Abstract
Rationale:
Thoracic-lumbar vertebral fracture is very common in clinic, and late post-traumatic kyphosis is the main cause closely related to the patients’ life quality, which has evocated extensive concern for the surgical treatment of the disease. This study aimed to analyze the clinical outcomes and surgical strategies for late post-traumatic kyphosis after failed thoracolumbar fracture operation.
Patient concerns:
All patients presented back pain with kyphotic apex vertebrae between T12 and L3. According to Frankel classification grading system, among them, 3 patients were classified as grade D, with the ability to live independently.
Diagnoses:
A systematic review of 12 case series of post-traumatic kyphosis after failed thoracolumbar fracture operation was involved.
Interventions:
Wedge osteotomy was performed as indicated—posterior closing osteotomy correction in 5 patients and anterior open-posterior close correction in 7 patients.Postoperatively, thoracolumbar x-rays were obtained to evaluate the correction of kyphotic deformity, visual analog scales (VAS) and Frankel grading system were used for access the clinical outcomes.
Outcomes:
All the patients were followed up, with the average period of 38.5 months (range 24–56 months). The Kyphotic Cobb angle was improved from preoperative (28.65 ± 11.41) to postoperative (1.14 ± 2.79), with the correction rate of 96.02%. There was 1 case of intraoperative dural tear, without complications such as death, neurological injury, and wound infection. According to Frankel grading system, no patient suffered deteriorated neurological symptoms after surgery, and 2 patients (2/3) experienced significant relief after surgery. The main VAS score of back pain was improved from preoperative (4.41 ± 1.08) to postoperative (1.5 ± 0.91) at final follow-up, with an improvement rate of 65.89%.
Lessons:
Surgical treatment of late post-traumatic kyphosis after failed thoracolumbar fracture operation can obtain good radiologic and clinical outcomes by kyphosis correction, decompression, and posterior stability.
Keywords: kyphosis, late, post-traumatic, thoracolumbar fracture, wedge osteotomy
1. Introduction
Spine fractures usually occur at the site of thoracolumbar junction. Primary treatment is very important for the disease, otherwise kyphosis will be developed, leading to low back pain, spinal stenosis, spinal cord injury, and so on. If these complications appeared, a revision surgery is necessary. During the past decades, kinds of treatment methods emerged for the treatment of late post-traumatic kyphosis after failed thoracolumbar fracture, mainly divided into 3 categories—anterior, posterior, and combined anterior and posterior operation.[1–4]
The causes of failed old thoracolumbar fractures are usually classified into 2 categories: (1) posterior insufficient reduction of the compressed vertebral body; and (2) excessive distraction reduction of the fractured vertebral. In addition, surgeons pay much attention to reduction and fixation of the fractured vertebral bodies, but neglect the treatment of intervertebral disc injury. No wonder which 1 reason involved, the disease would progress to late post-traumatic kyphosis. When the patient's kyphotic angle is less than 20°, without obvious pain and neurological symptoms, conservative treatment is suggested; when the patient's kyphotic angle is more than 20°, and combined with delayed pain and progressive nerve damage, operative treatment is recommended.
This study retrospectively analyzed a series of cases with late post-traumatic kyphosis after failed thoracolumbar fracture operation, aiming to evaluate the surgical strategies and clinical outcomes.
2. Patients and methods
2.1. Case series
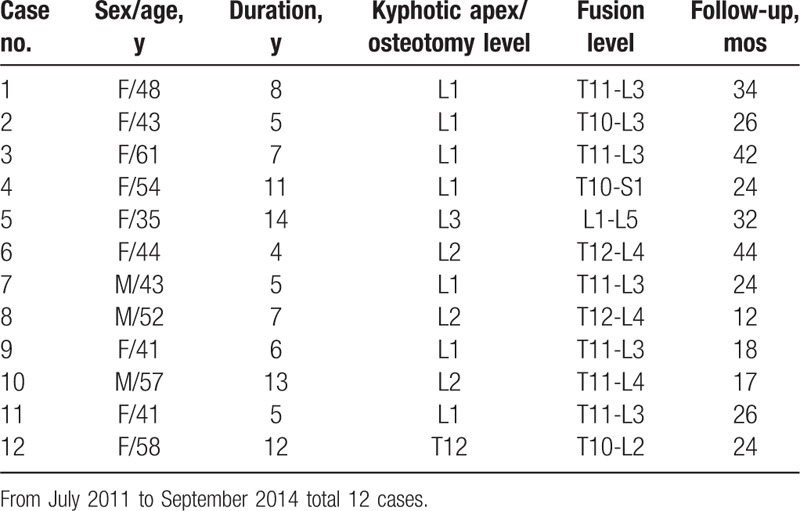
From July 2011 to September 2014, in all, 12 patients with post-traumatic kyphosis after failed thoracolumbar fracture operation were involved. There were 9 men and 3 women, with an average of 48.1 years (range 41–61years). The mean duration from the primary surgery to the revision surgery was 8.1 years (range 5–14 years). All patients had kyphotic apex vertebrae between T12 and L3 (T12 in 1 case, T1 in 7 cases, L2 in 3 cases, and L3 in 1 case; Table 1). In these cases, all the patients presented with back pain, and 4 of them accompanied by neurological deficit, such as numbness and weakness of the lower extremities. The primary operations were posterior operations, included internal fixation of spinous process in 1 case, simple reduction and pedicle screw fixation in 3 cases, pedicle screw internal fixation combined with vertebral lamina bone graft in 4 cases, decompression, reduction, pedicle screw internal fixation, and bone grafting fusion in 4 cases. The first appearance of the symptoms dated from 6 to 32 months, with the average period of 14.2 months. According to Frankel classification grading system, 9 patients had normal lower extremity function (E), and the other 3 patients were classified as grade D, with the ability to live independently.
Table 1.
Demographic data.
2.2. Surgical technique
All the patients received general anesthesia. After anesthesia, the patient was placed prone on the operating table. Then the operative segments were confirmed under intraoperative C-arm fluoroscopy (2 or 3 levels above/below osteotomy site), and a midline incision was made. The spine was exposed, and bilateral pedicle screws were placed on the 2 caudal and 2 cranial vertebrae using the free-hand technique. Then wedge osteotomy was performed—5 of them were performed by posterior closing osteotomy correction and 7 were performed by anterior open-posterior close correction. Before closing osteotomy surface, posterior and bilateral wall of the vertebral body must be removed to avoid damage the spinal cord. Then, spinal canal hidden decompression was done at the upper and lower margins of the vertebra, without residual pedicle cortex around the nerve roots. After extensive posterior decompression, the correction of the kyphosis was performed by in situ bending technique and assessed during operation. Next, the bended rods were fixed onto the pedicle screws and reinforced with a cross-link. The osteotomy gap between the osteotomized vertebra and upper vertebra was filled with autologous bone graft to obtain a bone-on-bone contact. Additionally, posterolateral fusion was also obtained by the graft of remaining bone chips. Finally, a nerve hook was routinely used to check the space around nerve roots, and the wound was closed with a suction drain.
2.3. Postoperation
Patients were encouraged to mobilize on third postoperative day with a customized thoracolumbar orthosis for 3 months.
2.4. Radiological assessments and clinical evaluation
The thoracolumbar x-rays were obtained for the patients postoperatively and at the regular follow-up. Radiological outcomes were assessed on the basis of standing anteroposterior (AP) and lateral x-rays. Also, Cobb angle was measured to revaluate the correction of kyphotic deformity. Cobb correction rate = (preoperative cobb − posterior cobb)/preoperative cobb × 100%.
Clinical outcome was accessed using the Frankel grading system for neurological status and visual analog scale (VAS) for back pain preoperatively and at the final follow-up. In addition, operative time, blood loss, functional improvement, and intraoperative and postoperative complications were recorded.
2.5. Statistical analysis
Preoperative and postoperative changes in kyphotic Cobb angles and lumbar lordosis angles were tested using the paired t test. All data were presented as the mean ± SEM. All statistical analyses were conducted with GraphPad Prism 5. Statistical differences were considered significant for a P value less than .05.
2.6. Ethics statement
This study was conducted in accordance with the Declaration of Helsinki and received approval from the Ethics Committee of our hospital.
3. Results
3.1. Summary of cases
The mean operative time was 188 minutes (range from 168 to 242 minutes), with a mean intraoperative blood loss of 824.5 mL (range from 520 to 1260 mL). Wound drainage lasted for a mean for 4.4 days (3–7), and the mean postoperative drainage volume was 422 mL (range from 310 to 840 mL). There were no complications such as death, neurological injury, and wound infection. Intraoperative dural tear occurred in 1 case, who experienced spinal fluid leak for nearly 2 weeks and then got controlled without further operative intervention.
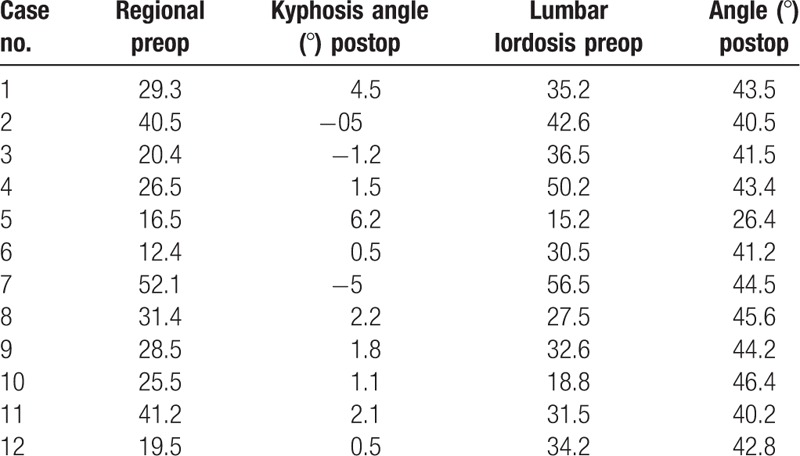
All the patients were followed up, with the average period of 38.5 months (range 24–56 months). The mean preoperative kyphotic Cobb angle was (28.65 ± 11.41) and the mean posterior Cobb angle was (1.14 ± 2.79), with the correction rate of 96.02%. No obvious loss of correction was found during the follow-up. The average lumbar lordosis angle was changed from (34.27 ± 11.66) degrees preoperatively to (41.68 ± 5.19) after operation (Table 2).
Table 2.
Radiological outcome in the 12 patients.
No patient suffered deteriorated neurological symptoms after surgery. The 3 patients with neurological symptoms of the lower extremities experienced various degrees of relief after surgery. Among them, 1 patient of D improved to E postoperatively, according to the Frankel grading system. During the follow-up, 1 of the remaining 2 patients of D improved to E at 6 months postoperatively, and the other remained as grade D at the final follow-up. The main VAS score of back pain was (4.41 ± 1.08) before operation, which improved to (1.5 ± 0.91) at final follow-up, with an improvement rate of 65.89% (typical cases; Figs. 1–3).
Figure 1.
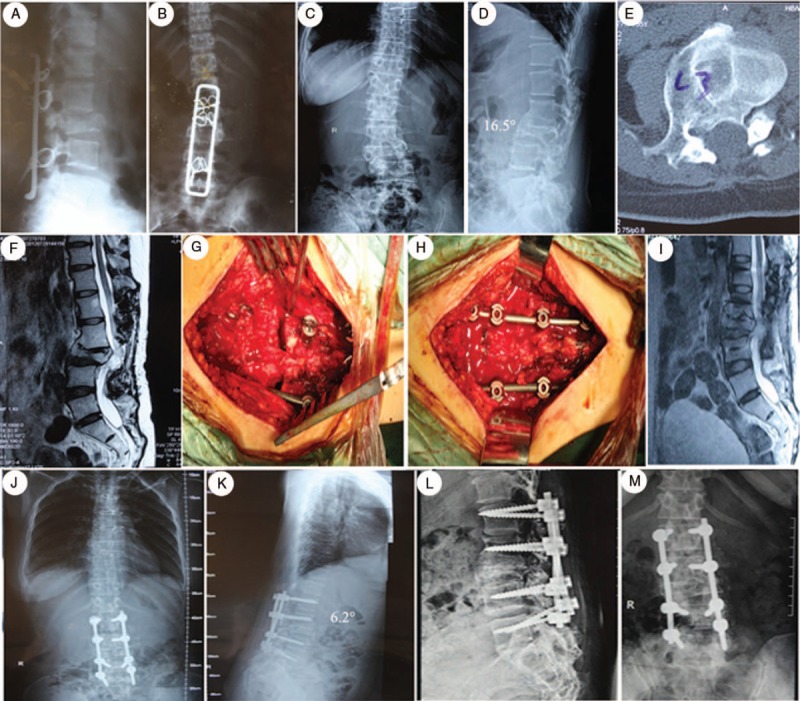
A 35-year-old female who presented with an old L3 fracture and severe back pain. (A, B) She was treated with a posterior fusion and fixation from L1-L5, 14 years ago. (C, D) The preoperative x-rays showed the kyphotic angle was 16.5°, the lumbar lordotic angle was 9.2°. (E, F) Preoperative CT reconstruction and MRI scan showed bony canal stenosis and spinal cord compression. (G–H) Intraoperative pictures showed posterior osteotomy and fixation. (I) Postoperative MRI scan indicated complete decompression of the spinal cord. (J, K) She was treated with a posterior osteotomy and fusion from L1-L5 with L3 pedicle subtraction osteotomy. (L, M) A anteroposterior (AP) and lateral x-ray taken half a year after posterior fusion showed restoration of sagittal alignment without hardware loosening or loss of correction. CT = computed tomography, MRI = magnetic resonance imaging.
Figure 3.
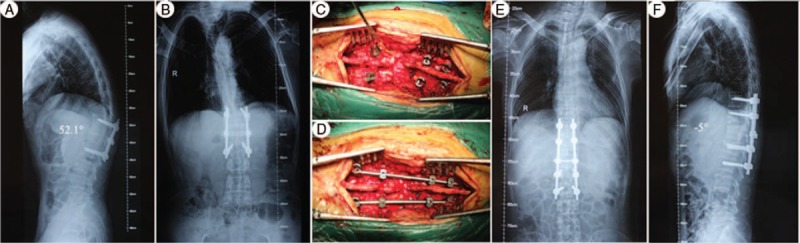
A 43-year-old male with L1 fracture, who underwent posterior reduction and fixation operation 2 years previously, presented with progressive low back pain. (A, B) The preoperative x-rays showed adjacent segment degeneration and thoracolumbar kyphosis, with the kyphotic angle 52.1°. (C, D) Intraoperative pictures showed posterior osteotomy and fixation. (E, F) Postoperative x-rays showed posterior osteotomy and fusion from T10-L2.
Figure 2.
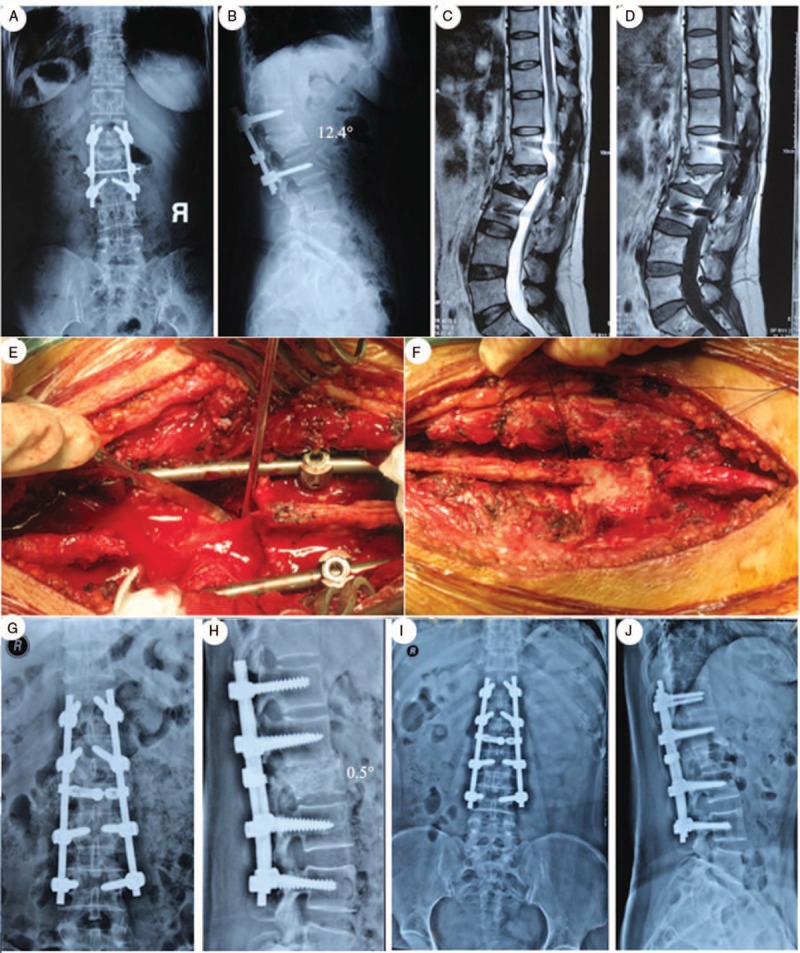
A 44-year-old female with L2 fracture, who underwent posterior reduction and fixation operation 4 years previously, presented with progressive low back pain. (A, B) The preoperative x-rays showed the kyphotic angle was 12.4°, the lumbar lordotic angle was 20.5°. (C, D) Preoperative T1 and T2 MRI scans indicated spinal cord compression at L2. (E) Intraoperative pictures showed posterior osteotomy and fixation. (F) Intraoperative pictures showed autogenous bone graft. (G, H) Postoperative x-rays showed posterior osteotomy and fusion from T12-L4 with L2 pedicle subtraction osteotomy. (I, J) Antero-posterior (AP) and lateral x-rays taken 3 months after posterior fusion showed restoration of sagittal alignment. MRI = magnetic resonance imaging.
4. Discussion
Thoracic-lumbar vertebral fracture is very common in clinic, which easily develops to kyphosis after failed timely and effective treatment. Along with the progress of the disease, severe lower back pain or spinal cord compression symptoms will occur, resulting in functional disability of patients.[5–8] Old thoracolumbar fractures failed in the first operation is not uncommon in clinic, and resulted in late post-traumatic kyphosis and spinal cord injury. Late post-traumatic kyphosis is the main case closely related to the patients’ life quality, which has evocated extensive concern for the surgical treatment of the disease.[9–11] The aim of surgery is to stable injured segments, correct deformity, and restore vertebral canal volume by decompression as much as possible.
4.1. Risk factors for late post-traumatic kyphosis secondary to thoracolumbar fracture
Generally, intervertebral disc injury can deteriorate the development of kyphosis of thoracolumbar fractures, postoperatively. Because injured intervertebral disc easily degenerates and eventually develops kyphosis. A retrospective radiographic follow-up was conducted by Schnee and Ansell,[12] the results of which showed a trend of loss in deformity correction with 10° after posterior surgery of thoracic-lumbar fracture. The possible reasons included disc height loss, and failed correction of injured vertebral and natural course of primary osteoporosis. Leferink et al[13] reported that disc height loss was the main cause contributed to progressive post-traumatic kyphosis of thoracic-lumbar fractures. Shi et al[14] conducted a retrospective study of 52 patients with thoracic-lumbar fractures for 7 years, and found that loss of upper intervertebral disc space of the fractured vertebra was the main cause induced postoperative corrective angle loss, and the loss of lower intervertebral disc space and the height of the vertebral exerted relative small effects.
Due to lack of the original fracture data, it is difficult to judge the stability of the primary fractures. On the basis of the 12 involved cases, the below factors were involved: (1) failed internal fixation, such as undeserved technique, overload on the internal fixation, or ineffective posterior brace after surgery; (2) the height of the fractured vertebral body was not restored satisfactorily; (3) the height of intervertebral space was not recovered (post-traumatic kyphosis mainly occurred at the site of the upper and lower intervertebral space, especially the upper intervertebral space); (4) sagittal balance was not handled suitably. Residual kyphosis might be aggravated during follow-up. It is vital to restore the sagittal balance in thoracic lumbar spine fractures.
4.2. Proximal junctional kyphosis
Proximal junctional kyphosis (PJK) is a kind of adjacent segment disease, which usually occurs after correction and internal fixation by spine instrumentation. The imaging characteristics of PJK must meet the following 2 points: (1) PJK angle > 0° after operation; (2) posterior PJK angle increases more than 10°, compared with preoperative PJK angle. In recent years, the occurrence rate of PJK has been gradually increased along with the development of spinal internal fixation technique. Kim et al[15] led a study focused on PJK in patients who had surgery for scoliosis and/or kyphosis, and the results indicated that the incidence of PJK ranged from 17% to 39%. In addition, the study also pointed out the majority seemed to occur at patients of older age within 2 years of primary operation. In a long-term review of minimum 5 years, PJK happened in 16 of 59 patients who underwent posterior surgery, whereas only 1 case of PJK happened in 16 patients who underwent anterior surgery; thus the results indicated that posterior surgery was a risk factor of PJK.[16] Another study led by Kim et al showed the prevalence of PJK was 39% at 7.8 years postoperation, which progressed significantly within 8 weeks postoperation (59%). Also, the combination of anterior and posterior spinal fusion surgery was considered as a risk factor.[17] Watanabe et al[18] confirmed that combined operation was a risk factor of PJK. Recently, Wang et al[19] found that the upper instrumentation vertebrae (UIV) at thoracolumbar junction was a risk factor for the development of PJK in degenerative lumbar scoliosis patients. The development of PJK deformity resulted from multiple factors, such as spine biomechanics, imaging parameters, clinical characteristics, and so on. Combined anterior and posterior surgery, and posterior surgery can be considered as independent risk factor for PJK.
4.3. Posterior correction strategies and clinical evaluation
Osteotomy is an effective method for the treatment of thoracolumbar deformity. Usually, 3 main approaches are widely practiced—anterior, posterior, and a combination of anterior and posterior approach. A single anterior approach is beneficial for nerve decompression, but with poor corrective effects, whereas a combination of anterior and posterior approach is effective of correction\, but with the disadvantages of severer injuries and higher complication rates. Because of good nerve decompression and deformity correction, posterior osteotomy is commonly recommended for the treatment of post-traumatic kyphosis after failed thoracolumbar fracture, including Smith Petersen osteotomy (SPO), pedicle subtraction osteotomy (PSO), posterior vertebral column resection (PVCR), and so on.[3,20,21]
Smith Petersen osteotomy was first applied for the treatment of kyphotic deformities by resecting the posterior elements of the vertebra in 1945.[22] One single level of SPO is expected to obtain 10° to 15° correction.[23–25] Simple SPO is difficult to achieve satisfactory outcomes for the sharp kyphosis of thoracic lumbar spine. PSO was first described by Thomasen,[26] which is a technique of transpedicular cortical decancellation osteotomy. Compared with SPO, PSO is technical demand, with the advantages of greater correction at sagittal and coronal plane.[27–29] PSO is the main surgical method for the treatment of this kind of kyphosis, with the average correction of 30 to 35 of a single-level PSO.[30–32] PVCR has the characteristics of severer injury, higher risk, and better corrective effect, which is mainly used for severe congenital deformity and deformity after pathological fracture. Recently, modified wedge closing osteotomy has been introduced in the treatment of post-traumatic kyphosis with less complications, satisfactory correction, and good fusion rate.[33–35]
5. Conclusions
In this study, posterior closing osteotomy and anterior open-posterior close osteotomy were performed. Preoperatively, all the patients had back pain with or without neurological symptoms of the lower extremities. After surgery, back pain was significantly ameliorated with an improvement rate of 65.89%. Kyphosis correction not only improved Cobb angle with the correction rate of 96.02% directively, but also benefited the improvement of neurological functions. Therefore, posterior wedge osteotomy is an effective surgical strategy to treat late post-traumatic kyphosis after failed thoracolumbar fracture operation by kyphosis correction, decompression, and posterior stability.
Footnotes
Abbreviations: PJK = proximal junctional kyphosis, PSO = pedicle subtraction osteotomy, PVCR = posterior vertebral column resection, SPO = Smith Petersen osteotomy, VAS = visual analog scale.
SL and ZL contributed equally to this work.
Funding: This study was supported by grants from the financial support of the National Science Foundation of China (NSFC, 81201393;2013YGYL015;02.03.2017–45).
The authors report no conflicts of interest.
References
- [1].Wood KB, Bohn D, Mehbod A. Anterior versus posterior treatment of stable thoracolumbar burst fractures without neurologic deficit: a prospective, randomized study. J Spinal Disord Tech 2005;18(suppl):S15–23. [DOI] [PubMed] [Google Scholar]
- [2].Brayda-Bruno M, Luca A, Lovi A, et al. Post-traumatic high thoracic angular kyphosis: posterior approach with correction and fusion in two steps. Eur Spine J 2012;21:2724–2726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Lazennec JY, Neves N, Rousseau MA, et al. Wedge osteotomy for treating post-traumatic kyphosis at thoracolumbar and lumbar levels. J Spinal Disord Tech 2006;19:487–94. [DOI] [PubMed] [Google Scholar]
- [4].Munting E. Surgical treatment of post-traumatic kyphosis in the thoracolumbar spine: indications and technical aspects. Eur Spine J 2010; 19suppl 1:S69–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Been HD, Poolman RW, Ubags LH. Clinical outcome and radiographic results after surgical treatment of post-traumatic thoracolumbar kyphosis following simple type A fractures. Eur Spine J 2004;13:101–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Chou D, Wang VY, Storm PB. Pedicle subtraction osteotomies for the correction of post-traumatic thoracolumbar kyphosis. J Clin Neurosci 2010;17:113–117. [DOI] [PubMed] [Google Scholar]
- [7].Li X, Zhang J, Tang H, et al. Closing-opening wedge osteotomy for thoracolumbar traumatic kyphosis. Eur J Med Res 2014;19:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Whitesides TE., Jr Traumatic kyphosis of the thoracolumbar spine. Clin Orthop Relat Res 1977;78–92. [PubMed] [Google Scholar]
- [9].Andress HJ, Braun H, Helmberger T, et al. Long-term results after posterior fixation of thoraco-lumbar burst fractures. Injury 2002;33:357–65. [DOI] [PubMed] [Google Scholar]
- [10].Martiniani M, Vanacore F, Meco L, et al. Is posterior fixation alone effective to prevent the late kyphosis after T-L fracture? Eur Spine J 2013;22suppl 6:S951–956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Hrabalek L, Houdek M, Vaverka M. [Contribution of MRI to the thoracolumbar spine injuries diagnostics and therapy]. Rozhl Chir 2009;88:461–5. [PubMed] [Google Scholar]
- [12].Schnee CL, Ansell LV. Selection criteria and outcome of operative approaches for thoracolumbar burst fractures with and without neurological deficit. J Neurosurg 1997;86:48–55. [DOI] [PubMed] [Google Scholar]
- [13].Leferink VJ, Zimmerman KW, Veldhuis EF, et al. Thoracolumbar spinal fractures: radiological results of transpedicular fixation combined with transpedicular cancellous bone graft and posterior fusion in 183 patients. Eur Spine J 2001;10:517–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Shi J, Mei X, Liu J, et al. The influence of correction loss in thoracolumbar fractures treated by posterior instrumentation: a minimum 7-year follow-up. J Clin Neurosci 2011;18:500–503. [DOI] [PubMed] [Google Scholar]
- [15].Kim HJ, Lenke LG, Shaffrey CI, et al. Proximal junctional kyphosis as a distinct form of adjacent segment pathology after spinal deformity surgery: a systematic review. Spine (Phila Pa 1976) 2012;3722 suppl:S144–164. [DOI] [PubMed] [Google Scholar]
- [16].Yagi M, King AB, Boachie-Adjei O. Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine (Phila Pa 1976) 2012;37:1479–1489. [DOI] [PubMed] [Google Scholar]
- [17].Kim YJ, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976) 2008;33:2179–84. [DOI] [PubMed] [Google Scholar]
- [18].Watanabe K, Uno K, Suzuki T, et al. Risk factors for proximal junctional kyphosis associated with dual-rod growing-rod surgery for early-onset scoliosis. Clin Spine Surg 2016;29:E428–433. [DOI] [PubMed] [Google Scholar]
- [19].Wang H, Ma L, Yang D, et al. Incidence and risk factors for the progression of proximal junctional kyphosis in degenerative lumbar scoliosis following long instrumented posterior spinal fusion. Medicine (Baltimore) 2016;95:e4443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Wu SS, Hwa SY, Lin LC, et al. Management of rigid post-traumatic kyphosis. Spine (Phila Pa 1976) 1996;21:2260–2266.[discussion 2267]. [DOI] [PubMed] [Google Scholar]
- [21].Lehmer SM, Keppler L, Biscup RS, et al. Posterior transvertebral osteotomy for adult thoracolumbar kyphosis. Spine (Phila Pa 1976) 1994;19:2060–7. [DOI] [PubMed] [Google Scholar]
- [22].Smith-Petersen MN, Larson CB, Aufranc OE. Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. Clin Orthop Relat Res 1969;66:6–9. [PubMed] [Google Scholar]
- [23].Kostuik JP, Maurais GR, Richardson WJ, et al. Combined single stage anterior and posterior osteotomy for correction of iatrogenic lumbar kyphosis. Spine (Phila Pa 1976) 1988;13:257–66. [DOI] [PubMed] [Google Scholar]
- [24].McMaster MJ. A technique for lumbar spinal osteotomy in ankylosing spondylitis. J Bone Joint Surg Br 1985;67:204–10. [DOI] [PubMed] [Google Scholar]
- [25].La Grone MO. Loss of lumbar lordosis. A complication of spinal fusion for scoliosis. Orthop Clin North Am 1988;19:383–93. [PubMed] [Google Scholar]
- [26].Thomasen E. Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop Relat Res 1985;142–52. [PubMed] [Google Scholar]
- [27].Bridwell KH, Lewis SJ, Rinella A, et al. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. Surgical technique. J Bone Joint Surg Am 2004;86-A(suppl 1):44–50. [DOI] [PubMed] [Google Scholar]
- [28].Bridwell KH, Lewis SJ, Lenke LG, et al. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. J Bone Joint Surg Am 2003;85-A:454–63. [DOI] [PubMed] [Google Scholar]
- [29].Potter BK, Lenke LG, Kuklo TR. Prevention and management of iatrogenic flatback deformity. J Bone Joint Surg Am 2004;86-A:1793–808. [DOI] [PubMed] [Google Scholar]
- [30].Ahn UM, Ahn NU, Buchowski JM, et al. Functional outcome and radiographic correction after spinal osteotomy. Spine (Phila Pa 1976) 2002;27:1303–11. [DOI] [PubMed] [Google Scholar]
- [31].van Royen BJ, Slot GH. Closing-wedge posterior osteotomy for ankylosing spondylitis. Partial corporectomy and transpedicular fixation in 22 cases. J Bone Joint Surg Br 1995;77:117–21. [PubMed] [Google Scholar]
- [32].Berven SH, Deviren V, Smith JA, et al. Management of fixed sagittal plane deformity: results of the transpedicular wedge resection osteotomy. Spine (Phila Pa 1976) 2001;26:2036–43. [DOI] [PubMed] [Google Scholar]
- [33].Jo DJ, Kim YS, Kim SM, et al. Clinical and radiological outcomes of modified posterior closing wedge osteotomy for the treatment of posttraumatic thoracolumbar kyphosis. J Neurosurg Spine 2015; 23:510–517. [DOI] [PubMed] [Google Scholar]
- [34].Zhang X, Zhang Y, Wang Z, et al. Modified posterior closing wedge osteotomy for the treatment of posttraumatic thoracolumbar kyphosis. J Trauma 2011; 71:209–216. [DOI] [PubMed] [Google Scholar]
- [35].Bourghli A, Boissiere L, Vital JM, et al. Modified closing-opening wedge osteotomy for the treatment of sagittal malalignment in thoracolumbar fractures malunion. Spine J 2015;15:2574–2582. [DOI] [PubMed] [Google Scholar]


