Abstract
Objective:
This meta-analysis aimed to compare the efficiency and safety of local liposomal bupivacaine infiltration and traditional cocktail analgesia for pain management in total hip arthroplasty (THA).
Methods:
PubMed, Embase, Web of science, Medline, and Cochrane library databases were systematically searched. Inclusion criteria: Participants: patients planned for a THA with a diagnosis of hip osteoarthritis. Interventions: liposomal bupivacaine was administrated in the experimental groups for pain control. Comparisons: the control groups received local infiltration of traditional analgesics. Outcomes: pain scores, opioids consumption, and postoperative complications among the patients. Study design: randomized control trials (RCTs) and non-RCTs. Methodological Index for Non-Randomized Studies scale was used to assess the methodological quality of the included studies. Meta-analysis was conducted by Stata 11.0 software. Systematic review registration number is CRD42017120981.
Results:
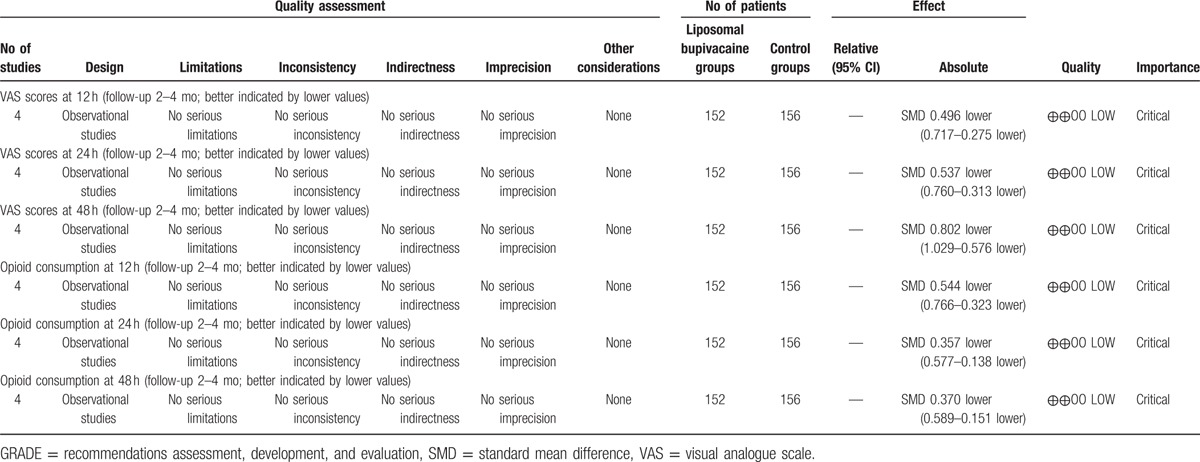
Four articles involving 308 participants were included. Current meta-analysis revealed that there were significant differences regarding postoperative pain score at 12 hours (standard mean difference [SMD] = −0.496, 95% CI: −0.717 to −0.275, P = .000), 24 hours (SMD = −0.537, 95% CI: −0.760 to −0.313, P = .000), and 48 hours (SMD = −0.802, 95% CI: −1.029 to −0.576, P = .000). Liposomal bupivacaine intervention was found to significantly decrease opioid consumption at 12 hours (SMD = −0.544, 95% CI: −0.766 to −0.323, P = .000), 24 hours (SMD = −0.357, 95% CI: −0.577 to −0.138, P = .001), and 48 hours (SMD = −0.370, 95% CI: −0.589 to −0.151, P = .001).
Conclusion:
Local liposomal bupivacaine infiltration could significantly reduce visual analogue scale (VAS) scores and opioid consumption within the first 48 hours following THA surgery. In addition, there was a decreased risk of nausea and vomiting in liposomal bupivacaine groups. The overall evidence level was low, which means that further research is likely to significantly alter confidence levels in the effect, as well as potentially changing the estimates. In any subsequent research, further studies should focus on the optimal dose of local anesthetics and the potential adverse side effects. In addition, surgeries that can improve pain relief and enable faster rehabilitation and earlier discharges should also be explored. Several potential limitations of this study should be noted. Four articles are included and the sample size in each trial is small. Some important outcome parameters such as range of motion were not fully described and could not be included in the meta-analysis. All included studies were retrospectives which may decrease evidence levels for the meta-analysis. The evidence quality for each outcome was low which may influence the results of the meta-analysis. Short-term follow-ups may lead to the underestimation of complications, such as neurotoxicity and cardiotoxicity. Publication bias is an inherent weakness that exists in all meta-analyses.
Keywords: liposomal bupivacaine, meta-analysis, pain control, total hip arthroplasty, traditional cocktail analgesia
1. Introduction
Total hip arthroplasty (THA) is a successful surgical procedure for the treatment of end-stage joint osteoarthritis.[1] With an aging population, the incidence of THA has risen sharply. It was reported that more than 330,000 of THAs were performed in the United States in 2011. By 2030, the demand for THA procedures is expected to increase to 500,000 producers annually.[2] However, THA is usually associated with moderate to severe postoperative pain which is recognized as an important problem associated with a functional recovery. Many strategies have been applied to reduce postoperative pain including peripheral nerve blocks, systemic morphine, and an epidural analgesia.[3–6] However, no consensus of gold standards for effective pain control following a THA was reached. Thus, pain management after a THA procedure was an interesting topic in the field of joint surgery.
Local infiltration analgesia has been recommended for postoperative pain management. An analgesia cocktail consisting of a mixture of ropivacaine, ketorolac, and opioid has been commonly used. Several studies have reported the various benefits for analgesia after joint arthroplasty surgery.[7–10] However, a short duration of action limits the clinical application. Liposomal bupivacaine is a long-lasting anesthetic. The acting process is that bupivacaine is encapsulated into multivesicular liposomes, making it a slow release treatment, with a controlled release from the liposomes.[11] The use of this time-released suspension in a total knee arthroplasty is well established and has demonstrated improved outcome and less complications.[12]
Currently, comparisons of local liposomal bupivacaine infiltration and traditional cocktail analgesia for pain management in THA have been seldom reported. Thus, there is a lack of scientific evidence. Therefore, we performed a meta-analysis from controlled clinical trials, to compare the efficacy and safety of local liposomal bupivacaine infiltration and traditional cocktail analgesia for pain management in THA procedures. Only adult participants with a diagnosis of end-stage hip osteoarthritis, and were prepared for a unilateral THA, were included in our study. The results outcomes were visual analogue scale (VAS) scores in different periods, opioids consumption, length of stay and postoperative complications among the participants.
2. Methods
This meta-analysis was reported according to the preferred reporting items for systematic reviews and meta-analyses guidelines. All analyses were based on previous published studies, thus no ethical approval and patient consent are required. Systematic review registration number is CRD42017120981.
2.1. Search strategy
Potentially relevant studies were identified from electronic databases including Medline (1966–2017.06.30), PubMed (1966–2017.06.30), Embase (1980–2017.06.30), ScienceDirect (1985–2017.06.30), and the Web of Science (1950–2017.06.30). The following key words were used on combination with Boolean operators AND or OR: “total hip replacement OR arthroplasty,” “liposomal bupivacaine,” “cocktail analgesia,” and “pain control.” Complete search strategy for Embase was shown Table 1. No restrictions were imposed on language. The bibliographies of retrieved trials and other relevant publications were cross-referenced to identify additional articles. The search process was performed as presented in Fig. 1.
Table 1.
EMBASE search strategy.
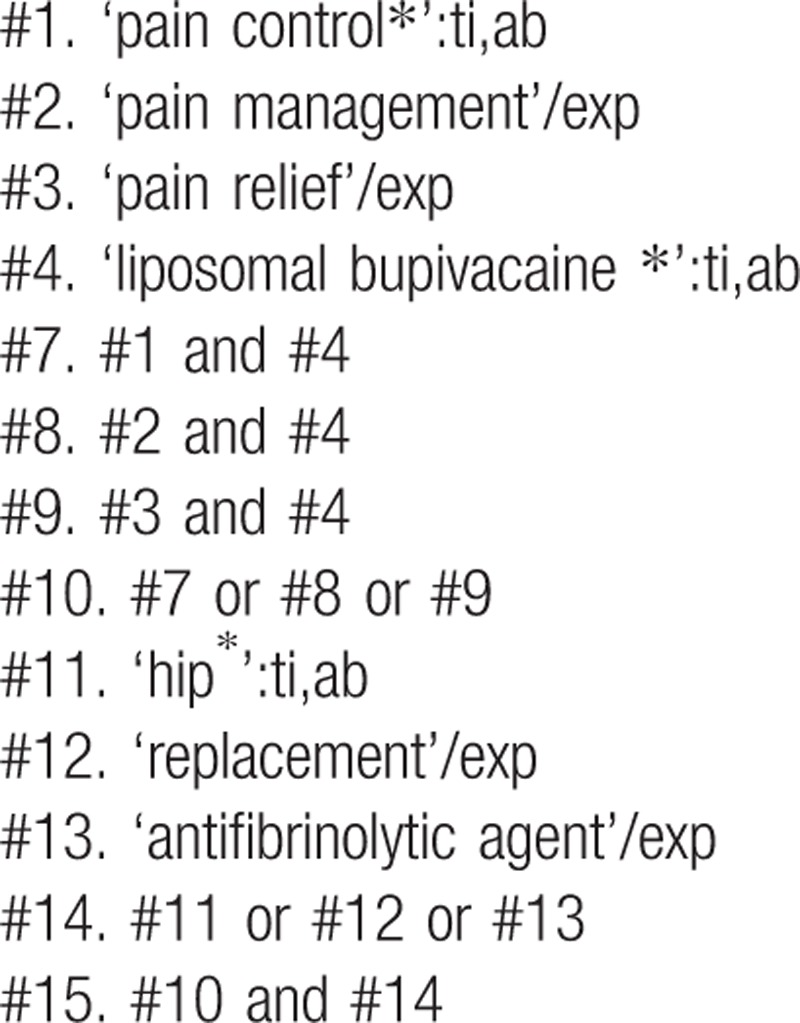
Figure 1.
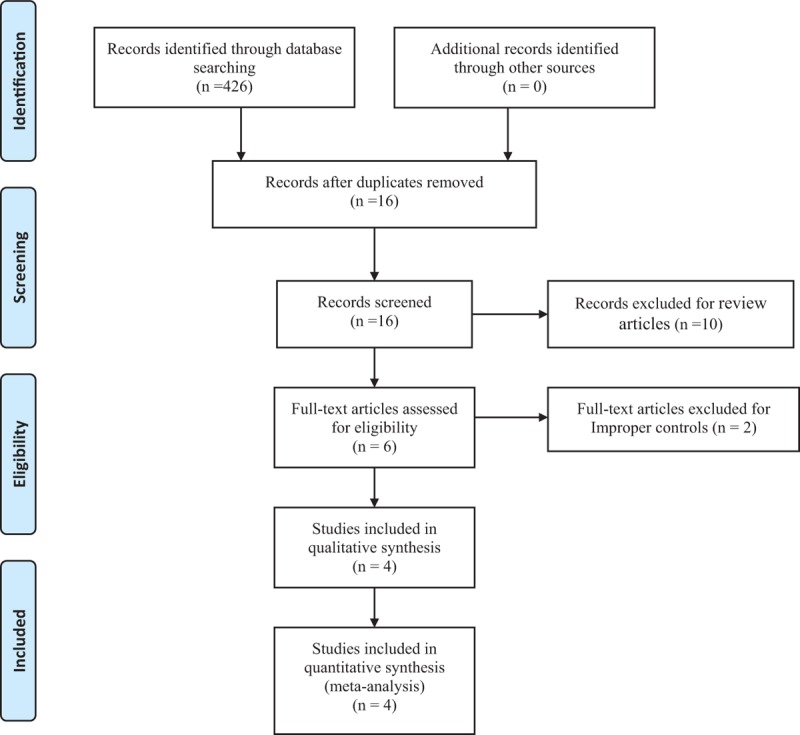
Search results and the selection procedure.
2.2. Inclusion and exclusion criteria
Inclusion criteria: participants: only published articles enrolling adult participants that with a diagnosis of end-stage of hip osteoarthritis and prepared for unilateral THA. Interventions: the intervention group received local liposomal bupivacaine infiltration for postoperative pain management after THA. Comparisons: the control group was received traditional local infiltration for postoperative pain control. Outcomes: VAS scores in different periods, opioids consumption, length of stay, and postoperative complications. Study design: clinical randomized control trials (RCTs) and non-RCTs were regarded as eligible in our study.
Exclusion criteria: articles would be excluded from the present meta-analysis for case reports, conference abstract, or review articles.
2.3. Selection criteria
Two reviewers independently scanned the abstracts of the potential articles identified by the above searches. Subsequently, the full text of the studies that met the inclusion criteria was screened, and a final decision was made. A senior author had the final decision in any case of disagreement regarding which studies to include.
2.4. Data extraction
A standard form for date extraction is printed for date extraction. Two of the authors independently extracted data from the included studies: first author names, publication year, samples size, baseline characteristics, intervention procedures, anesthesia method, and outcome parameters. Other relevant data were also extracted from individual studies. Primary outcomes were VAS scores and opioids consumption in different periods. Secondary outcomes were length of hospital stay and postoperative complications. The corresponding authors were consulted for details of data that were incomplete. Any disagreements were resolved through discussion.
2.5. Quality assessment
Methodological Index for Non-Randomized Studies scale, which assigns scores ranging from 0 to 24, was used to assess the methodological quality of the included studies in the present meta-analysis which was based on the 12 main items. The quality of the evidence for the main outcomes in present meta-analysis was evaluated using the Recommendations Assessment, Development, and Evaluation (GRADE) system including the following items: risk of bias, inconsistency, indirectness, imprecision, and publication bias. The recommendation level of evidence is classified into the following categories: high, which means that further research is unlikely to change confidence in the effect estimate; moderate, which means that further research is likely to significantly change confidence in the effect estimate but may change the estimate; low, which means that further research is likely to significantly change confidence in the effect estimate and to change the estimate; and very low, which means that any effect estimate is uncertain. Publication bias is a tendency on average to produce results that appear significant, because negative or near neutral results are almost never published. Funnel plot was used to assess the publication bias of the main outcomes.
2.6. Data analysis and statistical methods
Pooling of data was carried out using Stata 11.0 software (The Cochrane Collaboration, Oxford, UK). Statistical heterogeneity was evaluated based on the value of P and I2 using standard χ2 test. When I2>50%, P < .1 was considered to be significant heterogeneity, the random-effect model was used for meta-analysis. Otherwise, the fixed-effect model was performed. Sensibility analysis is conducted to assess the origins of heterogeneity. The results of dichotomous outcomes (postoperative complications) were expressed as risk difference (RD) with 95% confidence intervals (CIs). For continuous various outcomes (VAS scores, opioids consumption, and length of stay), mean difference, or standard mean difference (SMD) with a 95% CIs was applied for the assessment. A subgroup analysis was conducted for the main outcomes.
3. Results
3.1. Search result
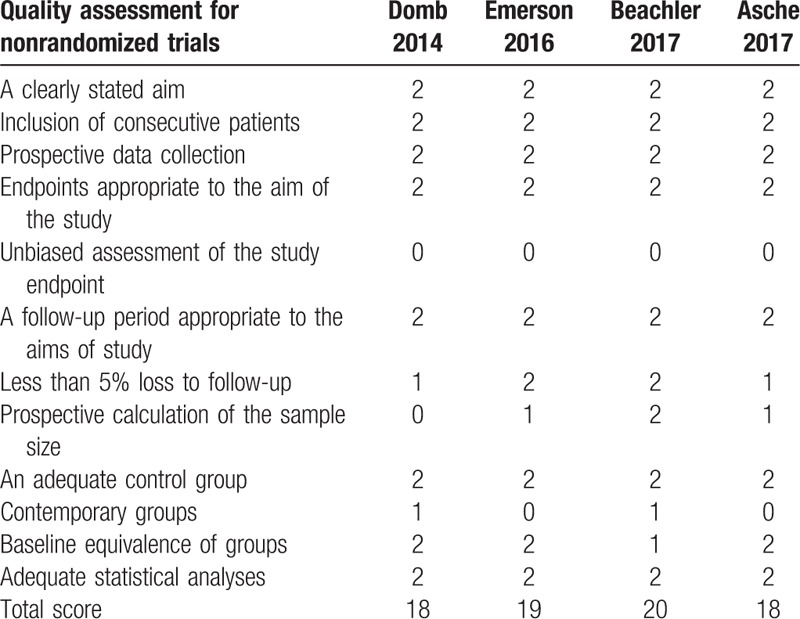
A total of 426 studies were identified through an initial search. By scanning the abstracts, 410 articles were removed for duplication and 10 records were removed as they were review articles only. After scanning the full papers, 2 articles were removed due to unsuitable controls. No gray literature was included. Finally, 4 studies[14–17] published between 2014 and 2017 were included in the present meta-analysis and all the studies were published in English. These studies included 152 patients in the experimental groups and 156 patients in the control groups. The characteristics of the included studies are reported in Table 2. The quality assessment of the included studies can be seen in detail in Table 3.
Table 2.
Trials characteristics.
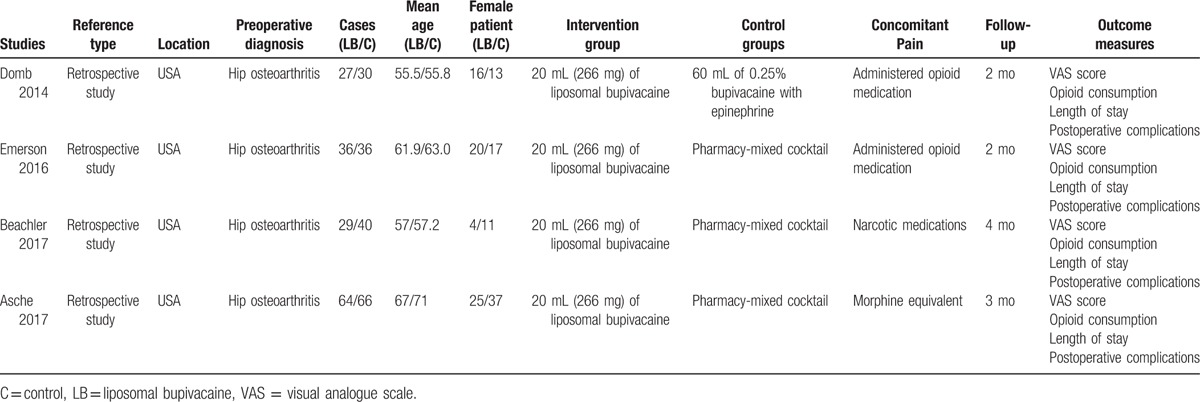
Table 3.
Methodological quality of the included studies.
3.2. Study characteristics
The sample size of the included studies ranged from 57 to 130. All of them compared the analgesic efficiencies between local liposomal bupivacaine infiltration and traditional local infiltration analgesia in THA. There are variations in dosage and types of local anesthetics among the groups. All the patients received general anesthesia for their surgery. All articles highlighted that THAs were performed by the same surgical teams. All the participants received narcotic medications as an adjunct to the concomitant pain management. All the studies suggest outcomes for at least 95% of the patients and follow-up period ranged from 2 to 4 months.
3.3. Outcomes for meta-analysis
3.3.1. VAS scores at 12 hours
Four articles showed the outcomes of VAS scores at 12 hours after THA. A fixed-effects model was used because no significant heterogeneity was found among the studies (χ2 = 5.42, df = 3, I2 = 44.6%, P = .144). The pooled results demonstrated that significant difference in VAS scores at 12 hour was found between 2 groups (SMD = −0.496, 95% CI: −0.717 to −0.275, P = .000, power = 86%; Fig. 2).
Figure 2.
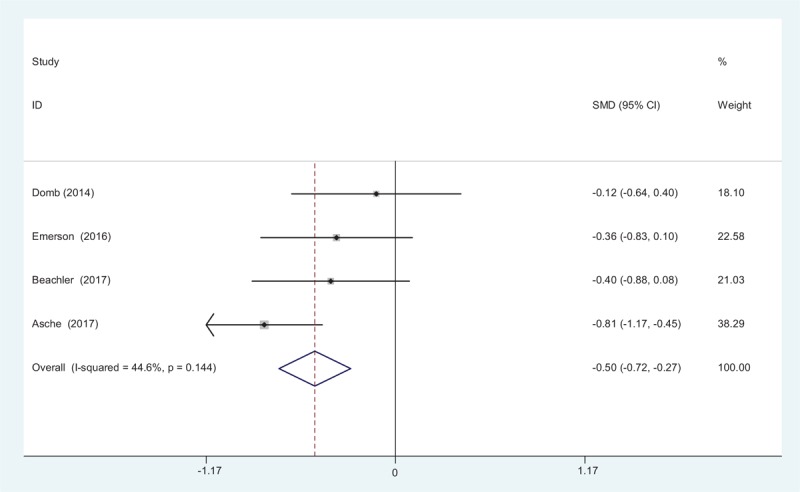
Forest plot diagram showing VAS scores at 12 hours following THA. THA = total hip arthroplasty, VAS = visual analogue scale.
3.3.2. VAS scores at 24 hours
Four studies reported the outcomes of VAS scores at 24 hours after THA. A random-effects model was used because significant heterogeneity was found among the studies (χ2 = 15.01, df = 3, I2 = 80.0%, P = .002). The pooled results demonstrated that there was significant difference in VAS scores at 24 hours between groups (SMD = −0.537, 95% CI: −0.760 to −0.313, P = .000, power = 82%; Fig. 3).
Figure 3.
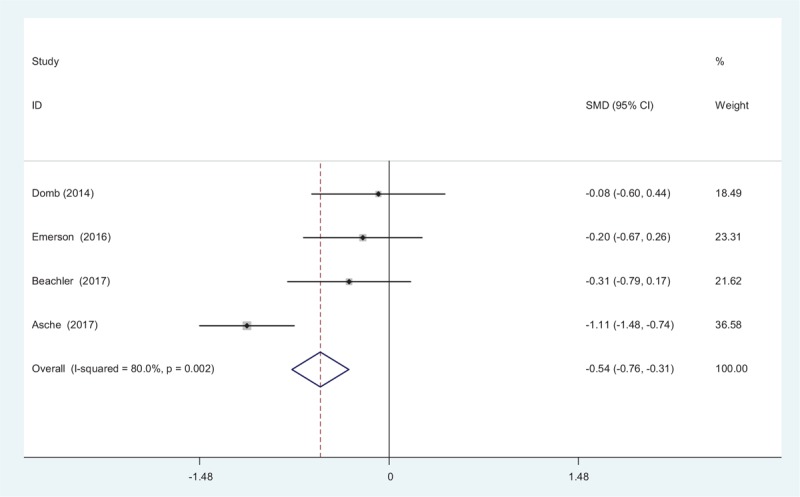
Forest plot diagram showing VAS scores at 24 hours following THA. THA = total hip arthroplasty, VAS = visual analogue scale.
3.3.3. VAS scores at 48 hours
Four studies reported the outcomes of VAS scores at 48 hours after THA. A fixed-effects model was used because no significant heterogeneity existed among these studies (χ2 = 3.85, df = 3, I2 = 22.1%, P = .278). The pooled results demonstrated that significant difference in VAS scores at 48 hours was identified between groups (SMD = −0.802, 95% CI: −1.029 to −0.576, P = .000, power = 88%; Fig. 4).
Figure 4.
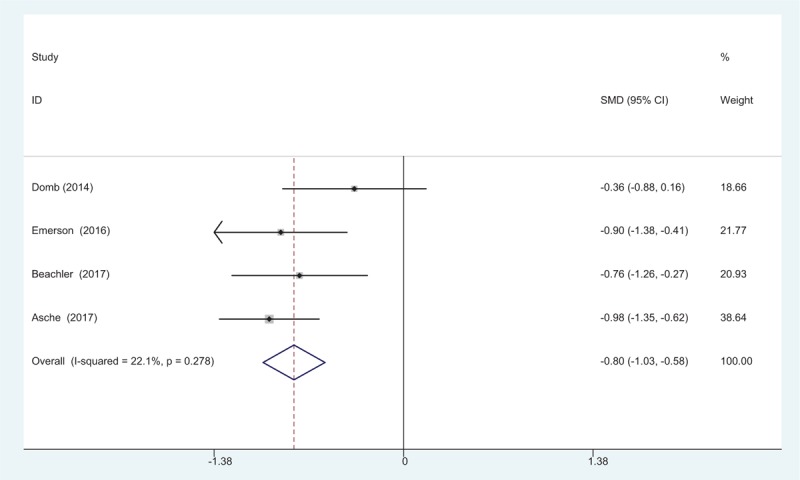
Forest plot diagram showing VAS scores at 48 hours following THA. THA = total hip arthroplasty, VAS = visual analogue scale.
3.3.4. Opioids consumption at 12 hours
Opioids consumption at 12 hours after THA was reported in 4 articles. A fixed-effects model was applied because no significant heterogeneity was found among these studies (χ2 = 1.16, df = 3, I2 = 0%, P = .762). Significant difference was detected in opioids consumption at 12 hours between the 2 groups (SMD = −0.544, 95% CI: −0.766 to −0.323, P = .000, power = 80%; Fig. 5).
Figure 5.
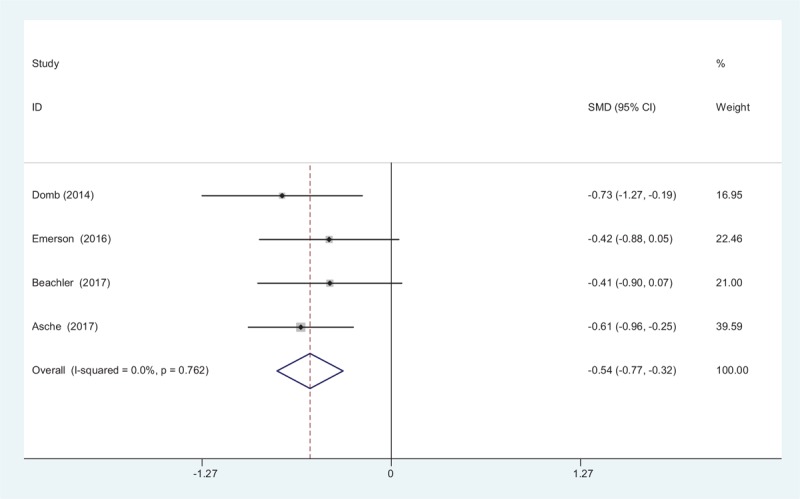
Forest plot diagram showing opioid consumption at 12 hours following THA. THA = total hip arthroplasty.
3.3.5. Opioids consumption at 24 hours
Opioids consumption at 24 hours after THA was provided in 4 studies. A fixed-effects model was used because no significant heterogeneity was found among these studies (χ2 = 4.31, df = 3, I2 = 30.4%, P = .230). The pooled results demonstrated that there was significant difference in opioids consumption at 24 hours between groups (SMD = −0.357, 95% CI: −0.577 to −0.138, P = .001, power = 83%; Fig. 6).
Figure 6.
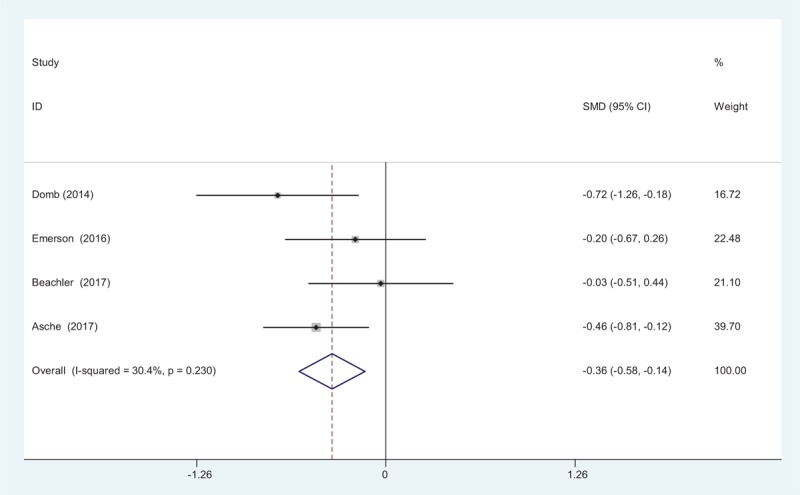
Forest plot diagram showing opioid consumption at 24 hours following THA. THA = total hip arthroplasty.
3.3.6. Opioids consumption at 48 hours
Four articles reported the outcomes of opioids consumption at 48 hours after THA. A fixed-effects model was used because no significant heterogeneity was found among the pooled data (χ2 = 0.69, df = 3, I2 = 0%, P = .875). Significance difference in opioids consumption at 48 hours was observed between the 2 groups. (SMD = −0.370, 95% CI: −0.589 to −0.151, P = .001, power = 86%; Fig. 7).
Figure 7.
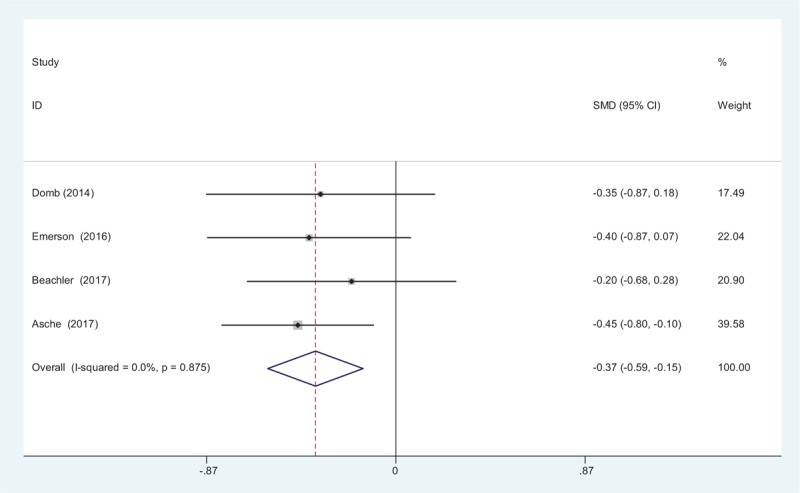
Forest plot diagram showing opioid consumption at 48 hours following THA. THA = total hip arthroplasty.
3.3.7. Length of hospital stay
Four studies reported the length of hospital stay for the groups. A fixed-effects model was used because no significant heterogeneity was identified in the pooled results (χ2 = 2.97, df = 3, I2 = 0%, P = .397). No significant difference in the length of hospital stay was observed between the 2 groups (SMD = −0.009, 95% CI: −0.227 to 0.209, P = .935, power = 90%; Fig. 8).
Figure 8.
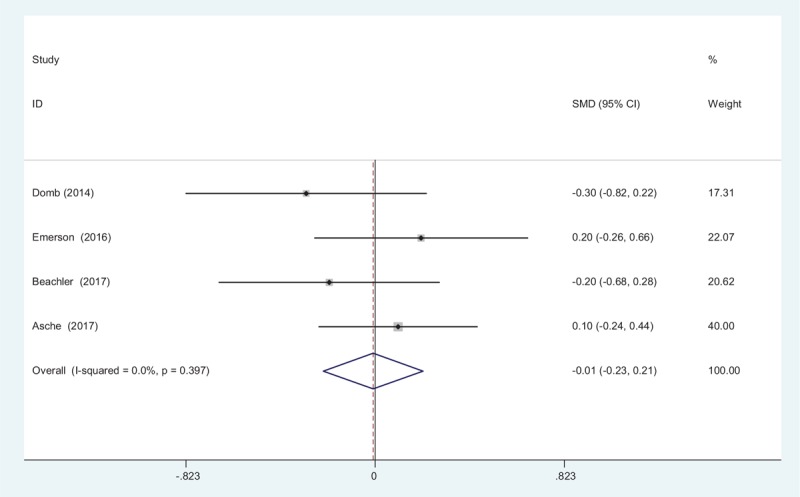
Forest plot diagram showing length of stay following THA. THA = total hip arthroplasty.
3.3.8. Nausea
Four studies reported the postoperative complications of nausea. A fixed-effects model was used because no significant heterogeneity was found among these studies (χ2 = 2.68, df = 3, I2 = 0%, P = .443). Significant difference in the incidence of nausea was found between the 2 groups (RD = −0.127, 95% CI: −0.234 to −0.021, P = .019, power = 91%; Fig. 9).
Figure 9.
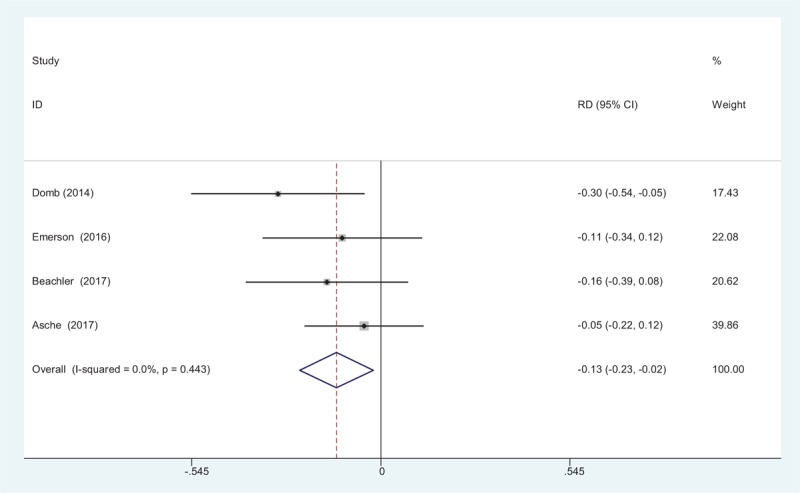
Forest plot diagram showing incidence of nausea following THA. THA = total hip arthroplasty.
3.3.9. Vomiting
Four articles reported the postoperative complications of vomiting following THA. A fixed-effects model was used due to the low significant heterogeneity among these studies (χ2 = 2.03, df = 3, I2 = 0%, P = .566). Significant difference was found in terms of the incidence of vomiting between the groups (RD = −0.103, 95% CI: −0.205 to −0.002, P = .045, power = 91%; Fig. 10).
Figure 10.
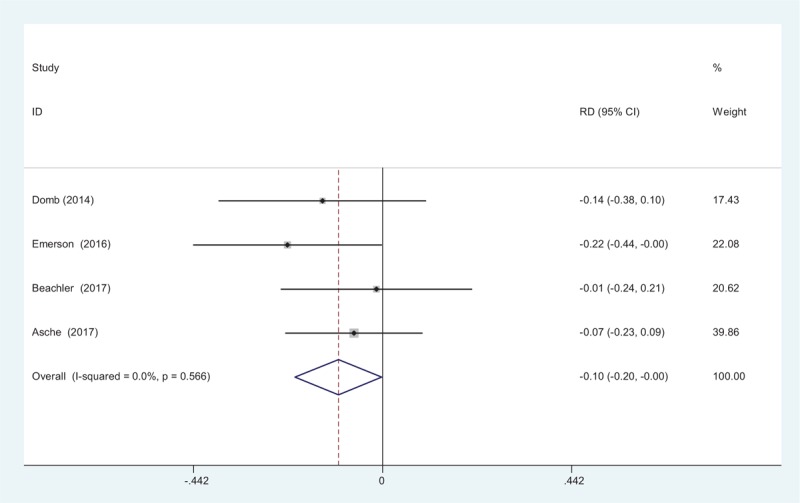
Forest plot diagram showing incidence of vomiting following THA. THA = total hip arthroplasty.
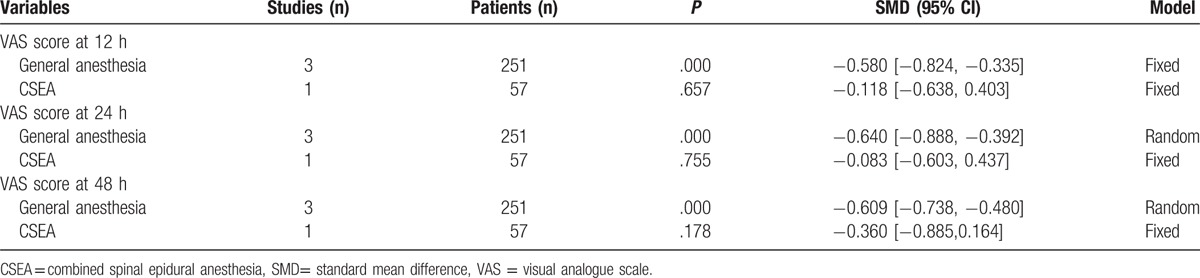
3.4. Publication bias and subgroup analysis
Publication bias was performed for the VAS score and opioid consumption at 12 hours. The funnel plots were symmetrical, indicating a low risk of publication bias (Figs. 11 and 12); however, publication bias could not be excluded, as the reliability of this kind of assessment was weak, especially as a low number of studies were included. The result of the subgroup analysis was presented in Table 4.
Figure 11.
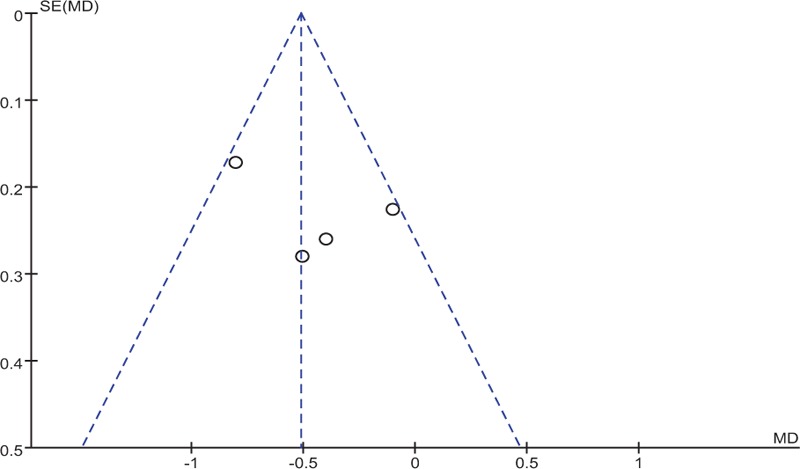
Funnel plot of VAS score at 12 hours. VAS = visual analogue scale.
Figure 12.
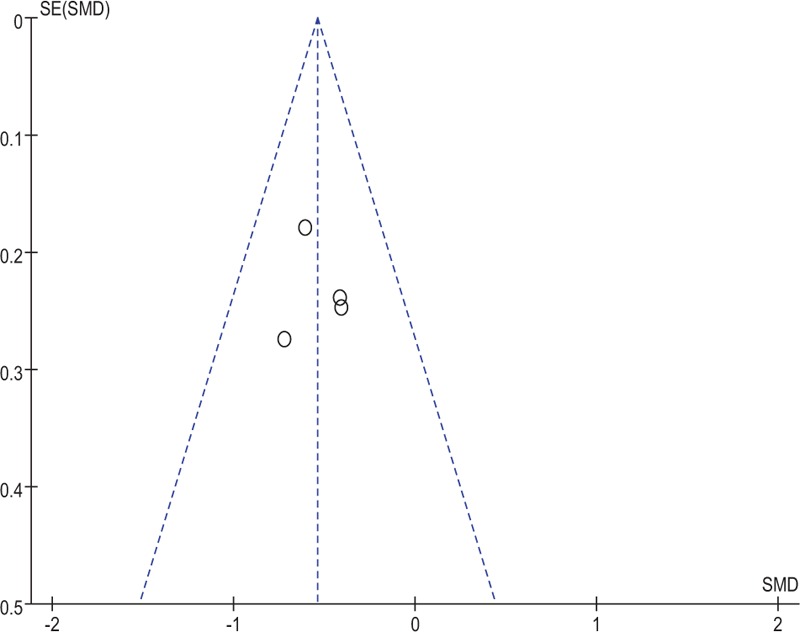
Funnel plot of opioid consumption at 12 hours.
Table 4.
Subgroup analysis.
4. Discussion
To the best of our knowledge, this is the first meta-analysis that compares the effectiveness and safety of local liposomal bupivacaine infiltration and traditional cocktail analgesia for pain management in THA surgery. The most important finding of the present meta-analysis was that local liposomal bupivacaine infiltration could significantly reduce the VAS scores and morphine consumptions within the first 48 hours after THA surgery. Moreover, there is a decreased risk of nausea and vomiting in liposomal bupivacaine groups compared with controlled groups. All outcomes in this meta-analysis were evaluated using the GRADE system. The evidence quality for each outcome was low (Table 5), which means that further research is likely to significantly alter confidence levels in the effect, as well as potentially changing the estimates.
Table 5.
The GRADE evidence quality for main outcome.
Consensus has been reached that effective pain control following major orthopedic surgery is important for functional recovery and reducing postoperative complications. Multimodal pain management following THA surgery has been shown to improve pain relief and reduce opioid consumption.[18,19] Local infiltration anesthesia is widely used and shows excellent outcomes for pain relief after THA. However, this approach has been criticized because of its short-term pain relief. Liposomal bupivacaine is a long-lasting, local anesthetic that is injected via a single-dose infiltration to produce an analgesic effect.[20] The drug was approved by the Food and Drug Administration in 2011. During the active process, bupivacaine is encapsulated into multivesicular liposomes, resulting in a slow and controlled release from the liposomes. Therefore, the analgesic effect can be sustained 72 hours up to 96 hours.[21] Furthermore, local administration of anesthetics is a simple technique that can be performed without an anesthetist. Kuang et al[22] showed that liposomal bupivacaine infiltration promotes superior pain relief and less postoperative complications compared traditional bupivacaine after total knee arthroplasty. Liu et al[23] found that local liposomal bupivacaine injection provided a significant beneficial effect over femoral nerve block in improving the pain in major orthopedic surgery. VAS scores in different periods after the THA surgery were the primary outcomes that were studied in our meta-analysis. The present meta-analysis indicated that local liposomal bupivacaine infiltration in THA could significantly reduce pain scores within the first 48 hours. Opioid consumption was also an important indicator for assessing the analgesic effect of liposomal bupivacaine. It was normally used as adjunct to a multimodal analgesia protocol. Also, the analgesic effect of the additional opioids provides a long postoperative period without any pain experienced by the participants. Opioid consumption is also considered an objective method of measuring pain. However, previous studies have frequently reported that patients have experienced drug-related side effects, such as nausea, vomiting, headache, and respiratory depression.[24,25] Moreover, long-term opioid use may result in drug dependence which is an important issue that should be considered. Effective analgesia protocol is crucial to reduce the consumption of opioids. A substantial number of previous studies have reported that the liposomal bupivacaine could decrease inpatient narcotic requirements in major orthopedic surgery. However, local administration of liposomal bupivacaine in THA was seldom reported. Conducting a meta-analysis can strengthen statistical power and enlarger the sample size by pooling results of published studies, which could identify stronger evidence to support study outcomes. The present meta-analysis indicated that local liposomal bupivacaine infiltration could significantly reduce opioid consumption in the first 48 hours after THA, compared with controls. Postoperative complications were major concerns following additional opioids. Nausea and vomiting are well-known side effects that are related to the systemic use of morphine. Adequate analgesia protocol could decrease opioid consumption and subsequently decrease the risk of postoperative complications. The present meta-analysis demonstrated that local liposomal bupivacaine infiltration could significantly decrease the incidence of nausea and vomiting. Considering that only 4 studies were included in our study, large sample sizes from high-quality studies should be conducted in the future. A risk of bias should also be considered when interpreting the findings.
For patients: the current data supports the finding that local liposomal bupivacaine infiltration could reduce pain and opioid consumption. For policymakers: based on the low evidence of the meta-analysis, more RCTs with large sample size are required to confirm the clinical benefits for the patients. For clinicians: further evidence including clinical and cost effectiveness of liposomal bupivacaine infiltration in THA is required, due to the quality of the evidence.
Several potential limitations of this study should be noted. Only 4 studies were included, and the sample size was relatively small. Some important outcome parameters such as range of motion were not fully described and could not be included in the meta-analysis. All included studies were retrospectives which may decrease evidence levels for the meta-analysis. The evidence quality for each outcome was low which may influence the results of the meta-analysis. Short-term follow-ups may lead to the underestimation of complications, such as neurotoxicity and cardiotoxicity. Publication bias is an inherent weakness that exists in all meta-analyses.
5. Conclusion
Local liposomal bupivacaine infiltration could significantly reduce VAS scores and opioid consumption within the first 48 hours following THA surgery. In addition, there was a decreased risk of nausea and vomiting in liposomal bupivacaine groups. In any subsequent research, further studies should focus on the optimal dose of local anesthetics and the potential adverse side effects. In addition, surgeries that can improve pain relief and enable faster rehabilitation and earlier discharges should also be explored.
Footnotes
Abbreviations: RCT = randomized controlled trials, THA = total hip arthroplasty, VAS = visual analogue scale.
XZ and QY equally contributed to this study.
QY conceived the design of the study. ZZ performed and collected the data and contributed to the design of the study. XZ finished the manuscript. All authors read and approved the final manuscript.
The authors have no conflicts of interest to disclose.
References
- [1].Amstutz HC, Thomas BJ, Jinnah R, et al. Treatment of primary osteoarthritis of the hip. A comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am 1984;66:228–41. [PubMed] [Google Scholar]
- [2].Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780–5. [DOI] [PubMed] [Google Scholar]
- [3].Kuchalik J, Granath B, Ljunggren A, et al. Postoperative pain relief after total hip arthroplasty: a randomized, double-blind comparison between intrathecal morphine and local infiltration analgesia. Br J Anaesth 2013;111:793–9. [DOI] [PubMed] [Google Scholar]
- [4].Singelyn FJ, Ferrant T, Malisse MF, et al. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous femoral nerve sheath block on rehabilitation after unilateral total-hip arthroplasty. Reg Anesth Pain Med 2005;30:452–7. [DOI] [PubMed] [Google Scholar]
- [5].Stevens M, Harrison G, McGrail M. A modified fascia iliaca compartment block has significant morphine-sparing effect after total hip arthroplasty. Anaesth Intensive Care 2007;35:949–52. [DOI] [PubMed] [Google Scholar]
- [6].Wiesmann T, Steinfeldt T, Wagner G, et al. Supplemental single shot femoral nerve block for total hip arthroplasty: impact on early postoperative care, pain management and lung function. Minerva Anestesiol 2014;80:48–57. [PubMed] [Google Scholar]
- [7].Andersen LJ, Poulsen T, Krogh B, et al. Postoperative analgesia in total hip arthroplasty: a randomized double-blinded, placebo-controlled study on peroperative and postoperative ropivacaine, ketorolac, and adrenaline wound infiltration. Acta Orthop 2007;78:187–92. [DOI] [PubMed] [Google Scholar]
- [8].Busch CA, Whitehouse MR, Shore BJ, et al. The efficacy of periarticular multimodal drug infiltration in total hip arthroplasty. Clin Orthop Relat Res 2010;468:2152–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Kuchalik J, Magnuson A, Tina E, et al. Does local infiltration analgesia reduce peri-operative inflammation following total hip arthroplasty? A randomized, double-blind study. BMC Anesthesiol 2017;17:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Lunn TH, Husted H, Solgaard S, et al. Intraoperative local infiltration analgesia for early analgesia after total hip arthroplasty: a randomized, double-blind, placebo-controlled trial. Reg Anesth Pain Med 2011;36:424–9. [DOI] [PubMed] [Google Scholar]
- [11].Branney J, Izadpanah M. Liposomal bupivacaine peripheral nerve block for the management of postoperative pain. Nurs Stand 2017;31:42–3. [DOI] [PubMed] [Google Scholar]
- [12].Schroer WC, Diesfeld PG, LeMarr AR, et al. Does extended-release liposomal bupivacaine better control pain than bupivacaine after total knee arthroplasty (TKA)? A prospective, randomized clinical trial. J Arthroplasty 2015;30(9 suppl):64–7. [DOI] [PubMed] [Google Scholar]
- [13].Wang X, Xiao L, Wang Z, et al. Comparison of peri-articular liposomal bupivacaine and standard bupivacaine for postsurgical analgesia in total knee arthroplasty: a systematic review and meta-analysis. Int J Surg 2017;39:238–48. [DOI] [PubMed] [Google Scholar]
- [14].Asche CV, Ren J, Kim M, et al. Local infiltration for postsurgical analgesia following total hip arthroplasty: a comparison of liposomal bupivacaine to traditional bupivacaine. Curr Med Res Opin 2017;33:1283–90. [DOI] [PubMed] [Google Scholar]
- [15].Beachler JA, Kopolovich DM, Tubb CC, et al. Liposomal bupivacaine in total hip arthroplasty: do the results justify the cost? J Orthop 2017;14:161–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Domb BG, Gupta A, Hammarstedt JE, et al. The effect of liposomal bupivacaine injection during total hip arthroplasty: a controlled cohort study. BMC Musculoskelet Disord 2014;15:310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Emerson RH, Barrington JW, Olugbode O, et al. Comparison of local infiltration analgesia to bupivacaine wound infiltration as part of a multimodal pain program in total hip replacement. J Surg Orthop Adv 2015;24:235–41. [PubMed] [Google Scholar]
- [18].Lee KJ, Min BW, Bae KC, et al. Efficacy of multimodal pain control protocol in the setting of total hip arthroplasty. Clin Orthop Surg 2009;1:155–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Maheshwari AV, Blum YC, Shekhar L, et al. Multimodal pain management after total hip and knee arthroplasty at the Ranawat Orthopaedic Center. Clin Orthop Relat Res 2009;467:1418–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Hamilton TW, Athanassoglou V, Trivella M, et al. Liposomal bupivacaine peripheral nerve block for the management of postoperative pain. Cochrane Database Syst Rev 2016;8:CD011476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Meneghini RM, Bagsby D, Ireland PH, et al. Liposomal bupivacaine injection technique in total knee arthroplasty. J Knee Surg 2017;30:88–96. [DOI] [PubMed] [Google Scholar]
- [22].Kuang MJ, Du Y, Ma JX, et al. The efficacy of liposomal bupivacaine using periarticular injection in total knee arthroplasty: a systematic review and meta-analysis. J Arthroplasty 2017;32:1395–402. [DOI] [PubMed] [Google Scholar]
- [23].Liu SQ, Chen X, Yu CC, et al. Comparison of periarticular anesthesia with liposomal bupivacaine with femoral nerve block for pain control after total knee arthroplasty: a PRISMA-compliant meta-analysis. Medicine 2017;96:e6462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Hida T, Yukawa Y, Ito K, et al. Intrathecal morphine for postoperative pain control after laminoplasty in patients with cervical spondylotic myelopathy. J Orthopaedic Sci 2016;21:425–30. [DOI] [PubMed] [Google Scholar]
- [25].Kunopart M, Chanthong P, Thongpolswat N, et al. Effects of single shot femoral nerve block combined with intrathecal morphine for postoperative analgesia: a randomized, controlled, dose-ranging study after total knee arthroplasty. J Med Assoc Thai 2014;97:195–202. [PubMed] [Google Scholar]


