Fig. 3.
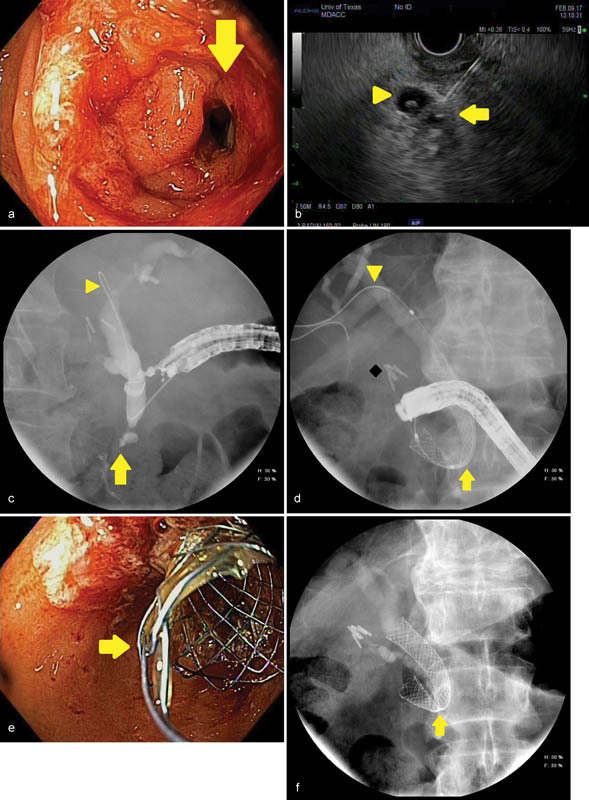
An image series is presented to illustrate endoscopic ultrasound (EUS)-guided biliary access in a 73-year-old man with an unresectable, infiltrating pancreatic cancer complicated by combined biliary obstruction and gastroduodenal outlet obstruction. ( a ) A high-grade duodenal stenosis (arrow) is identified obstructing the area of the papilla, which prevents endoscope passage for conventional endoscopic retrograde cholangiopancreatography (ERCP). ( b ) An endosonographic image obtained shows EUS being used to pass a 19-gauge needle through the scope into the bile duct (arrow). A periampullary diverticulum is noted with internal debris (arrowhead). ( c ) Fluoroscopy confirms a distal biliary stricture (arrow) following passage of an angled-tip 0.035 inch by 460-cm guidewire (arrowhead) through the needle; the needle and EUS scope are subsequently withdrawn leaving the guidewire in place. ( d ) The ERCP scope is passed over the guidewire and a covered metal biliary stent is deployed (arrow), creating a therapeutic choledochoduodenal fistula for biliary drainage. The guidewire (arrowhead) and deployment catheter are then removed. Surgical clips after cholecystectomy are noted (diamond). ( e ) Endoscopic image obtained with the ERCP scope demonstrating the covered metal biliary stent (arrow) emanating from the medial wall of the duodenal bulb. ( f ) The final fluoroscopic image after completion of the procedure confirms appropriate position and expansion of the metal biliary stent. A narrowing or “waist” is seen in the stent as it passes through the duodenal wall (arrow).
