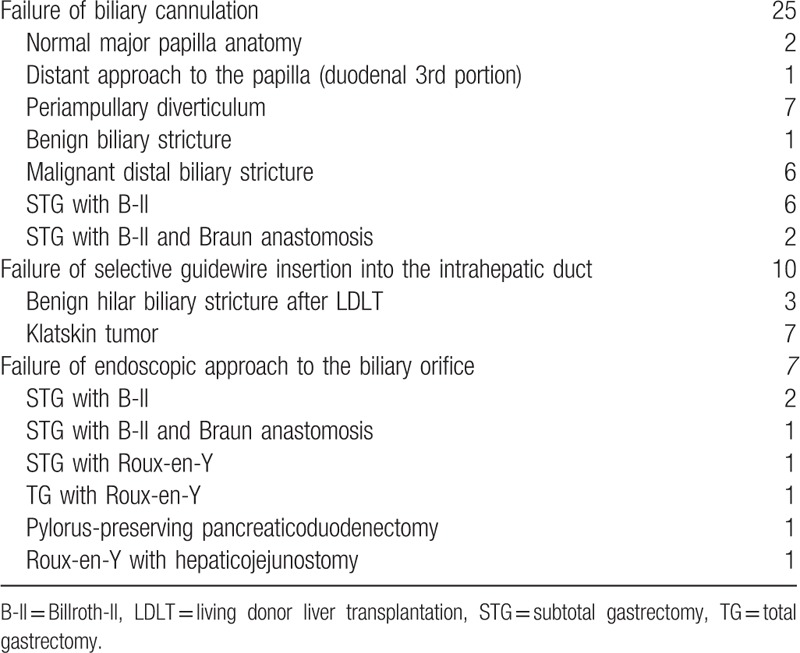
Table 3.
Outcomes of percutaneous-endoscopic rendezvous.
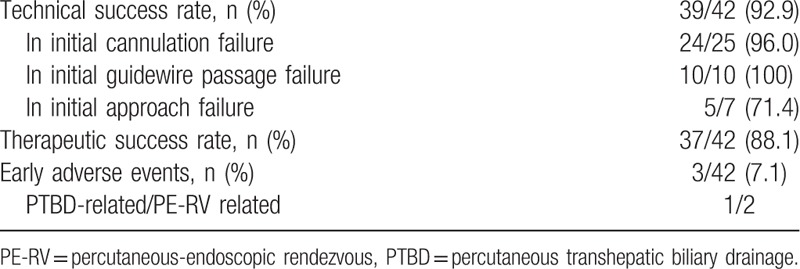
PE-RV technical failure occurred in 2 patients who had a Roux-en-Y anastomosis, with approach failure attributed to the longer bowel and loop formation, and one patient due to incidental AGW loss out of the percutaneous tract during patient's position change to prone.
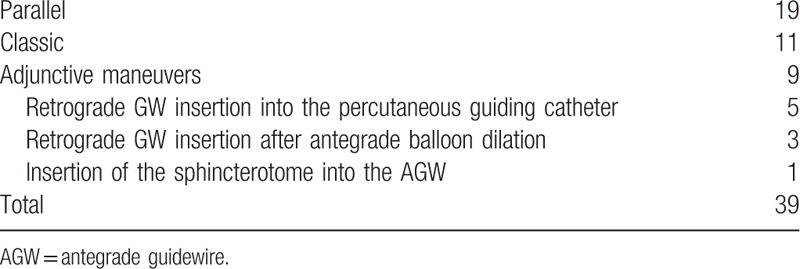
Biliary cannulation was successfully performed in all 39 cases with an accessible biliary orifice using one of the 5 techniques described in Table 4. The parallel technique was the most frequently used, followed by the classic technique.
Table 4.
Classification of percutaneous-endoscopic rendezvous cannulation techniques in 39 cases of accessible biliary orifice.
Bile duct stone removal failed in 1 patient with Billroth-II anatomy, despite technical success of PE-RV. This patient was successfully treated with percutaneous transhepatic cholangioscopy. In another patient with a malignant hilar biliary stricture, hilar stenting failed because of a tight biliary stricture through which only a GW, not the stent assembly, could be passed using PE-RV.
PTBD-related bleeding occurred in 1 patient, and pancreatitis developed in 1 patient. Two patients were treated conservatively. In 1 patient, AGW loss occurred during final PTBD tube reinsertion over the AGW after completion of therapeutic PE-RV. This patient was referred to the interventional radiologist and underwent a new ultrasound-guided puncture for PTBD near the intrahepatic duct branch where the original AGW was placed. No surgical intervention was required in any patients.
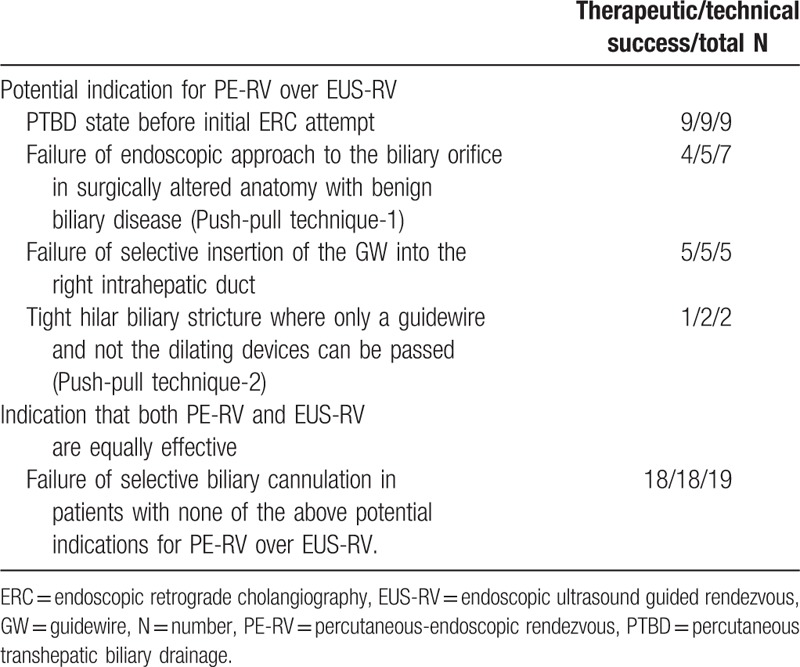
Potential indications for PE over EUS-RV were identified for 23 cases as follows (Table 5): (1) a preformed PTBD tube before initial ERC attempt; (2) failure of retrograde endoscopic approach to the biliary orifice due to surgically altered enteric anatomy complicated by bile duct stone or benign stricture; (3) tight hilar biliary stricture, in which a only GW passes, not dilating devices; and (4) failure of selective GW insertion into the right intrahepatic duct. PE-RV and EUS-RV were deemed to be equally effective for 19 cases of failed biliary cannulation in patients with no potential indications for PE-RV over EUS-RV.
Table 5.
Classification of clinical indications for percutaneous-endoscopic rendezvous considering substitutability with endoscopic ultrasound-guided rendezvous.
4. Discussion
PE-RV provides a salvage option for failed therapeutic ERC in patients with biliary obstructions, with installation of a PTBD tube rapidly alleviating acute biliary inflammation. The PTBD tube may facilitate subsequent therapeutic biliary intervention using simultaneous antegrade and retrograde access to the bile duct.[10,12–29] Based on our experience, although EUS-guided techniques are increasingly being developed and used, there are unique clinical indications for which PE-RV should be used.
In patients with a surgically altered enteric anatomy, EUS-RV cannot be used as a salvage technique after a failed retrograde approach to the biliary orifice as an accessible papilla or anastomosis is required. In contrast, PE-RV can assist the retrograde endoscopic access to the biliary orifice using a Push-pull technique-1 (Fig. 1). In our study, we successfully used this technique to overcome approach failure in 5 patients with a surgically altered enteric anatomy. Itoi et al[30] described a case of successful single balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography using a similar method in a patient with a Roux-en-Y limb complicated by a bile duct stone. Tsutsumi et al[31] recently described the use of a similar technique in a patient in whom initial approach to the anastomotic site failed because of a Roux-en-Y hepaticojejunostomy. With recent advances in balloon enteroscopy-assisted ERCP in patients with altered surgical anatomy,[32] the Push-pull technique-1 may no longer be valid in large biliary centers. In our center, balloon-assisted ERCP is now being implemented. However, only a long-type double-balloon enteroscope is available in Korea, and thus, most commercially available ERCP accessories are limited. Therefore, this technique would be still valid in centers not equipped for balloon enteroscopy or where only long-type double balloon enteroscopes are available.
To match the AGW to a retrograde endoscope near the Treitz ligament during the Push-pull technique-1, the AGW should be advanced from the intrahepatic bile duct into the small bowel as distally as possible, requiring stable and delicate control of the AGW. PE-RV facilitates manipulation of the AGW and advancement of the GW, compared to EUS-RV, by: (1) reducing the distance between the operator's right hand and the tip of the AGW as the esophagus and stomach are bypassed, and (2) allowing flexible percutaneous guiding devices (angiocatheter or biliary cannula), which enhances support of the GW shaft and facilitates advancement of the AGW distally. However EUS-RV has improved with an access needle developed by Wilson Cook, which decreases the risk of GW shearing and allows for repeated GW manipulation.[33]
In patients with a tight hilar biliary stricture, through which only a GW but not the stent assembly or dilating devices can be passed, and biliary stenting failure after application of either antegrade or retrograde force, EUS-RV cannot be used as a salvage technique, as it only permits retrograde manipulation for advancement of the dilating device or stent assembly. In these cases, the Push-pull technique-2 in PE-RV can overcome the tight hilar biliary stricture, using simultaneous pulling via the GW toward the percutaneous tract by an assistant nurse and pushing of the endoscope by the operator (Fig. 7).
The use of EUS-RV is also limited after failed GW insertion into the right intrahepatic duct, as the EUS-RV technique typically uses the left intrahepatic duct via the transgastric route, and therefore, advancement of the AGW from the right intrahepatic duct into the duodenum would be difficult. Of note, recent case reports have described successful EUS-RV using a right inferior intrahepatic route, close to the duodenum or antrum.[34–36] Further data should be accumulated for the use of EUS-RV via the right intrahepatic route.
For patients with a PTBD tube, it is clinically simple and technically easy to use the preformed PTBD tract as an antegrade route for RV, and therefore, EUS-guided transenteric puncture is not required. In this study, PE-RV was successfully performed via a preformed PTBD tract in 6 patients who failed selective biliary cannulation and in 3 patients who failed selective GW insertion into the targeted intrahepatic duct.
Except for the potential indications for PE-RV over EUS-RV described above, either PE or EUS-RV can be used in patients for whom failed selective biliary cannulation was the only obstacle in the initial ERC. However, PE-RV provides more varied cannulation techniques than EUS-RV, for which only 2 cannulation techniques are available, the classic (Fig. 2) and the parallel techniques (Fig. 3).[4,9]
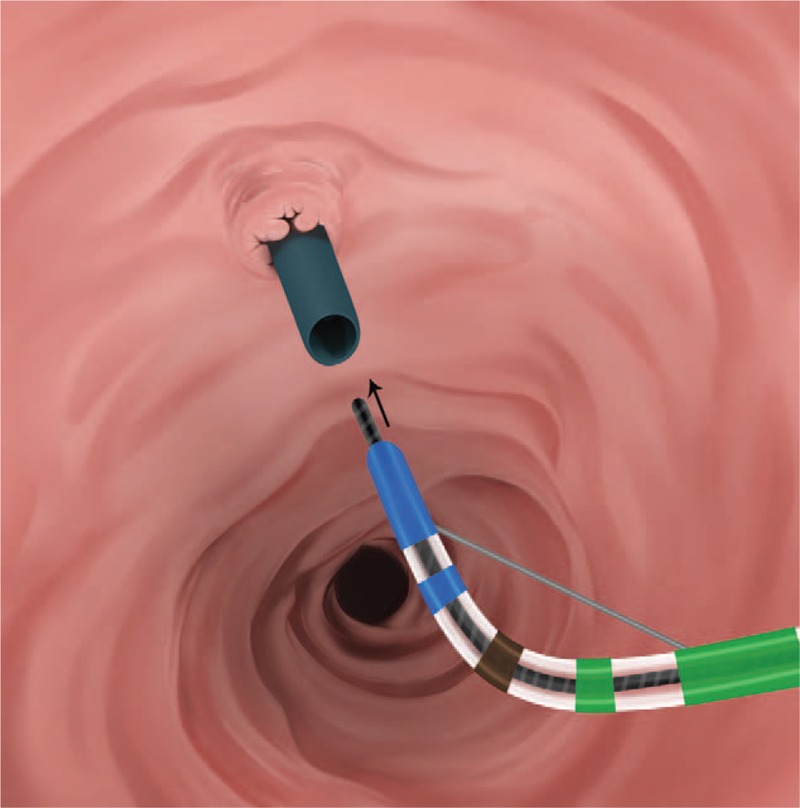
Figure 3.
Retrograde guidewire cannulation alongside the antegrade guidewire (AGW) (the parallel technique). Biliary cannulation is attempted in retrograde fashion alongside the AGW. AGW = antegrade guidewire.
The classic technique has been the most frequently used cannulation technique for PE-RV.[10,13–19,24] However, this technique can be limited by difficulty in capturing the hydrophilic GW, the possibility of kinking, torqueing, or incidental loss of the GW during withdrawal, laborious GW manipulation, and the risk of bile duct injury caused by the sharp end of the AGW during the therapeutic procedure.[20,22] Bile duct cannulation using the parallel technique is simple and effective, while avoiding the limitations of the classic technique.[12,18,22,23,25] In our center, we have usually considered this technique for initial cannulation attempts.
The cannulation technique in which the retrograde GW is in the percutaneous guiding catheter (Fig. 4) is exclusively applicable for PE-RV with antegrade guiding devices, such as an angiocatheter, ensuring sufficient space for retrograde passage of the GW through the ampullary orifice or stricture segment. We have used this technique for cases where the parallel technique was unsuccessful. Verstandig et al[18] reported 15 procedures using this rendezvous technique in 1993, with Lee et al[27] describing the technique as a modified rendezvous technique after failure of retrograde selective GW insertion into the right intrahepatic duct owing to bile duct invasion by gallbladder cancer.
Figure 4.
Retrograde insertion of the guidewire (GW) into the percutaneous guiding catheter. The retrograde GW is inserted into the lumen of the percutaneously placed hydrophilic-coated guiding angiocatheter. The sphincterotome is advanced over the retrograde GW, withdrawing the guiding catheter proximally. GW = guidewire.
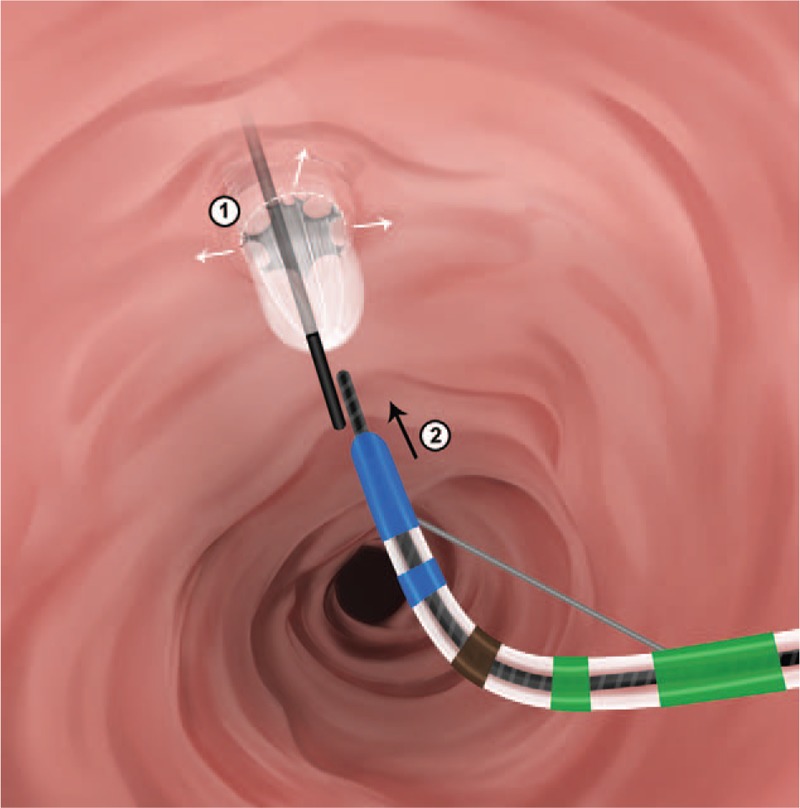
The cannulation technique in which the sphincterotome is placed into the AGW exiting the biliary orifice (Fig. 5) is also exclusively applicable for PE-RV and can be used as an alternative to the above technique. This technique can be technically challenging in terms of end-to-end matching between the AGW and the retrograde sphincterotome and has been described by Monkemuller et al[20] and Chang et al[26] as a rendezvous technique.
Figure 5.
Insertion of the sphincterotome into the antegrade guidewire (AGW) exiting the biliary orifice. End-to-end matching is attempted between the AGW and the sphincterotome. Then, the sphincterotome is placed into the AGW exiting the biliary orifice. Retrograde cannulation with the sphincterotome is attempted over the AGW. AGW = antegrade guidewire.
The technique in which a retrograde GW is inserted after antegrade balloon dilation of the biliary orifice (Fig. 6), first described by Shorvon et al,[12] can be useful for patients with huge bile duct stones in whom removal of the bile duct stone is difficult using the antegrade pushing method alone by an interventional radiologist, and therefore, retrograde pulling power is needed.
The strengths of the current study include reporting the potential indications for PE-RV over EUS-RV, suggesting the Push-pull techniques for overcoming tight hilar biliary strictures or difficult approaches to the biliary orifice, and describing diverse PE cannulation techniques. Nevertheless, the study has several limitations. The main limitation is potential bias related to its retrospective design and long-term data collection such as patient selection, incompleteness of patient information, and the changes in the proficiency of the technique over time. To minimize selection and information bias, we used a prospectively designed fill-in ERC database to record the demographics and ERC results of each patient. Another limitation is the lack of a direct comparison of EUS-RV and PE-RV. In this study, potential indications for PE-RV over EUS-RV were theoretically determined by our institution's experience and literature review. Therefore, our classification of the potential indications for PE-RV and EUS-RV should be re-verified by a future well-designed comparative study. Moreover, if the scope of the procedure is expanded to include balloon-assisted ERCP or EUS-guided antegrade intervention, some of the indications for PE-RV described in this study would be no longer valid. Therefore, our classification is valid only when comparing PE-RV and EUS-RV without considering balloon-assisted ERCP or other EUS-guided interventions. As a final limitation, adjunctive PE-RV cannulation techniques described in the study were performed in a limited number of cases. Therefore, their clinical relevance beyond classic or parallel techniques should be evaluated.
In conclusion, PE-RV has unique technological and clinical indications that distinguish it from EUS-RV. Therefore, PE-RV can still be considered a useful salvage technique for the treatment of biliary obstruction when therapeutic ERC fails. Future large-scale prospective studies comparing PE-RV and EUS-RV or comparing various cannulation PE-RV techniques are needed.
Acknowledgments
We would like to extend a special thanks to Sang Hun Lee, RN, from Ajou University Hospital, who participated in all the PE-RV procedures as a technical assistant for 10 years.
Footnotes
Abbreviations: ERC = endoscopic retrograde cholangiography, EUS-RV = endoscopic ultrasound-guided rendezvous, PE-RV = percutaneous-endoscopic rendezvous.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Schöfl R. Diagnostic endoscopic retrograde cholangiopancreatography. Endoscopy 2001;33:147–57. [DOI] [PubMed] [Google Scholar]
- [2].Adler DG, Baron TH, Davila RE, et al. ASGE guideline: the role of ERCP in diseases of the biliary tract and the pancreas. Gastrointest Endosc 2005;62:1–8. [DOI] [PubMed] [Google Scholar]
- [3].Bakman YG, Freeman ML. Difficult biliary access at ERCP. Gastrointest Endosc Clin N Am 2013;23:219–36. [DOI] [PubMed] [Google Scholar]
- [4].Iwashita T, Lee JG. Endoscopic ultrasonography-guided biliary drainage: rendezvous technique. Gastrointest Endosc Clin N Am 2012;22:249–58. viii–ix. [DOI] [PubMed] [Google Scholar]
- [5].Park DH, Jeong SU, Lee BU, et al. Prospective evaluation of a treatment algorithm with enhanced guidewire manipulation protocol for EUS-guided biliary drainage after failed ERCP (with video). Gastrointest Endosc 2013;78:91–101. [DOI] [PubMed] [Google Scholar]
- [6].Iwashita T, Doi S, Yasuda I. Endoscopic ultrasound-guided biliary drainage: a review. Clin J Gastroenterol 2014;7:94–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Iwashita T, Yasuda I, Mukai T, et al. EUS-guided rendezvous for difficult biliary cannulation using a standardized algorithm: a multicenter prospective pilot study (with videos). Gastrointest Endosc 2016;83:394–400. [DOI] [PubMed] [Google Scholar]
- [8].Kahaleh M, Artifon EL, Perez-Miranda M, et al. Endoscopic ultrasonography guided biliary drainage: summary of consortium meeting, May 7th, 2011, Chicago. World J Gastroenterol 2013;19:1372–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Kawakubo K, Isayama H, Sasahira N, et al. Clinical utility of an endoscopic ultrasound-guided rendezvous technique via various approach routes. Surg Endosc 2013;27:3437–43. [DOI] [PubMed] [Google Scholar]
- [10].Tomizawa Y, Di Giorgio J, Santos E, et al. Combined interventional radiology followed by endoscopic therapy as a single procedure for patients with failed initial endoscopic biliary access. Dig Dis Sci 2014;59:451–8. [DOI] [PubMed] [Google Scholar]
- [11].Park DH, Jang JW, Lee SS, et al. EUS-guided biliary drainage with transluminal stenting after failed ERCP: predictors of adverse events and long-term results. Gastrointest Endosc 2011;74:1276–84. [DOI] [PubMed] [Google Scholar]
- [12].Shorvon PJ, Cotton PB, Mason RR, et al. Percutaneous transhepatic assistance for duodenoscopic sphincterotomy. Gut 1985;26:1373–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Brambs HJ, Billmann P, Pausch J, et al. Non-surgical biliary drainage: endoscopic conversion of percutaneous transhepatic into endoprosthetic drainage. Endoscopy 1986;18:52–4. [DOI] [PubMed] [Google Scholar]
- [14].Robertson DA, Ayres R, Hacking CN, et al. Experience with a combined percutaneous and endoscopic approach to stent insertion in malignant obstructive jaundice. Lancet 1987;2:1449–52. [DOI] [PubMed] [Google Scholar]
- [15].Tsang TK, Crampton AR, Bernstein JR, et al. Percutaneous-endoscopic biliary stent placement. A preliminary report. Ann Intern Med 1987;106:389–92. [DOI] [PubMed] [Google Scholar]
- [16].Dowsett JF, Vaira D, Hatfield AR, et al. Endoscopic biliary therapy using the combined percutaneous and endoscopic technique. Gastroenterology 1989;96:1180–6. [DOI] [PubMed] [Google Scholar]
- [17].Hunt JB, Sayer JM, Jacyna M, et al. Combined percutaneous transhepatic and endoscopic placement of biliary stents. Surg Oncol 1993;2:293–8. [DOI] [PubMed] [Google Scholar]
- [18].Verstandig AG, Goldin E, Sasson T, et al. Combined transhepatic and endoscopic procedures in the biliary system. Postgrad Med J 1993;69:384–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Calvo MM, Bujanda L, Heras I, et al. The rendezvous technique for the treatment of choledocholithiasis. Gastrointest Endosc 2001;54:511–3. [DOI] [PubMed] [Google Scholar]
- [20].Monkemuller KE, Linder JD, Fry LC. Modified rendezvous technique for biliary cannulation. Endoscopy 2002;34:936. [DOI] [PubMed] [Google Scholar]
- [21].Wayman J, Mansfield JC, Matthewson K, et al. Combined percutaneous and endoscopic procedures for bile duct obstruction: simultaneous and delayed techniques compared. Hepatogastroenterology 2003;50:915–8. [PubMed] [Google Scholar]
- [22].Dickey W. Parallel cannulation technique at ERCP rendezvous. Gastrointest Endosc 2006;63:686–7. [DOI] [PubMed] [Google Scholar]
- [23].Cariani G, Di Marco M, Solmi L. Parallel rendezvous in ERCP. Gastrointest Endosc 2006;64:669. [DOI] [PubMed] [Google Scholar]
- [24].Liu YD, Wang ZQ, Wang XD, et al. Stent implantation through rendezvous technique of PTBD and ERCP: the treatment of obstructive jaundice. J Dig Dis 2007;8:198–202. [DOI] [PubMed] [Google Scholar]
- [25].Kim HJ, Cho YK, Jeon WK, et al. Bile duct cannulation guided by a percutaneous transhepatic biliary drainage tube in cases of difficult cannulation: modified rendezvous procedure. J Gastroenterol Hepatol 2007;22:766–7. [DOI] [PubMed] [Google Scholar]
- [26].Chang JH, Lee IS, Chun HJ, et al. Usefulness of the rendezvous technique for biliary stricture after adult right-lobe living-donor liver transplantation with duct-to-duct anastomosis. Gut Liver 2010;4:68–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Lee TH, Park SH, Lee SH, et al. Modified rendezvous intrahepatic bile duct cannulation technique to pass a PTBD catheter in ERCP. World J Gastroenterol 2010;16:5388–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Neal CP, Thomasset SC, Bools D, et al. Combined percutaneous-endoscopic stenting of malignant biliary obstruction: results from 106 consecutive procedures and identification of factors associated with adverse outcome. Surg Endosc 2010;24:423–31. [DOI] [PubMed] [Google Scholar]
- [29].Albert JG, Finkelmeier F, Friedrich-Rust M, et al. Identifying indications for percutaneous (PTC) vs. endoscopic ultrasound (EUS)- guided “rendezvous” procedure in biliary obstruction and incomplete endoscopic retrograde cholangiography (ERC). Z Gastroenterol 2014;52:1157–63. [DOI] [PubMed] [Google Scholar]
- [30].Itoi T, Ishii K, Sofuni A, et al. Single balloon enteroscopy-assisted ERCP using rendezvous technique for sharp angulation of Roux-en-Y limb in a patient with bile duct stones. Diagn Ther Endosc 2009;2009:154084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Tsutsumi K, Kato H, Okada H, et al. Usefulness of the rendezvous technique for deep scope insertion during endoscopic retrograde cholangiography in a patient with a Roux-en-Y hepaticojejunostomy. Endoscopy 2014;46(suppl 1 UCTN):E619–20. [DOI] [PubMed] [Google Scholar]
- [32].Yamauchi H, Kida M, Imaizumi H, et al. Innovations and techniques for balloon-enteroscope-assisted endoscopic retrograde cholangiopancreatography in patients with altered gastrointestinal anatomy. World J Gastroenterol 2015;21:6460–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Committee AT, Maple JT, Pannala R, et al. Interventional EUS (with videos). Gastrointest Endosc 2017;85:465–81. [DOI] [PubMed] [Google Scholar]
- [34].Park SJ, Choi JH, Park DH, et al. Expanding indication: EUS-guided hepaticoduodenostomy for isolated right intrahepatic duct obstruction (with video). Gastrointest Endosc 2013;78:374–80. [DOI] [PubMed] [Google Scholar]
- [35].Ogura T, Onda S, Sano T, et al. EUS-guided antegrade balloon dilation from right hepatic duct combined with retrograde rendezvous stent placement. Gastroenterology 2015;148:901–3. [DOI] [PubMed] [Google Scholar]
- [36].Ogura T, Sano T, Onda S, et al. Endoscopic ultrasound-guided biliary drainage for right hepatic bile duct obstruction: novel technical tips. Endoscopy 2015;47:72–5. [DOI] [PubMed] [Google Scholar]


