Abstract
Objective
Five to ten percent of interstitial cystitis/bladder pain syndrome (IC/BPS) patients have Hunner's lesions (HL), areas of non-specific inflammation and scarring. The poor quality of life of patients with HL is entwined in associated pain and loss of bladder capacity. Although the decrease in bladder capacity is usually dependent on pain, it may also be dependent upon scarring and associated compliance changes produced by the inflammatory process. This report reviews the potential role of endoscopic scar lysis using the holmium laser in the management of these patients whose only other therapeutic option is urinary diversion.
Methods
Two patients with HL and “end stage” bladders who underwent holmium laser division of bladder wall scar/tethering were identified. Clinical data were reviewed with emphasis on safety and efficacy.
Results
Both patients selected for this procedure underwent holmium laser lysis of known scar tissue in an effort to increase bladder capacity and improve symptoms of urinary frequency and pain with bladder filling. The median age of patients who underwent the procedure was 63 (59–67) years. Incisions were made with the holmium laser at frequencies of 3–10 Hz of 300–700 J along the region of scarring. All procedures were performed by the same practitioner. There was an increase in bladder capacity by 58.3% (50.0%–66.7%). During a mean follow-up of 4.2 years, there appeared to be a significant improvement with an increase in interval time between voids and a decrease in pain with bladder filling.
Conclusion
Patients with IC/BPS may be severely debilitated by a clinically significant decrease in their bladder capacity, especially in the face of HL. The use of the holmium laser to incise regions of scar and bladder wall tethering may produce a clinically significant and durable increase in bladder capacity. The use of this technique as a means of treating bladder scarring poses an excellent adjunct to existing treatment strategies.
Keywords: Hunner's lesions, Bladder scar, Endoscopic lysis
1. Introduction
Interstitial cystitis/bladder pain syndrome (IC/BPS) is a chronic, often disabling condition characterized by bladder pain, urinary frequency, and urgency. Five to ten percent of patients with IC/BPS have Hunner's lesions (HL), regions of transmural inflammation appearing as patches of reddened mucosa, often associated with small vessels radiating from a central pale scar [1]. These areas of inflammation and scarring usually result in the severe symptoms typically described in this patient population. The HL are thought to be the cause of pain; however, the associated scarring of the bladder appears, in many instances, to be associated with tethering of the bladder wall and changes in bladder capacity and compliance [2]. Furthermore, although fulguration of HL is a recommended therapy, concern has been raised that these procedures, while improving pain, may be associated with increased bladder wall scarring [3].
Ultimately, some IC/BPS patients with HL develop an “end stage” bladder on the basis of bladder wall fibrosis; with the only further option of care being urinary diversion. This highlights the need for a treatment strategy aimed at increasing bladder capacity while having low potential to create further bladder wall scarring. The holmium laser may be able to provide such benefits in patients with HL. The use of holmium laser as a means of therapy has been widely used in the field of urology [4]. To date, however, there have been no published reports on the use of this form of energy to treat the bladder wall changes seen in this select group of patients. The following report will explore two cases in which the holmium laser was used to incise bladder wall scar, thereby improving bladder capacity.
2. Cases
A chart review of two patients with IC/BPS and known scar formation were identified. Operative reports from cystoscopy and use of holmium laser were reviewed.
In both cases the holmium laser was used at 3–10 Hz and 300–700 J during cystoscopic visualization under general anesthesia. Postoperative follow-up was recommended within 2 weeks of the procedure. Routine follow-up was arranged at 3, 6, and 12-month intervals. Symptomatic data on clinical improvement during follow-up visits were obtained with medical record review. Data on follow-up were obtained over a period of 4.2 years.
2.1. Descriptions of case No. 1
A 66-year-old female with a history of IC/BPS complicated by multiple HL presented in consultation for increasing bladder pain and frequency. Office cystoscopy demonstrated extensive bladder wall scarring and mucosal tethering. Filling produced severe pain at approximately 30 mL. The patient had previously failed multiple medical and intravesical therapies and was otherwise a candidate for urinary diversion. Unfortunately, the use of bowel for reconstruction was limited due to her history of Crohn's disease with high grade stricture of distal ileum and a stable entero–entero fistula. The patient had undergone prior cystoscopic procedures with fulguration of HL, injection of triamcinolone into areas of scarring, and hydrodistention. In an attempt to increase her bladder capacity and manage pain, the patient selected to proceed with endoscopic lysis of her bladder scar. Preoperative CT scan showed no suggestion of an enterovesical fistula. No bowel was identified adjacent to the region of scar. The patient was counseled on the possibility of intraperitoneal rupture and the need for post operative foley catheterization.
Intraoperatively, scar and mucosal tethering originating along the right posterior mid lateral wall was identified. The bladder underwent distention with normal saline to approximately 60 cm H2O in order to facilitate separation of the scar as the incision was deepened. Using a 550 μm fiber, three incisions were created with the holmium laser at frequencies of 3–10 Hz and 300–400 J along the region of scarring down to perivesical fat. Minimal bleeding was encountered through the scarred regions (Fig. 1). A Foley catheter was left in situ for 1 week. Subsequent cystogram showed no extravasation. The patient was instructed to proceed with a bladder retraining (holding) protocol in order to maintain her bladder capacity.
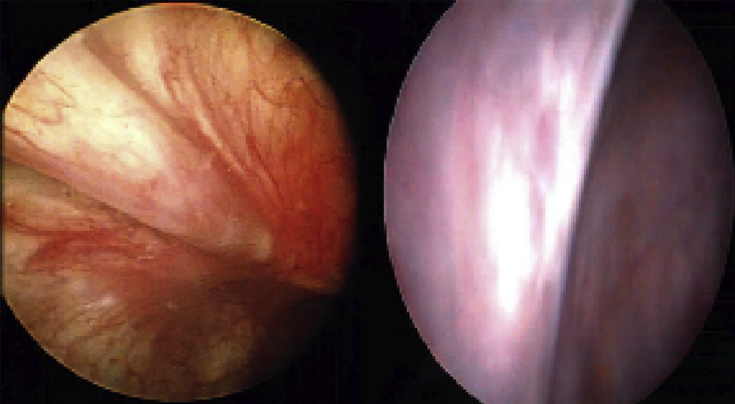
Figure 1.
Bladder scar with mucosal tethering.
During immediate follow-up, the patient reported improvement in her urinary frequency. She found an increase in the duration between voids and felt a significant decrease in pain with bladder filling. During cystoscopy approximately 2 years later there appeared to be continued bladder scarring in the posterior right mid lateral wall; however, distinct areas of normal bladder mucosa in this region were also noted. The patient tolerated bladder filling to approximately 60 mL.
2.2. Descriptions of case No. 2
A 59-year-old female with a history of IC/BPS presented in consultation for bladder pain and increased urinary frequency. During the patient's clinical evaluation she underwent cystoscopy which demonstrated HL with multiple areas of scar and mucosal tethering. Her bladder capacity during in-office cystoscopy was 120 mL. She had undergone prior cystoscopic procedures with fulguration of HL, injection of triamcinolone into areas of scarring, and hydrodistention without improvement of her symptoms. The patient's past surgical history was significant for multiple abdominal hernia repairs, hysterectomy, and removal gangrenous large bowel. Preoperative CT scan showed no abnormalities. The patient subsequently underwent cystoscopy where a large area of banding scar was identified along the right posterior bladder wall. This area was divided in several regions with a holmium laser using frequencies of 3–10 Hz and 700 J during slow hydrodistention of the bladder to approximately 60 cmH2O. A 550 μm fiber was used for this procedure (Fig. 2). A Foley catheter was left in situ for 1 week. Subsequent cystogram showed no extravesical extravasation. As with patient in the first case, she was asked to proceed with a bladder holding protocol.
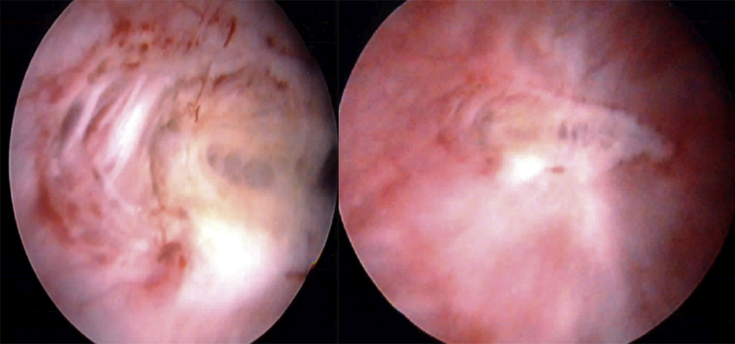
Figure 2.
Incision of bladder scar with holmium laser. Note the exposure of perivesical fat.
During immediate follow-up, the patient reported improvement in her urinary frequency. Her pain with bladder filling appeared to improve (from 8/10 on pain scale to 5/10) per patient report. Repeat in-office cystoscopy approximately 2 years later still revealed significant posterior bladder wall scarring with tethering; however, her bladder capacity at this time was increased to 200 mL through in-office cystoscopy.
3. Discussion
The use of the holmium laser to improve the bladder capacity of those patients with severe bladder wall scarring is a novel technique that has not previously been explored. The two IC/BPS patients presented suffered from severe bladder wall fibrosis, mucosal tethering, and loss of bladder capacity [5], [6]. Both had failed previous conservative management, endoscopic ablative procedures, and steroid injections to their HL. Although each was a candidate for urinary diversion, this procedure produced a relatively large increase in bladder capacity and, most importantly, had a favorable impact on their quality of life. These clinical benefits appear to be secondary to a notable increase in bladder capacity after the procedure.
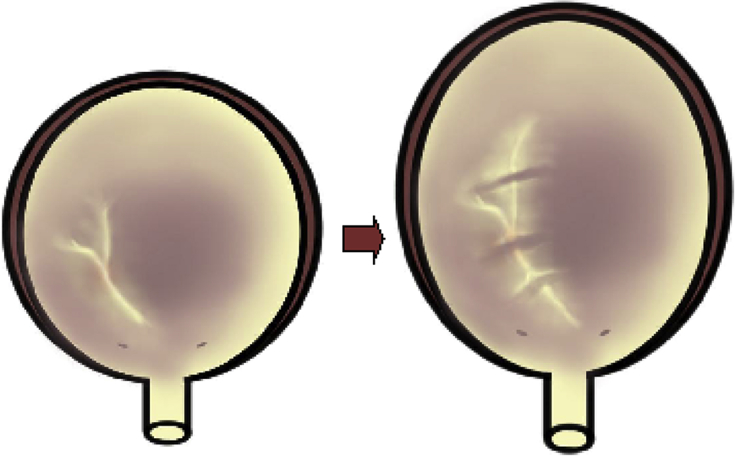
The etiology of decreased bladder compliance and capacity in patients with HL can be attributed to bladder pain and bladder wall scarring [7], [8]. In this instance, improvement in bladder capacity is based upon small increases in the bladder's radius producing a profound effect on its volume through the simple relationship V = 4/3 πr3. Thus, a 50 mL bladder capacity can be doubled through a 0.6 cm increase in its radius. This effect was clinically evident with a mean increase in bladder capacity after the use of the holmium laser by 58.3% (50.0%–66.7%) (Fig. 3).
Figure 3.
Increase in bladder capacity after holmium laser division of scar tissue.
The holmium laser for management of endoscopic scar lysis in patients with HL was chosen because of its theoretical ability to minimize further bladder scarring in a patient with a preexisting marked reduction in bladder capacity. Indeed, the holmium laser is commonly used in the endoscopic management of urethral stricture disease [9] and when employed for treatment of urethral carcinoma, was associated with a stricture rate of less than 9% [10], [11], [12]. In addition, the necessity for tissue contact, the small fiber size, and its average depth of tissue penetration of 0.5 mm allows for the incisions to be performed with precision and with little surrounding tissue trauma [10]. We found slow hydrodistention with saline to be helpful during the procedure to separate the tissue as the incision was elongated. In both patients, scar traversed the entire bladder wall and incisions needed to be carried down to perivesical fat (Figure 1, Figure 2). Care should be taken to limit operative time particularly when there is concern for extravesical fluid extravasation. Patients should be counseled about the possibility of intraperitoneal extravasation, particularly when dividing dome lesions.
The median interval time between cystoscopic procedures that were performed in office to determine bladder capacity was 2.2 years. During a mean follow-up of 4.2 years, there appeared to be a significant increase in time between voids and a decrease in pain with bladder filling. However, these improvements were most pronounced during the first 3–6 months after the procedure. In order to prevent or delay the redevelopment of scar, we have stressed the need for a post operative bladder holding protocol where the patient is asked to defer daytime voiding approximately 15–20 min beyond their normal sensation of fullness.
While it is clear that patients must still undergo strict bladder retraining protocols, this treatment may prove to be an excellent adjunct to triamcinolone injections and fulguration of these lesions. While this report documents two such cases, future studies aimed at a larger population size in addition to further prospective studies will allow for further characterization of this technique as a means of treatment and may have applicability to other conditions where severe bladder wall fibrosis also poses an issue.
4. Conclusion
The two presented cases demonstrate the use of holmium laser to divide scar tissue and thereby increase bladder capacity by more than 50.0%, ultimately improving symptoms associated with IC/BPS. The effects of the procedure were most pronounced 3–6 months after therapy with both patients reporting an increase in interval time between voids and a decrease in pain with bladder filling. The use of the holmium laser is an innovative technique for treating bladder scarring that poses an excellent adjunct to existing treatment strategies in patients with IC/BPS.
Conflicts of interest
Dr S Bahlani declares no conflict of interest. Dr R Moldwin: Taris Biomedical (Medical advisory board, investigator); Urigen Pharmaceuticals (Medical advisory board); Afferent Pharmaceuticals (Investigator).
Footnotes
Peer review under responsibility of Chinese Urological Association and SMMU.
References
- 1.Hanno P.M., Burks D.A., Clemens J.Q., Dmochowski R.R., Erickson D., Fitzgerald M.P. AUA guideline for the diagnosis and treatment of interstitial cystitis/painful bladder syndrome. J Urol. 2011;185:2162–2170. doi: 10.1016/j.juro.2011.03.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Payne C.K., Joyce G.F., Wise M., Clemens J.Q. Interstitial cystitis and painful bladder syndrome; urologic diseases in America project. J Urol. 2007;177:2042–2049. doi: 10.1016/j.juro.2007.01.124. [DOI] [PubMed] [Google Scholar]
- 3.National Institute of Diabetes and Digestive and Kidney Diseases . National Institutes of Health; 2012. Interstitial cystitis/painful bladder syndrome. [Google Scholar]
- 4.Elzayat E.A., Al-Mandil M.S., Khalaf I., Elhilali M.M. Holmium laser ablation of the prostate versus photoselective vaporization of prostate 60 cc or less: short-term results of a prospective randomized trial. J Urol. 2009;182:133–138. doi: 10.1016/j.juro.2009.02.117. [DOI] [PubMed] [Google Scholar]
- 5.Sastry D.N., Hunter K.M., Whitmore K.E. Urodynamic testing and interstitial cystitis/painful bladder syndrome. Int Urogynecol J. 2010;21:157–161. doi: 10.1007/s00192-009-1015-6. [DOI] [PubMed] [Google Scholar]
- 6.Kim S.H., Kim T.B., Kim S.W., Oh S.J. Urodynamic findings of the painful bladder syndrome/interstitial cystitis: a comparison with idiopathic overactive bladder. J Urol. 2009;181:2550–2554. doi: 10.1016/j.juro.2009.01.106. [DOI] [PubMed] [Google Scholar]
- 7.Berry S.H., Elliott M.N., Suttorp M., Bogart L.M., Stoto M.A., Eggers P. Prevalence of symptoms of bladder pain syndrome/interstitial cystitis among adult females in the United States. J Urol. 2011;186:540–544. doi: 10.1016/j.juro.2011.03.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Macdiarmid S.A., Sand P.K. Diagnosis of interstitial cystitis/painful bladder syndrome in patients with overactive bladder symptoms. Rev Urol. 2007;9:9–16. [PMC free article] [PubMed] [Google Scholar]
- 9.Wollin T.A., Denstedt J.D. The holmium laser in urology. J Clin Laser Med Surg. 1998;16:13–20. doi: 10.1089/clm.1998.16.13. [DOI] [PubMed] [Google Scholar]
- 10.Soderdahl D.W., Fabrizio M.D., Rahman N.U., Jarrett T.W., Bagley D.H. Endoscopic treatment of upper tract transitional cell carcinoma. Urol Oncol. 2005;23:114–122. doi: 10.1016/j.urolonc.2004.10.010. [DOI] [PubMed] [Google Scholar]
- 11.Razvi H.A., Chun S.S., Denstedt J.D., Sales J.L. Softtissue applications of the holmium: YAG laser in urology. J Endourol. 1995;9:387–390. doi: 10.1089/end.1995.9.387. [DOI] [PubMed] [Google Scholar]
- 12.Kelly D.C., Das A. Holmium laser enucleation of the prostate technique for benign prostatic hyperplasia. Can J Urol. 2012;19:6131–6134. [PubMed] [Google Scholar]