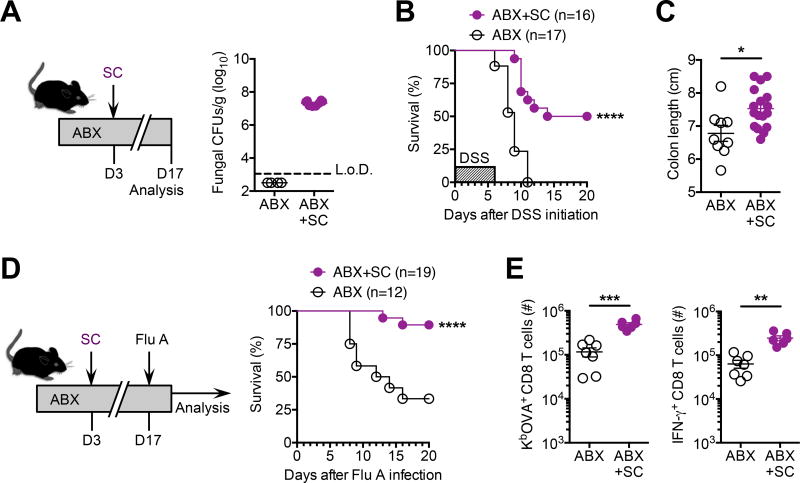
Figure 2. Saccharomyces cerevisiae intestinal mono-colonization overturns disease susceptibility induced by commensal bacteria depletion.
(A) Recoverable fungal colony forming units (CFUs) in the feces of specific-pathogen free mice administered S. cerevisiae (SC) and maintained on drinking water supplemented with an antibiotic cocktail containing ampicillin, gentamicin, metronidazole, neomycin, vancomycin for 14 days (ABX+CA), compared with antibiotic treated controls without SC inoculation (ABX).
(B) Percent survival after DSS supplementation in the drinking water (for six days) for mice described in panel (A).
(C) Colon length after DSS treatment (for six days) for mice described in panel (A).
(D) Percent survival after influenza A PR8-OVA (Flu A) intranasal infection (6 × 104 PFUs) for mice described in panel (A).
(E) Total number of Flu A-specific KbOVA tetramer+ CD8 T cells (left), and IFN-γ+ CD8 T cells after in vitro OVA257–264 peptide stimulation (right), from lungs nine days after Flu A infection for mice described in panel (A).
*P < 0.05, **P < 0.01, ***P < 0.001, by ****P < 0.0001, Log-rank (Mantel-Cox) test (B,D) or unpaired t-test with Welch’s correction (C,E). Data are representative of at least two independent experiments each with similar results. Bars, mean ± s.e.m. L.o.D., limit of detection.