INTRODUCTION
Most international organizations accept 7% as a reasonable glycated hemoglobin (HbA1c) value to aim for, while managing diabetes.[1,2,3] These organizations also suggest targets for fasting plasma glucose (FPG) and postprandial plasma glucose (PPG) which should be achieved with optimal glucose-lowering treatment.[1,2,3]
The three parameters, HbA1c, FPG, and PPG, together form the glycemic triad.[4] An understanding of the deleterious effects of glycemic variability (GV), mediated in part though oxidative stress, later led to the creation of a unified glucose tetrad concept.[5] This helped in improving clinical decision-making and in planning therapeutic interventions.
THE EARLY PENTAD
Further awareness of the needs of persons with diabetes informed the development of the glycemic pentad.[6] To the four glycemic parameters listed above, the pentad added quality of life (QoL). The glycemic pentad highlighted the importance of patient-reported outcomes (PROs) and underlined the relevance of the biopsychosocial model of health to diabetology. This pentad was a person-centered or patient-centered tool, meant to help achieve better outcomes. QoL was included as it is a measurable target, which contributes to long-term outcomes in diabetes care.
THE GLYCEMIC PENTAD
However, it was felt that QoL was not a glycemic parameter in the strict sense, and its inclusion was not warranted in a list of glycemic targets. Discussion on this topic helped prepared another framework, with five glucose-related variables: HbA1c, FPG, PPG, minimal GV, and minimal hypoglycemia.[7,8] This rubric is justified as all five investigations listed are related to glycemia, are independently related to cardiovascular outcomes, and are important targets of glucose-lowering therapy.
THE GLYCEMIC HEXAD
Fueled by enhanced focus on safety and tolerability of drugs, modern research has revealed subtle differences in the pathophysiology, presentation, and clinical implications of day-time hypoglycemia and nocturnal hypoglycemia. With this in mind, the glycemic pentad has been expanded to the glycemic hexad. The hexad lists three efficacy-oriented targets (HbA1c, FPG, and PPG) along with three safety-oriented goals (hypoglycemia, nocturnal hypoglycemia and GV). The six-point concept has been published as the Glycemic Sixer,[9] a term which resonates with cricket playing nations.
NUMBERS AS TOOLS
Number-based constructs such as the ones mentioned above are useful pedagogic tools, which also serve as frameworks upon which to plan and evaluate glucose-lowering therapy. Use of these models allows an treating physician to create a glucophenotype[10] or glucotype of an individual patient and choose the most appropriate therapy. The chosen treatment modalities help in achieving effective glucose control, in a safe and well-tolerated manner. This process has been facilitated by the development of modern insulin analogs, oral fixed-dose combination, and injectable glucagon-like peptide 1 receptors, which provide effective glucose control with low risk of hypoglycemia.
COMPREHENSIVE THERAPEUTIC APPROACH
Diabetes management, however, is much more than glucose-lowering alone. The glucocentric approach, in fact, has long been abandoned in favor of a comprehensive one, which targets multiple metabolic pathways and systems. The four main vasculometabolic targets[11] in diabetes care can be listed as the Metabolic Quartet (HbA1c, blood pressure, weight, and lipids).
THE THERAPEUTIC PENTAD
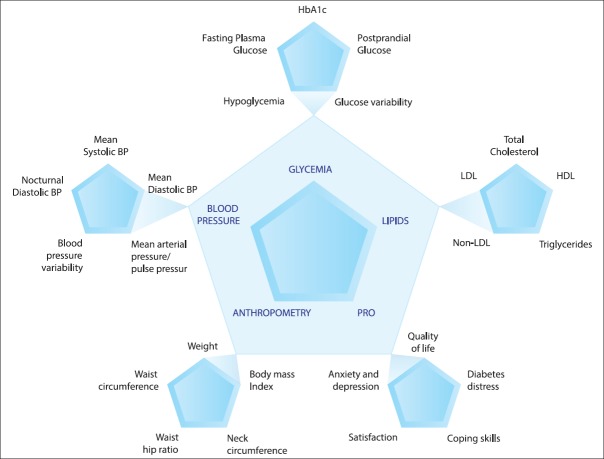
To this quartet, we suggest addition of PROs. Inclusion of PROs to this model reinforces patient-centered or person-centered care as a pillar of diabetes management. It reminds the physician that the person with diabetes care has a right to evaluate treatment regimens. This therapeutic pentad, or pentad of targets, provides guidance to the physician in planning management strategies [Figure 1].
Figure 1.
The therapeutic pentad and pentuplets. BP: Blood pressure, HDL-C: High-density lipoprotein-cholesterol, LDC-C: Low-density lipoprotein-cholesterol
THE FIVE PENTUPLETS
Each angle of this pentad can further be expanded, to serve as a teaching tool. This taxonomic structure is similar to that used by the ancient Indian physician, Atreya, who propounded Atreya's quadruple.[12] His quadruple lists four components, which are essential for optimal medical outcome. These are the physician, patient, drug, and attendant. For each stakeholder, Atreya describes four properties, thus creating four equipowerful quadruplets. Similarly, we can embellish the therapeutic pentad and create five quintuplets, to provide a comprehensive list of targets that must be addressed in diabetes management. This serves as an exhaustive list of evidence-based end-points, which contribute toward improving both biomedical and psychosocial, health, in persons with diabetes.
THE THERAPEUTIC HEXAD
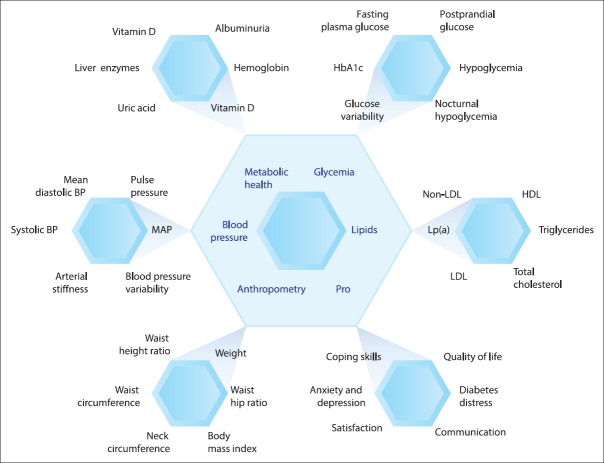
Diabetology is an ever-evolving science[13] and its complexity is bound to grow. Insights into pathophysiology and salutogenic factors of diabetes, coupled with pharmaceutical developments, will increase the range of targets in diabetes management. We therefore propose a therapeutic hexad, or sixer, with six accompanying sextuplets. The sixth angle that we add is metabolic health, which includes nonglycemic investigations related to renal, hepatic, and metabolic parameters. The relationship of these “numbers” to cardiovascular outcomes is well documented and backed by evidence [Figure 2].
Figure 2.
The therapeutic hexad and hexuplets. BP: Blood pressure, HDL-C: High-density lipoprotein-cholesterol, LDC-C: Low-density lipoprotein-cholesterol, LP (a): Lipoprotein (a), MAP: Mean arterial pressure, PRO: Patient-reported outcome
FROM TOOLS TO TARGETS
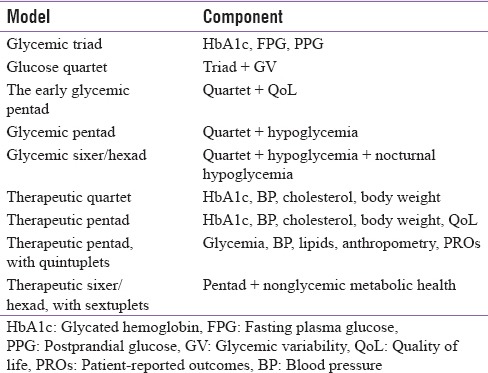
The rubrics discussed in this editorial are not ends in themselves. Rather, they utilize a numerophile strategy to prepare teaching tools which are easy to understand, teach, and learn [Table 1]. We note, with appreciation, usage of these models at national level across South and Southeast Asia and efforts of experts to achieve concordance of existing therapies with our models.[14] The models convert complex theory into simple (but not simplistic) knowledge, which informs pragmatic clinical decision-making. This, in turn, helps achieve optimal health for persons living with diabetes.
Table 1.
Various glycemic and therapeutic models in diabetes care
REFERENCES
- 1.Garber AJ, Abrahamson MJ, Barzilay JI, Blonde L, Bloomgarden ZT, Bush MA, et al. Consensus statement by the American association of clinical endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm-2017 executive summary. Endocr Pract. 2017;23:207–38. doi: 10.4158/EP161682.CS. [DOI] [PubMed] [Google Scholar]
- 2.Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, et al. Management of hyperglycemia in type 2 diabetes, 2015: A patient-centered approach: Update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015;38:140–9. doi: 10.2337/dc14-2441. [DOI] [PubMed] [Google Scholar]
- 3.Qaseem A, Barry MJ, Humphrey LL, Forciea MA. Clinical Guidelines Committee of the American College of Physicians. Oral pharmacologic treatment of type 2 diabetes mellitus: A clinical practice guideline update from the American College of Physicians. Ann Intern Med. 2017;166:279–90. doi: 10.7326/M16-1860. [DOI] [PubMed] [Google Scholar]
- 4.Beisswenger P, Heine RJ, Leiter LA, Moses A, Tuomilehto J. Prandial glucose regulation in the glucose triad: Emerging evidence and insights. Endocrine. 2004;25:195–202. doi: 10.1385/ENDO:25:3:195. [DOI] [PubMed] [Google Scholar]
- 5.Monnier L, Colette C, Owens DR. Integrating glycaemic variability in the glycaemic disorders of type 2 diabetes: A move towards a unified glucose tetrad concept. Diabetes Metab Res Rev. 2009;25:393–402. doi: 10.1002/dmrr.962. [DOI] [PubMed] [Google Scholar]
- 6.Kalra S, Kalra B. The glycemic pentad: Role of insulin analogues. Webmedcentral. 2010 [Google Scholar]
- 7.Kalra S, Bajwa SJ, Baruah M, Sehgal V. Hypoglycaemia in anesthesiology practice: Diagnostic, preventive, and management strategies. Saudi J Anaesth. 2013;7:447–52. doi: 10.4103/1658-354X.121082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kalra S. Hypoglycaemia in diabetes. J Pak Med Assoc. 2014;64:1090–3. [PubMed] [Google Scholar]
- 9.Kalra S. The Glycaemic Sixer. J Pak Med Assoc. [PubMed] [Google Scholar]
- 10.Kalra S, Gupta Y. The gluco-phenotype. J Pak Med Assoc. 2016;66:118–9. [PubMed] [Google Scholar]
- 11.Kaplan NM. The deadly quartet: Upper-body obesity, glucose intolerance, hypertriglyceridemia, and hypertension. Arch Intern Med. 1989;149:1514–20. doi: 10.1001/archinte.149.7.1514. [DOI] [PubMed] [Google Scholar]
- 12.Kalra S, Kalra B, Agrawal N. Therapeutic patient education: Lessons from Ayurveda: The quadruple of Atreya. Internet J Geriatr Gerontol. 2010;5:10. [Google Scholar]
- 13.Kalra S, Baruah MP, Kalra B. Diabetes care: Evolution of philosophy. Indian J Endocrinol Metab. 2017;21:495–97. doi: 10.4103/ijem.IJEM_109_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The Glycemic Pentad Forum: Glycemic Pentad. JAPI. 2017;65:68–79. [PubMed] [Google Scholar]