Supplemental Digital Content is available in the text
Keywords: Chinese herbal, meta-analysis, post stroke, stroke recovery
Abstract
Background:
Stroke is a condition with high morbidity and mortality, and 75% of stroke survivors lose their ability to work. Stroke is a burden to the family and society. The purpose of this study was to evaluate the effectiveness of Chinese herbal patent medicines in the treatment of patients after the acute phase of a stroke.
Methods:
We searched the following databases through August 2016: PubMed, Embase, Cochrane library, China Knowledge Resource Integrated Database (CNKI), China Science Periodical Database (CSPD), and China Biology Medicine disc (CBMdisc) for studies that evaluated Chinese herbal patent medicines for post stroke recovery. A random-effect model was used to pool therapeutic effects of Chinese herbal patent medicines on stroke recovery. Network meta-analysis was used to rank the treatment for each Chinese herbal patent medicine.
Results:
In our meta-analysis, we evaluated 28 trials that included 2780 patients. Chinese herbal patent medicines were effective in promoting recovery after stroke (OR, 3.03; 95% CI: 2.53–3.64; P < .001). Chinese herbal patent medicines significantly improved neurological function defect scores when compared with the controls (standard mean difference [SMD], −0.89; 95% CI, −1.44 to −0.35; P = .001). Chinese herbal patent medicines significantly improved the Barthel index (SMD, 0.73; 95% CI, 0.53–0.94; P < .001) and the Fugl–Meyer assessment scores (SMD, 0.60; 95% CI, 0.34–0.86; P < .001). In the network analysis, MLC601, Shuxuetong, and BuchangNaoxintong were most likely to improve stroke recovery in patients without acupuncture. Additionally, Mailuoning, Xuesaitong, BuchangNaoxintong were the patented Chinese herbal medicines most likely to improve stroke recovery when combined with acupuncture.
Conclusions:
Our research suggests that the Chinese herbal patent medicines were effective for stroke recovery. The most effective treatments for stroke recovery were MLC601, Shuxuetong, and BuchangNaoxintong. However, to clarify the specific effective ingredients of Chinese herbal medicines, a well-designed study is warranted.
1. Introduction
Worldwide, ischemic stroke is the second largest cause of death, and stroke from all causes has high morbidity and mortality.[1]Annually, 15 million people suffer a stroke.[2] In China, there are 2.5 million new stroke cases each year and 7.5 million stroke survivors.[3] Survivors may be affected by complications, including vascular dementia and hemiplegia.
The stroke recovery period occurs after the acute stroke period. Although mortality is low during the recovery period, there are serious functional neural defects and a high rate of stroke recurrence. Seventy-five percent of stroke survivors are unable to work.[4] The recurrence rate, 90 days after the stroke, is 7.4%, and the incidence rate of transient ischemic attacks is 17.3%.[5,6] Stroke is a burden for the family and society.
Traditional Chinese Medicine (TCM) has been historically used for stroke treatment, and is widely used today.[7] Chinese herbal medicine is an important component of TCM, which has several characteristics, including natural medicine, complex composition, and multifunction.
Chinese herbal medicines for stroke treatment are generally a mixture of different plant and animal extracts.[8] Different herbal medicines have anti-inflammatory or antioxidant properties, cause vasodilation, increase cerebral blood flow velocity, inhibit platelet aggregation, protect against reperfusion injury, and increase tissue tolerance to hypoxia.[9]
The role of herbal drug treatment for stroke recovery has been investigated. For example, YinxingDamo injection (including Ginkgo extract) was proposed to increase cerebral collateral circulation and capillary networks, while decreasing edema, intracranial pressure, and hypoxia-induced nerve cell injury.[10,11] In areas of cerebral ischemia, Tongxinluo capsules (including, extract of ginseng and hirudo) may protect nerve cells by increasing the expression of brain-derived neurotrophic factors.[12,13] Danhong injection (including Salvia miltiorrhiza and Carthamustinctorius) may upregulate the expression of growth-associated protein 43, promote axonal regeneration, and accelerate neural functional recovery.[14,15]
Although Chinese herbal medicine is widely used in stroke recovery in Southeast Asia and Chinese-speaking regions, the evidence of its efficacy remains insufficient. Additionally, there are various types and combinations of Chinese drugs on the market, and it is difficult to compare their therapeutic effects in clinical studies.
Although there have been systematic reviews of TCM treatments for stroke recovery in Chinese journals, the studies showed contradictory results.[16–18] A recent systematic review analyzed the effect of NeuroAiD (MLC601) treatment in stroke recovery and indicated that MLC601 has limited therapeutic effect on neural functional recovery when compared with placebo.[19] We analyzed the use of Chinese patent herbal medicines for stroke recovery. We used traditional and network meta-analysis to analyze the effect of Chinese herbal medicines on poststroke assessment outcomes.
2. Methods
This meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews (PRISMA) guidelines.[20]
2.1. Search strategy
We systematically searched, through August 2016, the following databases: PubMed, Embase, Cochrane Central Register of Controlled Trials, China Knowledge Resource Integrated Database (CNKI), China Science Periodical Database (CSPD), and China Biology Medicine disc (CBMdisc). Keywords used in the search including “post stroke,” “stroke recovery,” “convalescence,” “Chinese herbal medicine,” and “random.” The details of the search strategy in PubMed are presented in Supplemental 1. The search was limited to studies published in English or Chinese. To identify additional eligible studies, we also manually searched reference lists from relevant original and review articles.
2.2. Data selection, data extraction, and quality assessment
Two authors independently searched the literature and selected relevant studies. Inconsistencies were resolved by group discussion. Eligible studies met the following inclusion criteria: patients with a stroke were evaluated during recovery and convalescence; randomized controlled trial; investigated poststroke neurological function and ability to participate in activities of daily living, but not complications; the intervention group was treated with Chinese herbal patent medicines, while the control group did not receive Chinese herbal patent medicines; and the outcome assessments included neurological function and the ability to engage in activities of daily living. Additionally, we excluded letters, editorials, reviews, conference papers, nonhuman studies, and academic dissertations that had not been peer-reviewed.
The following items were extracted from the articles: first author, publication year, sample size, average age, sex ratio, type of stroke, duration of stroke onset, interventions, control, duration of therapy, and follow-up. We assessed the methodological quality of the trials using the risk of bias approach according to the Cochrane Collaboration.[21] The data extraction and quality assessment were conducted independently by 2 authors. In case of disagreement, an additional author examined the original article and made an independent assessment.
The primary outcome of our analyses was the number of patients showing significant improvement, as assessed by widely used stroke recovery criteria, or the number of patients able to resume self-care. The secondary outcomes were neurological function and the ability to engage in activities of daily living, as assessed by the neurological functional defect scores (NDS), Barthel index (BI), Fugl–Meyer assessment (FMA), and functional independence measure (FIM). The major purpose of this study was to determine the effect of Chinese medicine on poststroke recovery of neurological function. We did not evaluate poststroke sequelae, including poststroke depression and epilepsy.
2.3. Statistical analysis
We performed a pairwise meta-analysis using a random-effects model.[22] For dichotomous outcomes, odds ratios (ORs), with 95% confidence intervals (CIs), were calculated to determine the effect size. For continuous data, the standard mean difference (SMDs) and 95% CIs were calculated. The I2 statistic was used to assess heterogeneity across multiple studies. In the absence of statistical heterogeneity (<50%), we used a fixed-effect model, in the presence of heterogeneity we used a random-effects model. We used subgroup analysis to explore heterogeneity according to the drug delivery method and whether Chinese herbal patent medicines were or were not used in combination with acupuncture. Egger test[23] and Begg test[24] were used to evaluate publication bias. The symmetry of a funnel plot was assessed. The trim and fill method was used to correct for publication bias.[25]
A random effects network meta-analysis for mixed multiple treatment comparisons was used to preserve the within-trial randomized treatment comparisons.[26] The network analysis adopted a frequentist framework, and a contrast-based model was used to evaluate multiarm trials. Transitivity was assessed by a network plot, which describes direct and indirect comparisons of any pair of interventions. Inconsistency between direct and indirect sources of evidence was statistically assessed globally (by comparison of the fit and parsimony of consistency and inconsistency models) and locally (by the calculation of the difference between direct and indirect estimates in all closed loops in the network). However, since there are no loops in the network, the network has no degrees of freedom for inconsistency. To rank the treatments for each outcome, we used the surface under the cumulative ranking (SUCRA) probabilities.[27] The comparison-adjusted funnel plots were used to determine whether small-study effects were present in our analyses.[28] All tests were 2-tailed, and a P value of less than .05 was considered statistically significant. Data analyses were performed using STATA software (version 13.0; StataCorp, College Station, TX).
3. Results
We identified 639 articles written in English and 972 written in Chinese. After removing duplicates, 968 articles were identified. After the titles and abstracts were screened, 874 articles were excluded. The full-text of the remaining 94 articles was evaluated, and 66 studies were excluded. Exclusion criteria were: the comparison group included herbal treatment (n = 20); treatment for complications (n = 9); acute stroke treatment (n = 9); use of nonpatented Chinese medicine formulae (n = 8); duplicate publications (n = 7); abstracts (n = 5); no desired outcomes (n = 5); protocols (n = 2); and master's thesis (n = 1). Finally, our systematic review included 28 trials that assessed 2780 patients (Fig. 1, Table 1).[29–56]
Figure 1.
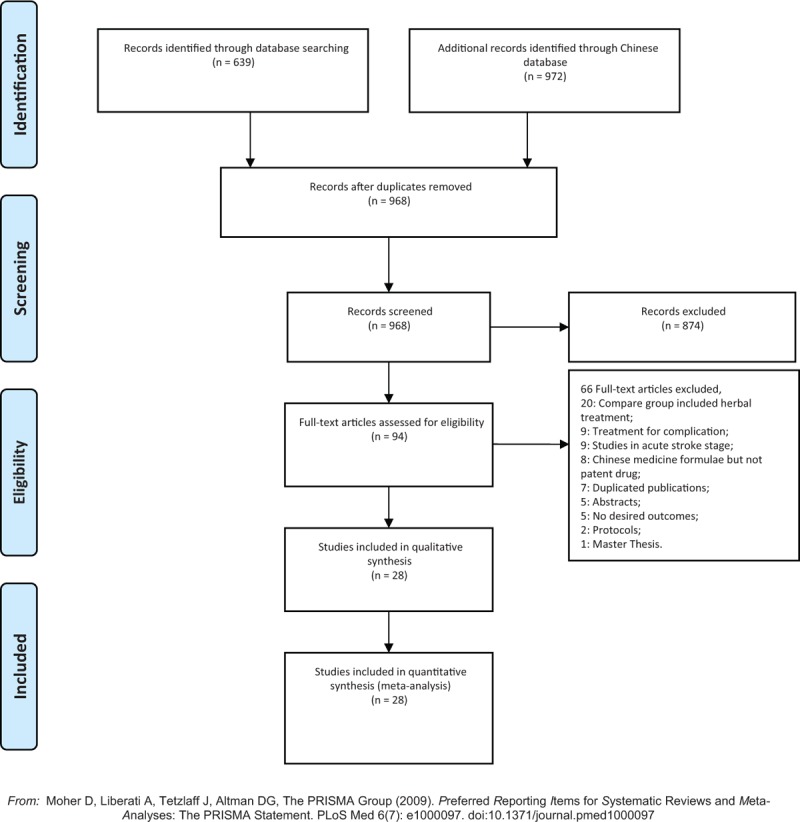
PRISMA flowchart illustrating the selection of studies included in our analyses. PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-analyses.
Table 1.
Characters of included studies.
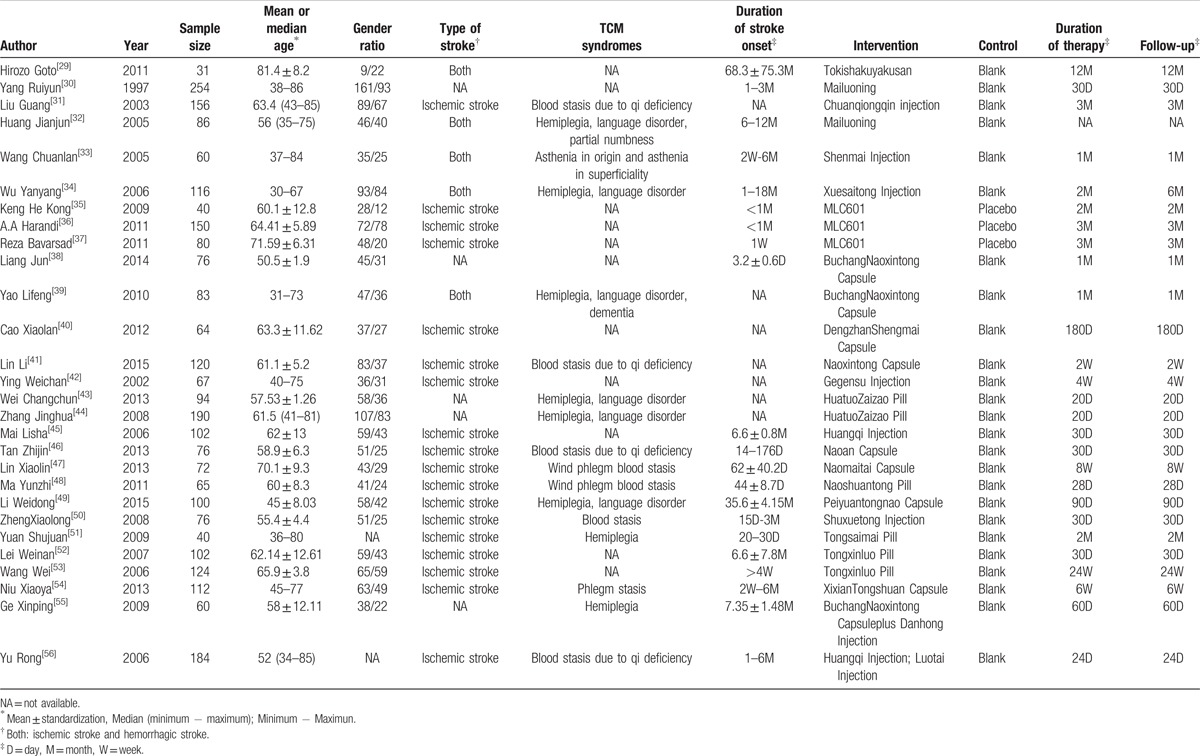
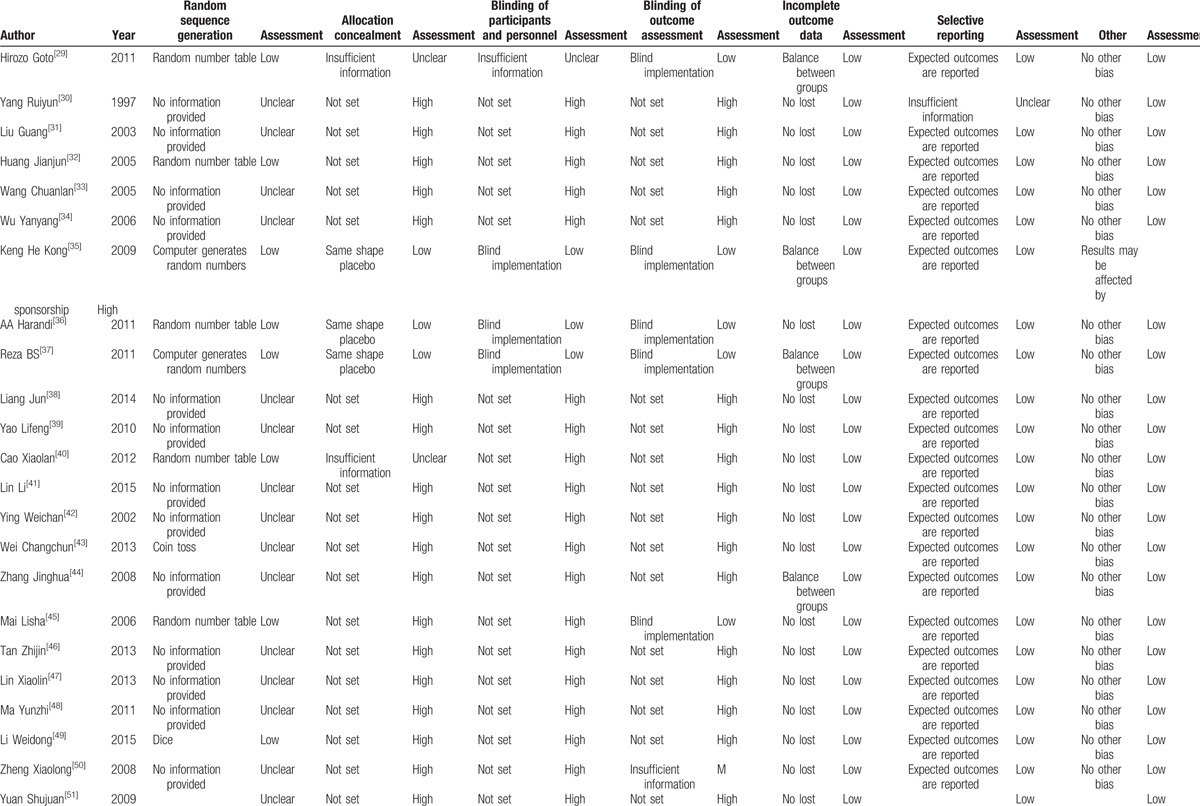
The age of patients ranged from 30 to 90 years. The number of male patients was slightly more than that of female patients. Eighteen studies included patients with ischemic stroke, 5 included patients with either hemorrhagic or ischemic stroke, and 5 did not specify the type of stroke. All studies included patients in the stroke recovery phase; however, 7 did not clearly define the duration of treatment. The shortest intervention and follow-up time was 2 weeks, and the longest was 180 days (Table 1). Although all the studies were randomized controlled trials, 3 were of double-blind design. The overall quality of included studies was not considered ideal, and the details of risk of bias for each trial are shown in Table 2 . In the included studies, 1 received support from Moleac Pte. Ltd and the National Medical Research Council of Singapore.[35] One study received funding from Comprehensive Research on Aging and Health from the Japanese Ministry of Health, Labor, and Welfare.[29] In the other studies the funding source was not disclosed.
Table 2.
Detail of risk of bias for each included study.
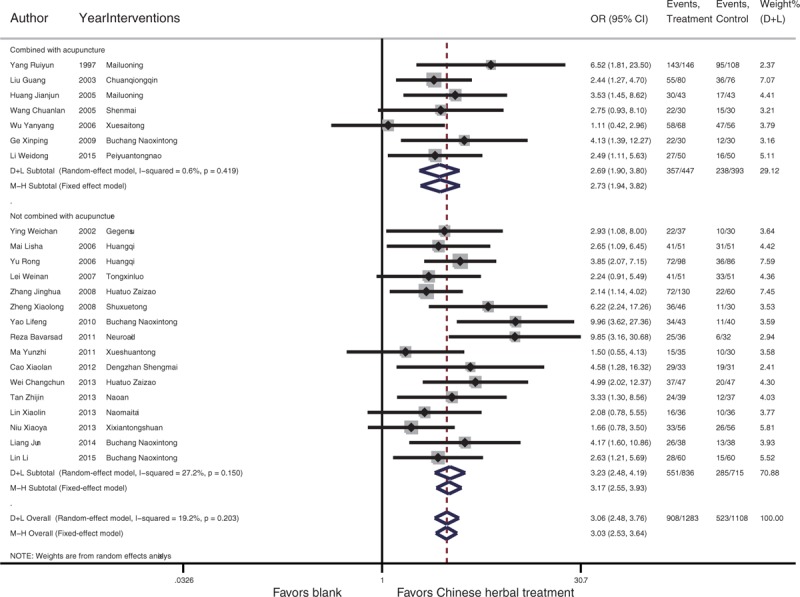
Chinese patent medicines were effective in recovery after stroke (OR, 3.03; 95% CI: 2.53–3.64; P < .001). In the drug-delivery subgroup analysis, oral Chinese medicine improved poststroke recovery (OR, 3.00; 95% CI: 2.37–3.80; P < .001), and intravenous injection of Chinese medicine had similar effects (OR, 3.14; 95% CI, 2.38–4.14; P < .001) (Fig. 2). Chinese herbal medicines combined with acupuncture were more effective than acupuncture alone (OR, 2.73; 95% CI, 1.94–3.82; P < .001), and Chinese herbal medicines when not combined with acupuncture were more effective than control (OR, 3.17; 95% CI, 2.55–3.93; P < .001) (Fig. 3). When assessing recovery of neurological function and the ability to perform activities of daily living, Chinese herbal patent medicines significantly improved the NDS scores when compared with control (SMD, −0.89; 95% CI, −1.44 to −0.35; P = .001). Chinese herbal patent medicines significantly improved scores on the BI (SMD, 0.73; 95% CI, 0.53–0.94; P < .001) and FMA (SMD, 0.6; 95% CI, 0.34–0.86; P < .001). In 1 study included in the analyses, the Chinese Medicine Symptom scores were significantly improved after herbal treatment (SMD, −0.95; 95% CI, −1.33 to −0.57; P < .001). No other significant differences were identified (Fig. 4). Publication biases were identified in the overall effect results (Begg test, P = .035; Egger test, P = .074). After the correction with the trim and fill method, the results of the random effect model were unchanged. Other results did not show significant publication bias (Supplemental 2).
Figure 2.
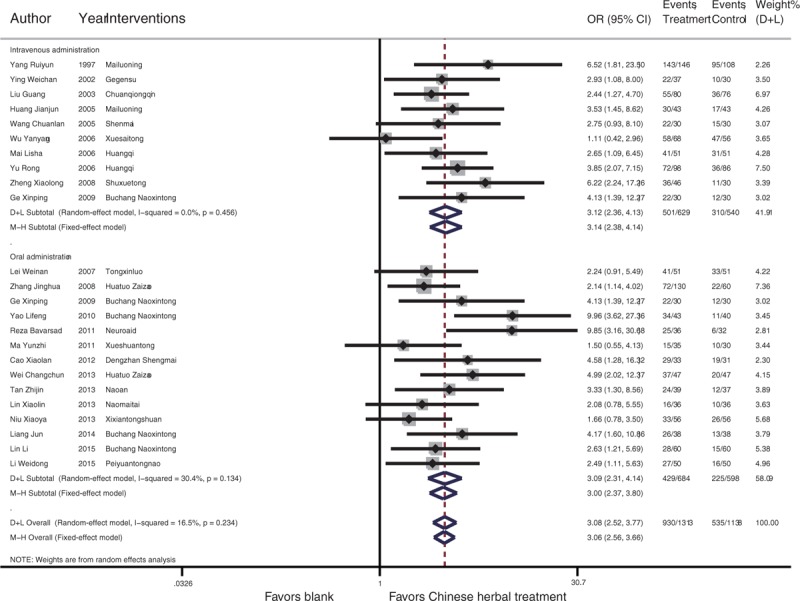
Forest plot of the overall effect of Chinese patent medicines in stroke recovery patients with drug-delivery subgroup analysis.
Figure 3.
Forest plot of the overall effect of Chinese patent medicines in stroke recovery patients with acupuncture subgroup analysis.
Figure 4.
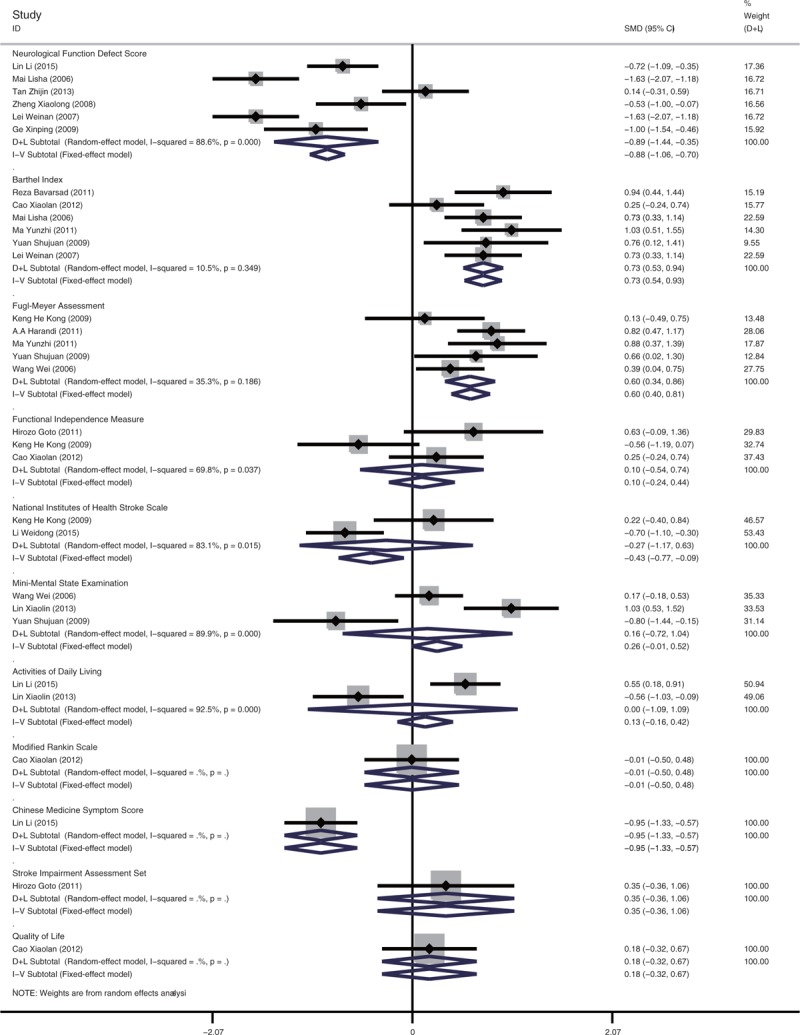
Forest plot of recovery of neurological function and activities of daily life in stroke recovery patients.
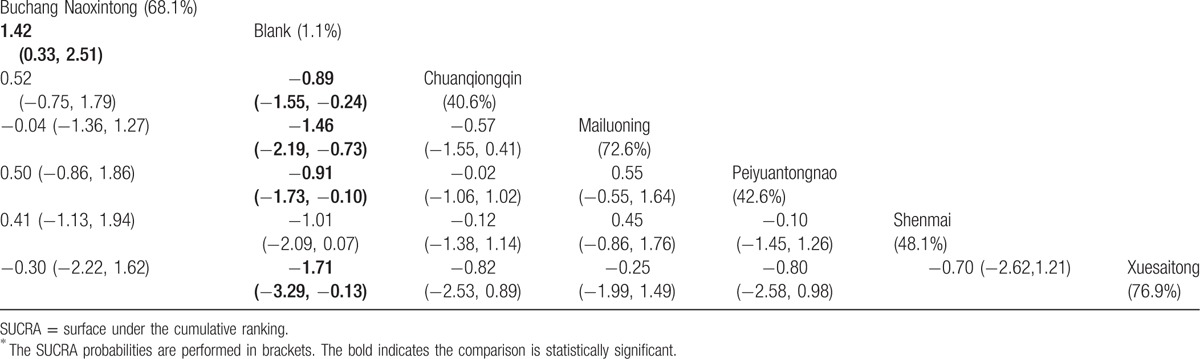
In the network analysis, we compared Chinese herbal medicine plus acupuncture versus acupuncture alone, and Chinese herbal medicine versus placebo control. Comparisons of the therapeutic effectiveness of Chinese herbal patent medicines are shown in Fig. 5. The figure identifies the predominantly pairwise comparisons of different Chinese patent medicines used for stroke recovery. The nodes were weighted according to the number of studies that evaluated each treatment, and the edges were weighted according to the precision of the direct estimate for each pairwise comparison. The comparisons of Chinese herbal medicines without acupuncture and with acupuncture are shown in Tables 3 and 4, respectively. We ranked the comparative effects of all included Chinese patent medicines in stroke recovery with SUCRA probabilities (%). The results indicated that MLC601, Shuxuetong, and BuchangNaoxintong were most likely to improve stroke recovery in patients who did not receive acupuncture (Fig. 6A). In addition, Mailuoning, Xuesaitong, and BuchangNaoxintong were more likely to improve stroke recovery when combined with acupuncture (Fig. 6B). The comparison-adjusted funnel plot used to assess publication bias and determine the presence of small-study effects, did not identify publication bias in the network meta-analysis (Supplemental 2).
Figure 5.
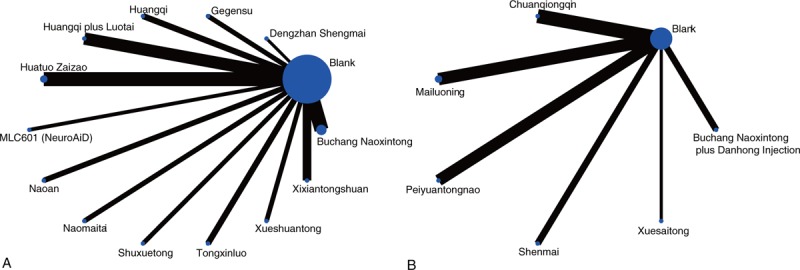
Network of comparisons for overall effect included in the analyses. A, Without acupuncture. B, Combined with acupuncture. The direct comparison between interventions was connected in the network plot, in which nodes are weighted according to the number of studies evaluating each treatment and edges according to the precision of the direct estimate for each pairwise comparison. When a treatment involved more arms, the nodes are larger and the more the edges are weighted, the more accurate the comparison (small standard error).
Table 2 (Continued).
Detail of risk of bias for each included study.
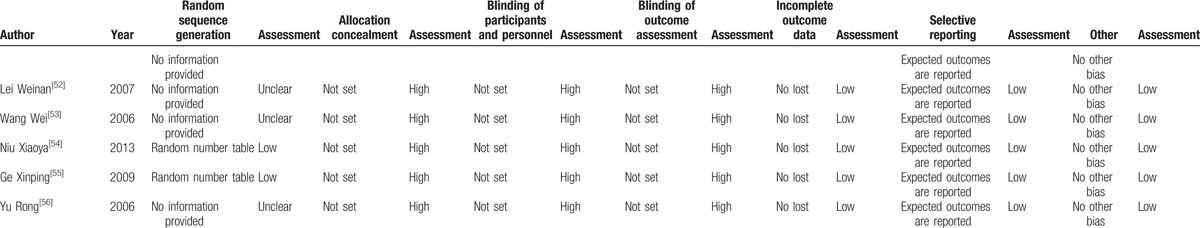
Table 3.
The league table of the consistency model network meta-analysis for the therapeutic effectiveness of Chinese herbal patent medicines without acupuncture on post stroke recovery.
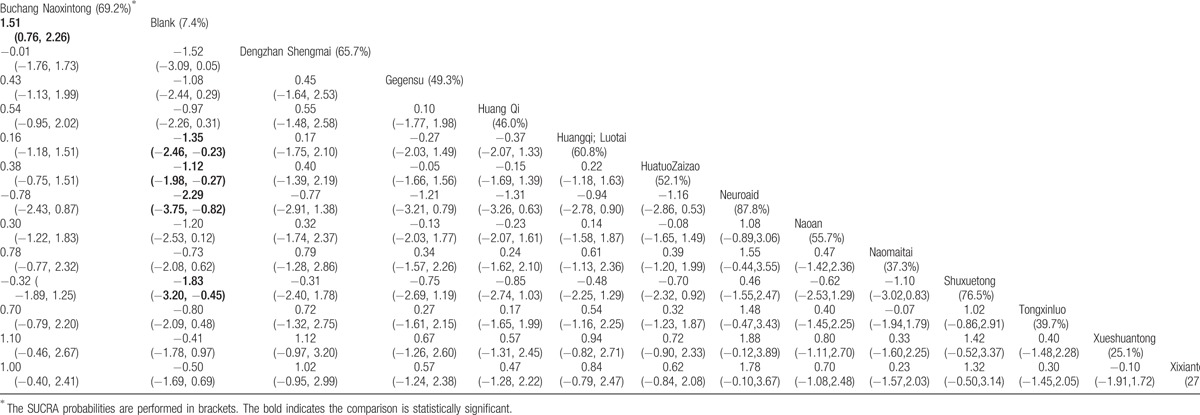
Figure 6.
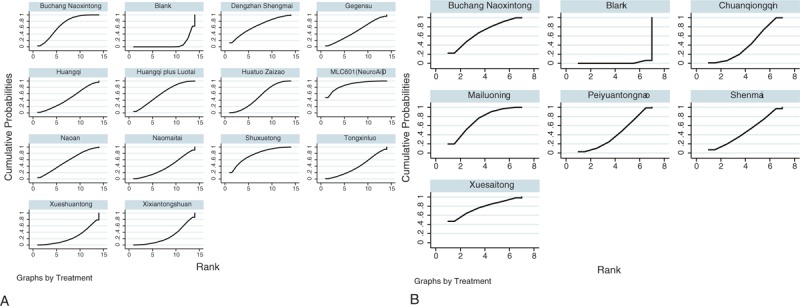
The cumulative ranking plots based on the estimated from SUCRA probabilities for overall effect. A, Without acupuncture. B, Combined with acupuncture. The cumulative ranking plots based on the estimated from SUCRA probabilities for major outcome. SUCRA that expresses the percentage of effectiveness each treatment was first compared with an ideal drug. The plot shows cumulative probabilities versus ranks for all treatments in network analysis. SUCRA = surface under the cumulative ranking.
Table 4.
The league table of the network meta-analysis for the therapeutic effectiveness of Chinese herbal patent medicines with acupuncture on post stroke recovery.
4. Discussion
In this study, we systematically analyzed the effect of Chinese herbal patent medicine on the recovery of patients after a stroke and suggest that these medicines have a significant positive effect on stroke recovery. Chinese patent medicine significantly improved the neurological function defect scores, the BI scores, and the FMA. In general, the medicines were found to be effective for stroke recovery. The network meta-analysis showed that MLC601, Shuxuetong, and BuchangNaoxintong were most likely to facilitate stroke recovery without acupuncture, while Mailuoning, Xuesaitong, BuchangNaoxintong were most likely to improve stroke recovery when combined with acupuncture.
MLC601 (NeuroAiD, DanqiPiantan Capsule) is a Chinese drug use in stroke recovery. NeuroAiD consists of 9 herbs (Radixastragali, Radix Salviamiltiorrhizae, Radix PaeoniaeRubra, RhizomaChuanxiong, Radix AngelicaeSinensis, Carthamustinctorius, Prunuspersica, Radix Polygalae, and RhizomaAcoriTatarinowii) and 5 animal components (Hirudo, EupolyphagaseuSteleophaga, CalculusBovis Artifactus, Buthusmartensii, and CornuSaigaetataricae). A recent meta-analysis including 4 randomized clinical trials suggested that MLC601 is not more effective than placebo in recovery after stroke[19]; however, we found that MLC601 was likely to improve stroke recovery. The different results were likely because we excluded studies that included acute stage stroke treatment.
Shuxuetong injection, composed of hirudo and pberetima, is commonly used in TCM for the treatment of ischemic cerebrovascular events. Shuxuetong affects blood rheology, and may prolong clotting time, reduce platelet adhesion, increase arterial blood flow, and inhibit thrombosis. Shuxuetong inhibits BCL-2-associated X protein and caspase-3 induced nerve cell death by promoting BCL-2 expression.[57] In addition, Shuxuetong reduces inflammation as assessed by levels of high-sensitivity C-reactive protein and homocysteine.[58] Hirudo and pberetima are widely used in traditional medicine to promote blood circulation and remove blood stasis.
The potential mechanisms were as follows: stroke is neurological condition resulting from local vascular abnormalities. Neural cells in the center of the injury region may suffer irreversible injury and cell death. Oxygen-free radicals are produced in the ischemic penumbra, and reperfusion of the area results in the death of additional neurons. The Chinese herbal medicines Honghua and Danshen, the main components in BuchangNaoxintong, are used clinically to activate blood circulation and dissipate blood stasis.
Nonpatented Chinese herbal medicines were also used to treat the complications of stroke. The most frequently used nonpatented Chinese herbal medicine was BuyangHuanwu Decoction, which contains ChuanXiongQin, Hunagqi, and other herbal components.[59] In the treatment of severely disabled patients, or invalids, the dose of Hunagqi is increased, which invigorates the distribution of medicines such as SanQi, HongHua, and Danshen. In this study the combination of Chinese patent medicines improved poststroke recovery in a manner similar to traditional Chinese medicines that were not patented.
Traditional Chinese medicine treatment of poststroke recovery has several challenges, including dialectical complexity, multiple prescriptions, and lack of uniformity of drugs. Therefore, we prefer to use standardized Chinese patent medicines to treat complications of stroke. There are few randomized clinical trials (RCTs) that have evaluated the combination of Chinese patent medicine on the treatment of stroke sequelae. Further clinical studies of Chinese medicine, using modern medical research methods, could provide more reliable results.
We analyzed the effectiveness of Chinese herbal patent medicines for stroke recovery by traditional meta-analysis. Our study suggests that Chinese herbal patent medicines promote functional neurological recovery after stroke. We performed subgroup analysis according to the method of drug delivery (oral or intravenous) and whether the Chinese herbal patent medicines were or were not combined with acupuncture. In our study, we could not conclude that oral administration is better than intravenous. However, because of the diverse and complex components of herbal medicines, intravenous injection may have a higher incidence of adverse reactions, while adverse reactions to oral drugs are uncommon. Chinese herbal medicines with or without acupuncture have similar results. Acupuncture-related randomized controlled trials are needed to confirm the effect of acupuncture on patients’ poststroke.
We did not analyze stroke patients in acute phase because the main purpose of acute phase treatment is to reduce the mortality and disability rate. The purpose of acute phase treatment is to rapidly reduce intracranial pressure, reduce cerebral edema, prevent infection, and provide symptomatic treatment. Chinese herbal medicine is mainly used to protect nervous system function and is not the main treatment for an acute stroke.
The individualized treatment model, rather than the model generalized to the population, was always used for patients receiving Chinese herbal medicines. In the current study, the treatment effect was evaluated by comparing patients treated with Chinese herbal patent medicines with patients who did not receive Chinese herbal patent medicine. For other individualized treatments model was balanced between intervention and control group. Although potential confounders may influence the treatment effect, we describe a systematic and comprehensive review for the treatment effect of Chinese herbal medicines on poststroke recovery.
Chinese herbal medicine is the traditional medicine in China, and provides an important supplement in the treatment of stroke sequelae for Western Medicine. Although TCM has been used in China for thousands of years, it is not popular outside China. The main reason is that when the Chinese medicine enters a foreign market, it is necessary to obtain approval from the drug administration agency of the country. Most Chinese herbal medicines are obtained from plants and animals with diverse and complex compositions. Therefore, identification of the specific composition is difficult. In addition, some Chinese medicine contains harmful trace elements, such as mercury and lead that limit use in the Western world. Chinese medicine has the principle of dialectical treatment, meaning that for the same disease different medications should be administered according to the TCM symptoms of the specific patient. This view is different from Western medicine theories. However, with the internationalization of China, the modernization of TCM research has begun. The Philippines, Singapore, France, and Iran have accepted MLC601 (NeuroAiD, called DanqiPiantan Capsule in China), for the treatment of stroke sequelae. Chinese medicine has a long history and many types of drugs. The effectiveness of many Chinese medicines needs to be scientifically confirmed before international acceptance of these medicines occurs.
The double-blind randomized placebo-controlled study is an important study design to evaluate the effectiveness of medical interventions. In the past, Chinese scientists had a lower level of knowledge of study design, especially in tested patients. Thus, well-designed RCTs are not common in China. In addition, it is complicated to design a placebo control for Chinese medicine and other natural medicines. The color, smell, and taste are difficult to simulate with nontherapeutic ingredient. However, Chinese scientists have explored creating placebo herbal drugs. Dilution of the drugs or removal of the effective components can result in a placebo that retains the original appearance and smell, with minimal therapeutic effect. Placebo preparation of natural drugs for use in clinical trials is an urgent issue for Chinese scientists.
This study has several limitations. First, the results were based on previous studies, not on an individual patient level. Second, the outcome assessments have a relatively high degree of subjectivity. Third, due to the variety of herbal medicines, we could not classify the drugs based on their composition. Fourth, we did not analyze Chinese medicine formulae and nonpatent drugs. Fifth, although some studies did not distinguish between ischemic or hemorrhagic stroke, treatment using TCM is relative similar for both types of stroke and is based on identifying TCM syndromes. Further studies are needed to clarify the effective ingredients of Chinese herbal medicine. Sixth, data from Taiwan, Japan, and Korea were not included due to language restricted. Seventh, the criteria for significant improvement were different among the included studies, this could introduce uncontrolled biases and affect treatment effect for poststroke recovery. Finally, we originally intended to evaluate subgroup analysis based on life style; however, these data were not available.
The findings of this study indicate that the Chinese herbal patent medicines are effective for stroke recovery, and that MLC601, Shuxuetong, and BuchangNaoxintong are most likely to improve stroke recovery in patients not receiving acupuncture. In addition, Mailuoning, Xuesaitong, BuchangNaoxintong are most likely to improve stroke recovery in patients receiving acupuncture.
Supplementary Material
Footnotes
Abbreviations: BI = Barthel index, CBMdisc = China Biology Medicine disc, CI = 95% confidence interval, CNKI = China Knowledge Resource Integrated Database, CSPD = China Science Periodical Database, FIM = functional independence measure, FMA = Fugl–Meyer assessment, NDS = neurological functional defect scores, OR = odds ratios, PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses, SMD = standard mean difference, SUCRA = surface under the cumulative ranking, TCM = traditional Chinese medicine.
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Teasell R, Rice D, Richardson M, et al. The next revolution in stroke care. Expert Rev Neurother 2014;14:1307–14. [DOI] [PubMed] [Google Scholar]
- [2].Rehm J, Taylor B. Alcohol consumption, stroke and public health—an overlooked relation? Addiction 2006;101:1679–81. [DOI] [PubMed] [Google Scholar]
- [3].Wu X, Zhu B, Fu L, et al. Prevalence, incidence, and mortality of stroke in the Chinese island populations: a systematic review. PLoS One 2013;8:e78629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Malcolm MP, Vaughn HN, Greene DP. Inhibitory and excitatory motor cortex dysfunction persists in the chronic poststroke recovery phase. J Clin Neurophysiol 2015;32:251–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Coull AJ, Lovett JK, Rothwell PM. Population based study of early risk of stroke after transient ischaemic attack or minor stroke: implications for public education and organisation of services. BMJ 2004;328:326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Chen CL, Venketasubramanian N, Lee CF, et al. Effects of MLC601 on early vascular events in patients after stroke: the CHIMES study. Stroke 2013;44:3580–3. [DOI] [PubMed] [Google Scholar]
- [7].Venketasubramanian N, Lee CF, Wong KS, et al. The value of patient selection in demonstrating treatment effect in stroke recovery trials: lessons from the CHIMES study of MLC601 (NeuroAiD). J Evid Based Med 2015;8:149–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Borchers AT, Hackman RM, Keen CL, et al. Complementary medicine: a review of immunomodulatory effects of Chinese herbal medicines. Am J ClinNutr 1997;66:1303–12. [DOI] [PubMed] [Google Scholar]
- [9].Sucher NJ. Insights from molecular investigations of traditional Chinese herbal stroke medicines: implications for neuroprotective epilepsy therapy. Epilepsy Behav 2006;8:350–62. [DOI] [PubMed] [Google Scholar]
- [10].Zhang Z, Peng D, Zhu H, et al. Experimental evidence of Ginkgo bilobaextract EGB as a neuroprotective agent in ischemia stroke rats. Brain Res Bull 2012;87:193–8. [DOI] [PubMed] [Google Scholar]
- [11].Liu J. The use of Ginkgo biloba extract in acute ischemic stroke. Explore (NY) 2006;2:262–3. [DOI] [PubMed] [Google Scholar]
- [12].Rastogi V, Santiago-Moreno J, Dore S. Ginseng: a promising neuroprotectivestrategy in stroke. Front Cell Neurosci 2014;8:457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Hildebrandt JP, Lemke S. Small bite, large impact-saliva and salivary molecules in the medicinal leech, Hirudomedicinalis. Naturwissenschaften 2011;98:995–1008. [DOI] [PubMed] [Google Scholar]
- [14].Ji XY, Tan BK, Zhu YZ. Salvia miltiorrhiza and ischemic diseases. ActaPharmacol Sin 2000;21:1089–94. [PubMed] [Google Scholar]
- [15].Adams JD, Wang R, Yang J, et al. Preclinical and clinical examinations of Salvia miltiorrhiza and its tanshinones in ischemic conditions. Chin Med 2006;1:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Junhua Z, Menniti-Ippolito F, Xiumei G, et al. Complex traditional Chinese medicine for poststroke motor dysfunction: a systematic review. Stroke 2009;40:2797–804. [DOI] [PubMed] [Google Scholar]
- [17].Lu L, Li HQ, Fu DL, et al. Rhubarb root and rhizome-based Chinese herbal prescriptions for acute ischemic stroke: a systematic review and meta-analysis. Complement Ther Med 2014;22:1060–70. [DOI] [PubMed] [Google Scholar]
- [18].Ni X, Liu S, Guo X. Medium- and long-term efficacy of ligustrazine plus conventional medication on ischemic stroke: a systematic review and meta-analysis. J Tradit Chin Med 2013;33:715–20. [DOI] [PubMed] [Google Scholar]
- [19].Gonzalez-Fraile E, Martin-Carrasco M, Ballesteros J. Efficacy of MLC601 on functional recovery after stroke: a systematic review and meta-analysis of randomized controlled trials. Brain Inj 2016;30:267–70. [DOI] [PubMed] [Google Scholar]
- [20].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Ades AE, Lu G, Higgins JP. The interpretation of random-effects meta-analysis in decision models. Med Decis Making 2005;25:646–54. [DOI] [PubMed] [Google Scholar]
- [23].Stuck AE, Rubenstein LZ, Wieland D. Bias in meta-analysis detected by a simple, graphical test. Asymmetry detected in funnel plot was probably due to true heterogeneity. BMJ 1998;316:469. [PMC free article] [PubMed] [Google Scholar]
- [24].Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088–101. [PubMed] [Google Scholar]
- [25].Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000;56:455–63. [DOI] [PubMed] [Google Scholar]
- [26].White IR, Barrett JK, Jackson D, et al. Consistency and inconsistency in network meta-analysis: model estimation using multivariate meta-regression. Res Synth Methods 2012;3:111–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Li D, Wang T, Shen S, et al. Effects of fluroquinolones in newly diagnosed, sputum-positive tuberculosis therapy: a systematic review and network meta-analysis. PLoS One 2015;10:e0145066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Trinquart L, Chatellier G, Ravaud P. Adjustment for reporting bias in network meta-analysis of antidepressant trials. BMC Med Res Methodol 2012;12:150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Goto H, Satoh N, Hayashi Y, et al. A chinese herbal medicine, tokishakuyakusan, reduces the worsening of impairments and independence after stroke: a 1-year randomized, controlled trial. Evid Based Complement Alternat Med 2011;2011:194046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Yang R, Wang H. Curative effect observation of combination of acupuncture with medicine therapy for stroke. J Clin Acupuncture Moxibustion 1997;12–3. [In Chinese]. [Google Scholar]
- [31].Liu G, Wu Y. Comprehensive treatment of 80 cases of cerebral infarction sequela. J Pract Traditional Chin Med 2003;19:415.[In Chinese]. [Google Scholar]
- [32].Huang J, Zeng H, Xu J. Observation on the therapeutic effect of acupuncture combined with intravenous infusion in the treatment of apoplexy sequelae. Chin Gen Pract 2005;8:1193–4. [In Chinese]. [Google Scholar]
- [33].Wang C. Observation of 30 cases of acute cerebral vascular disease with the treatment of acute cerebral vascular disease with the combination of Shen Mai injection and acupuncture. J Pract Traditional Chin Med 2005;21:73.[In Chinese]. [Google Scholar]
- [34].Wu Yanyang Clinical observation on the treatment of 60 cases of sequela of apoplexy by acupuncture and massage together with medicine. Guiding J Traditional Chin Med 2006;12:41–2. [In Chinese]. [Google Scholar]
- [35].Kong KH, Wee SK, Ng CY, et al. A double-blind, placebo-controlled, randomized phase II pilot study to investigate the potential efficacy of the traditional Chinese medicine Neuroaid (MLC 601) in enhancing recovery after stroke (TIERS). Cerebrovasc Dis 2009;28:514–21. [DOI] [PubMed] [Google Scholar]
- [36].Harandi AA, Abolfazli R, Hatemian A, et al. Safety and efficacy of MLC601 in Iranian patients after stroke: a double-blind, placebo-controlled clinical trial. Stroke Res Treat 2011;2011:721613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Bavarsad Shahripour R, Shamsaei G, Pakdaman H, et al. The effect of NeuroAiD (MLC601) on cerebral blood flow velocity in subjects’ post brain infarct in the middle cerebral artery territory. Eur J Intern Med 2011;22:509–13. [DOI] [PubMed] [Google Scholar]
- [38].Liang J. To observe the clinical efficacy of Naoxintong Capsule in the treatment of stroke recovery period. Shenzhen J Integr Traditional Chin Western Med 2014;24:50–1. [In Chinese]. [Google Scholar]
- [39].Yao L. The clinical curative effect of 43 cases of recovery of Buchangnaoxintong capsule in the treatment of stroke. Tianjin Pharmacy 2010;22:31–2. [In Chinese]. [Google Scholar]
- [40].Cao X, Zhou X, Zhuang H. Clinical observation on the treatment of dengzhanshengmai capsule in the recovery stage of ischemic wind-stroke. Global Traditional Chin Med 2012;05:56–7. [In Chinese]. [Google Scholar]
- [41].Lin L, Peng X, Shi H, et al. Clinical observation on the treatment of Butylphthalide Soft Capsules plus Naoxintong Capsule in the recovery stage of qi deficiency and blood stasis syndrome cerebral infarction: a report of 60 cases. Guiding J Traditional Chin Med Pharmacy 2015;59–61. [In Chinese]. [Google Scholar]
- [42].Ying W. Therapeutic effect of Puerarin Injection on the treatment of cerebral infarction. Zhejiang J Integr Traditional Chin Western Med 2002;12:690.[In Chinese]. [Google Scholar]
- [43].Wei C. Clinical analysis on prevention and treatment of Apoplexy by HuaTuo reconstruction pill. Health Care Today b 2013;[In Chinese]. [Google Scholar]
- [44].Zhang J, Guo A. Curative effect observation on the treatment of 130 cases of Apoplexy by HuaTuo reconstruction pill. Guangdong Med J 2009;30:296.[In Chinese]. [Google Scholar]
- [45].Mai L, Huang L, Qian H, et al. Effect of Huangqi Injection on the change of 24-hour dynamic blood pressure in elderly patients with cerebral infarction at convalescent stage. Chin J Clin Rehabil 2006;10:30.[In Chinese]. [Google Scholar]
- [46].Tan Z, Li P, Sun G. Capsule combined western medicine treatment of cerebral stroke recovery QDBS Observation of 76 Cases. Popular Sci Technol 2013;132–3. [In Chinese]. [Google Scholar]
- [47].Lin X. Clinical observations of Naomaitai Capsules plus compound cerebroproteinhydrolysate tablets on old patients with convalescing cerebral infarction. Chin J Exp Traditional Med Formulae 2013;19:314–6. [In Chinese]. [Google Scholar]
- [48].Ma Y, Lan R. Clinical observation on 35 cases of recovery phase of ischemic apoplexy treated by the combination of cerebral embolism and rehabilitation training. Liaoning J Traditional Chin Med 2011;394–5. [In Chinese]. [Google Scholar]
- [49].Li W. Pei-yuan brain capsule, acupuncture combined with western medicine stroke recovery randomized parallel group study treatment. J Pract Traditional Chin Internal Med 2015;167–70. [In Chinese]. [Google Scholar]
- [50].Zheng X. Clinical observation of Shuxuetong injection in the treatment of ischemic stroke (recovery). Gansu J TCM 2008;21:15.[In Chinese]. [Google Scholar]
- [51].Yuan S, Li F. Clinical observation of the effect of Tongsaimai Tablets Combined with rehabilitation training on stroke hemiplegia. J New Chin Med 2009;57–8. [In Chinese]. [Google Scholar]
- [52].Lei W, Wu Y, Huang L. Effect of Tongxinluo capsule on ability of activities of daily living of old reconvalescent with cerebral infarction. Hebei J TCM 2007;29:739–41. [In Chinese]. [Google Scholar]
- [53].Wang W. The effects of tongxinluo capsule on patients with convalescent brain infarction. Chin J Difficult Complicated Cases 2006;5:331–3. [In Chinese]. [Google Scholar]
- [54].Niu X, Zou W, Zhao Y, et al. XixianTongshuan capsule combined with aspirin in the treatment of ischemic stroke recovery of phlegm and blood stasis syndrome in 56 cases. J Traditional Chin Med 2013;54:1056–7. [In Chinese]. [Google Scholar]
- [55].Ge X, Jin Y, Wang Y, et al. Combined acupuncture and medicine in treating 60 cases of apoplexy sequelae. China's Naturopathy 2009;17:30.[In Chinese]. [Google Scholar]
- [56].Yu R, Chen C, He S. Summarization on 98 cases of ischemic apoplexy convalescent period treated by combination of TCM and western medicine. Guiding J TCM 2006;12:26.[In Chinese]. [Google Scholar]
- [57].Qiao H, Dong L, Zhang X, et al. Protective effect of luteolin in experimental ischemic stroke: upregulated SOD1, CAT, Bcl-2 and claudin-5, down-regulated MDA and Bax expression. Neurochem Res 2012;37:2014–24. [DOI] [PubMed] [Google Scholar]
- [58].Ran X, Diao JX, Sun XG, et al. Huangzhi oral liquid prevents arrhythmias by upregulating caspase-3 and apoptosis network proteins in myocardial ischemia-reperfusion injury in rats. Evid Based Complement Alternat Med 2015;2015:518926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Hu HQ. Recent development of Chinese therapies for apoplexy sequel. J Henan Coll Traditional Chin Med 2003;18:83–5. [In Chinese]. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


