Abstract
Rural residents’ health is challenged by high health care costs, chronic diseases, and policy decisions affecting rural health care. This single-case, embedded design study, guided by community-based participatory research principles and using mixed methods, describes outcomes of implementation of a community care team (CCT) and care coordination to improve outcomes of patients living in a frontier community. Seventeen organizations and 165 adults identified as potential care coordination candidates constituted the target populations. Following CCT development, collaboration and cohesion increased among organizations. Patients who participated in care coordination reported similar physical and lower emotional health quality of life than national counterparts; emergency department use decreased following care coordination. Key components identified as successful in urban settings seem applicable in rural settings, with emphasis on the key role of team facilitators; need for intense care coordination for people with complex health needs, especially behavioral health needs; and access to specialty care through technology.
Keywords: Primary health care, case management, patient-centered care, continuity of patient care, rural health, mental health, quality of life, community health workers, social determinants of health, medically underserved area, patient care team
Rural residents’ health is challenged by increasing health care costs and chronic diseases, longer life spans, and policy decisions differentially affcting funding for health services in rural communities.1,2 This embedded case study describes outcomes of implementation of a community care team (CCT) employing collaboration and care coordination to improve patient outcomes and reduce emergency room use in a frontier community, Ely, Minnesota, with a population of 3,450.3 An original partner in the Minnesota (MN) Health Care Homes project in 2011, the Ely CCT serves Northeastern (NE) Minnesota, a region with higher rates of poor physical and mental health days, poverty, and unemployment than the state and nation.4,5 Health care access is challenged by distance, two hours from the closest urban area. Concerned organizations, including the clinic, critical access hospital, schools, and mental health organizations, identified community care coordination as their evidence-based strategy to improve health outcomes in their community.6-8 Effectiveness of this strategy in rural communities has not been demonstrated, although projects such as the Vermont Blueprint for Health9 have led the effort.
Accountable Communities for Health in rural communities
In 2011, a national strategy was developed to implement the requirements of the Affordable Care Act10 and to improve patient and community health outcomes. It employed six priorities to achieve its aims;11 three (patient engagement, coordination of care, and working with communities)12,13 are key components of the Ely CCT. In 2015, the U.S. Department of Health and Human Services reported that these priorities led to improvements in patient and family satisfaction, less over-utilization of services such as emergency departments, improvement in health outcomes of people with chronic diseases, and increased community collaborations to improve overall wellness and prevent disease.14
Care coordination
Care coordination, a critical strategy to improve patient outcomes since the early 1900s,15 gained renewed visibility when family-centered medical homes began development in the 1980s to support children with disabilities and their families.16 In 2007, endorsement of family-centered medical homes by the American Academy of Family Physicians (AAFP), American Academy of Pediatrics (AAP), American College of Physicians (ACP), and American Osteopathic Association (AOA) brought care coordination to the forefront in primary care redesign,17 foreshadowing the key role of care coordination in Accountable Communities for Health (ACH). In 2012, the Agency for Healthcare Research and Quality detailed the role of care coordination in integrated primary care, while recognizing the wide range of diversity among care coordination models including who may conduct care coordination activities.7 For instance, patient navigators, community health workers, social workers, and nurses may conduct care coordination activities.18 The results of research regarding care coordination are mixed, though; they vary by community, the particular care coordination model being implemented, the target population, and reasons individuals are referred for care coordination (relevant social determinants of health and diagnoses).19-24 Care coordination in rural communities may be more challenging than in urban communities, because of 1) factors that contribute to poorer health outcomes such as poverty and 2) limited access to health care specialists (such as psychiatrists).7 Research regarding care coordination in rural communities is limited.24
Rural Accountable Communities for Health
The Ely CCT plan was influenced heavily by the Vermont Blueprint for Health project. Implemented in 2009, this statewide initiative to redesign primary care established regions, or hospital service areas (HSAs), was funded by health care payers.9 At each level of the project—statewide, HSAs, and primary care clinics—clinical and community teams were created. Although the scope of the Vermont model is statewide, many of its local projects were set in rural sites somewhat similar to Minnesota’s NE Iron Range.
A recent Prevention Institute study regarding critical components of ACH in Vermont and five other sites identified nine key components of an ACH: 1) a mission, 2) multisectoral partnerships, 3) an integrator organization, 4) a governance structure, 5) use of process and outcome data, 6) a strategic plan, 7) community engagement, 8) communications, and 9) sustainable financing.13 The five communities that formed the basis of the Prevention Institute study, in addition to the Vermont Blueprint for Health, were large population areas ranging from approximately 160,000 to over 3 million people. One of the five Prevention Institute Study’s communities, Pathways to a Healthy Bernalillo County, is among several pathways models being implemented nationally to meet the same aim as Vermont Blueprint for Health.25 The Pathways model employs community health workers to conduct outreach to high risk patients and offer care coordination. Interventions are based on so-called recipes for addressing psychosocial needs such as child care, housing, and transportation.26 Another evidence-based strategy, Project Echo, links specialists in urban areas, typically at medical schools, with providers and patients in primary care practices that would not otherwise have access to specialty care.27
Needs
Nationally, rural communities suffer health disparities relative to other communities. They are more likely than others to have health and dental workforce shortages, less likely to receive appropriate treatment for health issues such as acute myocardial infarction and hypertension, more likely to experience higher rates of serious and deadly injuries including suicide among men, and more likely to die at a younger age.28 People living in rural communities are disproportionately likely to suffer behavioral health disparities, less likely to receive mental health services, and more likely to receive fragmented services.29-31 Health outcomes are poorer in the NE Iron Range than in other areas in the county, state, and nation. A markedly high proportion of people have complications due to substance dependency, including opioid use; higher unemployment rates; suicide; and lower median household incomes.32-34 This geographic region is designated as both a Health Professional Shortage Area (HPSA; including mental health) and a Medically Underserved Areas/Populations (MUAs/MUPs).35
Poverty, one contributor to health disparities,36 is more prevalent in rural communities than elsewhere.37,38 Approximately 16.3% of people in rural areas live in poverty compared with 15.9% overall.39 Poverty in rural MN is increasingly problematic.40 Residents of the NE Iron Range area, a low-income population group, experience higher rates of poverty than the state average.41
Summary
Evaluation results of ACH are limited, especially in rural communities, given the recent development of ACHs.13 In 2012, the Agency for Healthcare Research and Quality (AHRQ) noted inconsistencies in evaluation of medical homes and recommended that future research measure change over time in typical clinics, using measures from other studies.8,42 Much research has focused on projects located in high population areas; organized around multiple payer support; and with services located in a centralized urban area. In contrast, this study describes the development of a rural, grassroots-driven, ACH project and patient and interorganizational outcomes. This study’s research questions are:
Did the creation of a community care team lead to increased interorganizational interactions?
What is the quality of life (QOL) of patients who participated in care coordination?
Did emergency department (ED) use change for people who participated in care coordination?
Methods
This study is a single-case, embedded design,43 guided by community-based participatory research principles (CBPR),44-46 using mixed methods. The method was designed to describe individual and system change occurring in a rural community implementing two evidence-based strategies, network development and care coordination, to improve patient outcomes. Based on CBPR principles, this study focuses on the rural Northeast Iron Range community as the unit of analysis and builds on its strengths, such as community networking to improve wellness. The study has been guided by a research team since the Ely CCT project began in 2011; demonstrating collaborative partnerships at each phase of the project. The team includes the researcher, a primary care physician, clinic manager, the CCT and Behavioral Health Network (BHN) project directors, care coordinators, administrators and staff representing other organizations participating in the CCT and BHN, and community members. The team is engaged in planning the research project, data collection, analysis, and dissemination of results. Results of the study have guided program and network development and evaluation of the project.
The chosen methodology, single-case, embedded design, is appropriate for this study, which seeks knowledge about the implementation of an accountable community for health project in a rural community, because the project is unique. The Ely CCT was the only rural pilot in the Minnesota State Innovation Model’s initial pilot, and Minnesota was only one of five states participating in that national project. Multiple strategies for collecting data at the individual and organizational level, while embedding sub-studies within the larger case study, provide rich information for examining the three research questions. Longitudinal data collection provides information regarding change over time in network development and client outcomes. The study has Essentia Health IRB approval; informed consent was obtained from people completing the wellness survey and the subject for whom the individual case study was created.
Population studied
The study included two samples, organizations participating in the Ely CCT and care coordination patients. Nineteen of the CCT’s 21 public and private nonprofit organizations completed a social network survey in 2015 (see Table 1). Although individual and family members serve on the Ely CCT, they did not complete the survey because their relationships with organizations are different than interorganizational relationships. Lack of community partner members’ anonymity poses a threat. The 143 adult patients receiving care coordination between 2012 and 2015 constitute the second sample. Demographic characteristics of the second sample are presented in the Results section.
Table 2.
MEAN NUMBER OF ENCOUNTERS BY LEVEL OF CARE COORDINATION
| Level | N | Mean | SD |
|---|---|---|---|
| Significant Service | 52 | 26.69 | 29.84 |
| Short-term Service | 63 | 3.08 | 2.081 |
| Referral/No Service | 28 | 1.75 | 1.71 |
N = 143
Measurement and data collection
Measurement tools and data collection methods varied within and across the three research questions. Both qualitative and quantitative data collection methods were used to answer the research questions regarding interor-ganizational interactions and care coordination. Change in ED use, a proxy measure for health care costs, was quantitative.47,48
Change in CCT
To describe change in the CCT, data were obtained through observation, ongoing interviews with staff, and network documents such as minutes of meetings and the strategic plan. Change in network interactions was measured by change in the number of participating organizations and changes in type of relationships using social network analysis (SNA) and through qualitative data regarding network growth. The initial SNA survey was developed in 2011, based on other similar surveys49-50 and consultation with the CCT Project Director; it was slightly revised in 2013 and 2014 to measure additional components of interorganizational relationships.49 Social network analysis uses the terms “nodes” and “vertices” to refer to participating organizations and “edges” to refer to relationships between organizations.51 The type of relationship was indicated by: No Relationship, Have A Limited Relationship, Have A Relationship and Would Like To Strengthen It, and Currently Working Together Successfully. The CCT Project Director emailed an invitation to one representative of each CCT organization to complete the survey in 2011, 2013, and 2015 with a link to the electronic survey. A second reminder was sent to all members and then individual emails to organizations who had not yet completed the survey, to encourage as full participation as possible. After the first SNA survey, interviews were conducted with each agency director to discuss the results of the SNA, ascertain whether they had any reservations about sharing the results publically, and obtain their recommendations for future surveys. Members expressed no reservations about sharing the data, had no recommendations for change in future surveys, and were interested in the results.
To develop the narrative regarding network growth, data were gathered through observation at network meetings and review of meeting minutes and documents establishing formal agreements between organizations.
Patient wellness
To describe the characteristics of the sample, patient characteristics (age, gender) and risk factors (smoking, body mass index [BMI])52 were retrieved from the patients’ clinic electronic health record (EHR) for the period of 2012 through February 2016. BMI was categorized into four categories: <18.5 = underweight, 18.5 to 24.9 = healthy, 25 to 29.9 = overweight, 30 = considered obese. Care coordinators rated their interaction with each patient as either Significant Service, Short-term Service, or Referral but No Service, in order to determine whether care coordination varied by demographics and risk factors (see Box 1).
Box 1. LEVEL OF INTENSITY OF CARE COORDINATION.
|
| |
| Level | Definition |
|
| |
| Significant Service | Care coordination with individuals with multiple, complex, persistent needs in multiple systems (physical, social, behavioral health). Includes development of care plan and systematic working through it. |
| Short-term Service | Needs met through short-term care coordination, including education, referrals, and follow up. |
| Referral/No Service | Referral received and service offered. Engagement unsuccessful. |
To measure wellness, patients age 18 and older who participated in care coordination between 2012 and 2015 were invited to complete the SF-36, a quality of life (QOL) measure with extensive research documenting psychometrics and appropriateness for people with chronic illness.8,11,53 Eight concepts of the SF-36: Physical functioning, Role limitations due to physical health, Role limitations due to emotional problems, Energy/fatigue, Emotional well-being, Social functioning, Pain, and General health, were computed. Interviews with patients were conducted at two points in time (May 2015 and January 2016). Patients received a phone call inviting them to participate in the study; those who agreed were invited to complete the survey at the clinic, the clubhouse—a nonprofit behavioral health recovery program, or another location of their choosing. After reviewing the informed consent document and signing it, patients were handed an iPad to complete the SF-36. After completion of the SF-36, patients received a $10 gift card as an incentive.
To enhance understanding of the relationship between care coordination and wellness, a representative case study was created; information was drawn from care coordination records to compile the story.54
Health care costs
Historical and current ED use, a commonly used measure for health care costs, was captured from patients’ EHRs.47-48 Because of the complex environment of payers, many of whom do not share individual patient reimbursement costs, calculating actual ED costs is impractical. Therefore, the organization and this study employs ED use as a proxy for health care costs.
Data analysis
This single-case study, embedded design used several data analytic methods to answer the three research questions.
Question 1
Two narratives describing change in the size and scope of the CCT were created through review of existing documents and notes from observations and interviews. SPSS 23 and NodeXL Pro55 were used for analysis of quantitative data to answer the first research question. Data were formatted into the NodeXL format and imported into NodeXL and formatted separately for importing into SPSS 23. To describe changes in the CCT, frequencies by type of organizations by year were summarized. Change in organizational relationships was described using social network maps, and metrics (number of vertices, number of unique edges, and density) were calculated using NodeXL.50 Density is the number of relationships present in a network, divided by the possible number, as a measure of cohesion.51
Question 2
To answer the second research question, QOL was described using quantitative measures and a representative case study.52 Using SPSS 23,56 descriptive statistics were tabulated for patient demographics, characteristics, and QOL. Differences between the eight concepts and the individual item from the SF-36 between Time 1 and Time 2 and between this sample and a national sample were calculated using t-tests. To place the results of the SF-36 surveys into context, the results were compared with those of the Medical Outcomes Study.57 A case study representative of changes in QOL based on one patient’s experience was created, using guidance for writing medical case reports: describing the demographics, reason for case study, intervention, and responses to the intervention.55 Efforts were taken to anonymize the case study.
Question 3
Because the number of encounters differed dramatically by level of interaction for the 143 adults, those who had received Significant Service and who had data for six months prior to and after the first care coordination episode (n = 47, 36%) were included in this analysis (see Table 2).
The number and proportion of ED encounters for the six months prior to and after each adult’s first care coordination episode were calculated. This time period allowed the highest number of patients with data both pre- and post-first care coordination encounters.58,59 The percent change in encounters between Time 1 and Time 2 was calculated.
Results
The results of the single case, embedded study are presented through: 1) a description of the development of the CCT model—its growth, through social network analysis and narrative describing development of a second network inside the CCT; 2) care coordination and patient wellness through the SF-36 and a representative case study of an adult with behavioral health challenges; and 3) examination of change in ED use six months prior to the first care coordination encounter and the same period after the first encounter.
The creation of a community care team and increased interorganizational interactions
Development of the Ely CCT
The Ely Community Care Team, the focus of this embedded single-case study, is administered by the Essentia Health Ely Clinic (EHEC)—a rural clinic which is part of an integrated health system serving Minnesota, North Dakota, Wisconsin, and Idaho. The clinic provides primary care, including prenatal services, management of chronic conditions, and access to specialty services using telemedicine, to an area covering approximately 480 square miles. The region has approximately 12,000 permanent residents, with a dramatic population increase during summer months due to tourism in the Boundary Waters Canoe Area Wilderness and Superior National Forest. The Iron Range area in Northern Minnesota, historically a mining and logging region, is now a vacation destination. Located on the Canadian border, the area’s average annual temperature is 35 degrees Fahrenheit. Ely, the largest town in the target service area, is 50 miles from Virginia, MN, (population 8,712) where many agency headquarters are located, and 100 miles from Duluth (population 86,212), the largest and only urban area in St. Louis County. The northern portion of the county differs from greater St. Louis County, the largest geographic county east of the Mississippi River, with an older and poorer population who have reduced access to health care.
In 2010, EHEC recognized that some patients, especially people with behavioral health concerns, were being overlooked. Essentia Health Ely Clinic joined with the Minnesota Department of Health (MDH), the regional mental health center and Ely public school to form a network that successfully competed for a MDH Health Care Homes Division planning grant. The group participated in a learning community sponsored by the National Academy of State Health Policy (NASHP) and Commonwealth Fund and refined their focus, with care coordination and community collaboration as key strategies to improve health outcomes for people with complex health needs.
The Ely CCT project began July 2011 with MDH funding and has received additional state funding through the MDH State Innovation Model (SIM) grant, from the Centers for Medicare and Medicaid Services,60 to develop accountable communities for health. One primary care provider stated, “The CCT model essentially takes us from the model of the health care home to the health care neighborhood.”61[p. 32] Based on principles of family-centered medical homes,17,62 the Ely CCT model was comprised of a clinic team (primary care providers and community health workers) and a broader community team, in order to plan, implement, and evaluate their Accountable Community for Health project. Recognizing the critical role that social determinants of health play in health outcomes, the project director, who also served as care coordinator and community care team facilitator, spent much of the first year developing relationships with and between community organizations to create the Ely Administrative Collaborative. This group developed the CCT vision and mission statements, identified staff to participate in the CCT, and developed a multiagency release of information form that allowed staff to acknowledge shared clients and to collaborate. In 2012, the Ely CCT expanded to include 19 agency partners and two community and family partners. It held monthly meetings focusing on networking, developing tools and systems for collaboration, problem-solving challenges interorganizationally such as communication barriers, and care coordination. Celebrating its fourth anniversary, the Ely CCT now has 42 members representing community and family partners and 21 agency partners (see Figure 1). Care coordination and teamwork have expanded, with two clinic care coordinators, a care coordinator in the schools, and a part time care coordinator at the clubhouse serving adults with behavioral health issues. Community Care Team representatives serve on two additional school teams, a team focusing on elders with dementia, and the CCT’s Behavioral Health Network (BHN). Community Care Team organizations have collaborated to obtain grant funding to support teaming and programming. For instance, in fall 2015, a CCT subgroup developed the BHN to address gaps in services for people with behavioral health issues and obtained federal funding.
Figure 1.
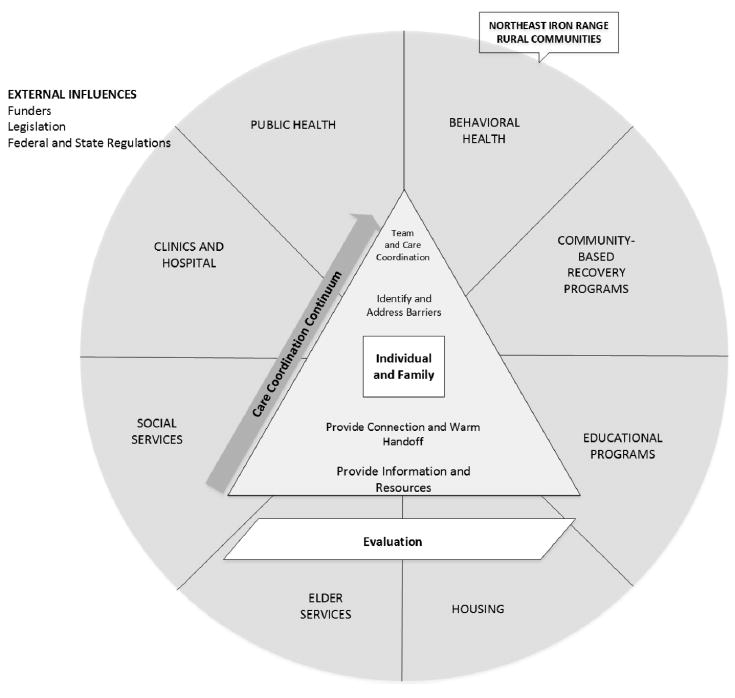
Ely Community Care Team Model.
Strategic planning
Development of the Ely CCT strategic plan began with the creation of a mission, vision, and annual workplans. The mission is: “The Community Care Team provides collaborative care and support to help you achieve your wellness goals.” Its vision is:
Adequate resources are available to citizens when needed to help them with their physical health, mental health, and psychosocial challenges. Professionals in health, education, and public service are trained in recognizing when someone is confronted with such challenges and are prepared to provide an appropriate response in giving assistance. Patients and their supporters have the tools and resources to help them be a partner in meeting their wellness, treatment and recovery goals.63[p. 2]
The Ely CCT created its 2015–2019 Strategic Plan in February 2015 with annual updates.
The Ely CCT model for care coordination
The Ely CCT model for care coordination, implemented first in the primary care clinic and now expanded to two other sites, includes outreach, assessment, referrals, and follow-up. Care coordinators have a variety of backgrounds: education, community health worker certification, bachelors in social work, and licensed practical nursing. Behavioral health and other specialty consultation is available through the regional mental health center and the health care system’s home location, an urban center 100 miles from the rural NE Iron Range area served by the Ely CCT.
Change in number and types of organizational relationships between 2012 and 2015
During the first year of the Ely CCT Project, the project director focused on developing relationships between organizations that served residents in rural NE Minnesota Iron Range communities. Seven organizations agreed to participate in an Administrative Collaborative supporting the Ely CCT and to assign staff to participate in care coordination. Representatives of 11 organizations completed the first social network analysis survey in late 2011, early 2012; the number of CCT organizations completing the survey increased to 19 in 2015. The percent of organizations that were “currently working together” increased consistently between Time 1, Time 2, and Time 3 (see Figure 2).
Figure 2.
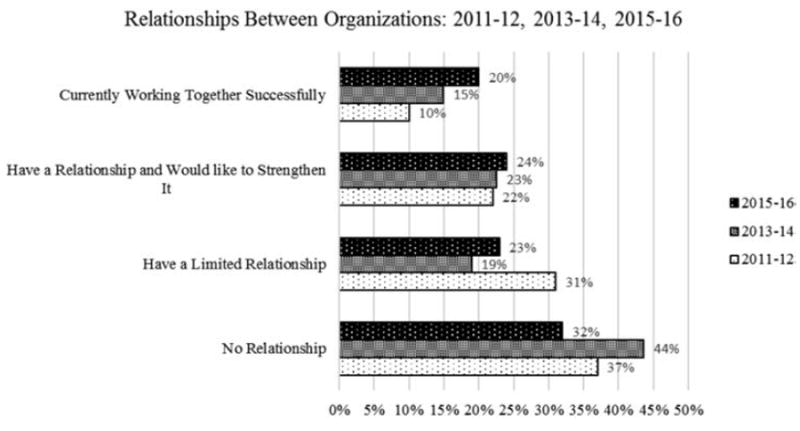
Relationships between organizations: 2011–12, 2013–14, 2015–16.
The number of vertices (or organizations) increased between Time 1 and Time 2; they decreased by two in Time 3 (see Table 3, Figure 3). The change between Time 2 and Time 3 represented a change rather than the loss of a key partner. In two instances, two different subunits of one organization completed the organizational survey in Time 2; therefore, in Time 3, each of the two parent organizations completed only one survey, thus dropping the total number of organizations to 19 in Time 3 and affecting the number of unique edges (relationships between organizations). The number of unique edges increased dramatically between Time 1 and Time 3. The density was similar in Time 1 and Time 2, and increased in Time 3, indicating an increase in cohesion between Time 2 and Time 3. Graphically depicting the relationships allows one to visualize the number of relationships where organizations are working together successfully (black, wide lines, with arrows indicating the direction of the relationships), such as the School-Early Childhood relationship. Grey lines indicate that an organization believes a relationship exists with another organization and they would like to strengthen it. This information provides an area for future growth in relationships, such as the mutual wish by the clubhouse and the free clinic to strengthen their existing relationship.
Table 4.
BMI RATES
| BMI Category | Frequency | Percent |
|---|---|---|
| Underweight | 8 | 4.8 |
| Healthy Weight | 42 | 25.5 |
| Overweight | 37 | 22.4 |
| Obese | 72 | 43.6 |
| Missing | 6 | 3.6 |
| Total | 165 | 100.0 |
Figure 3.
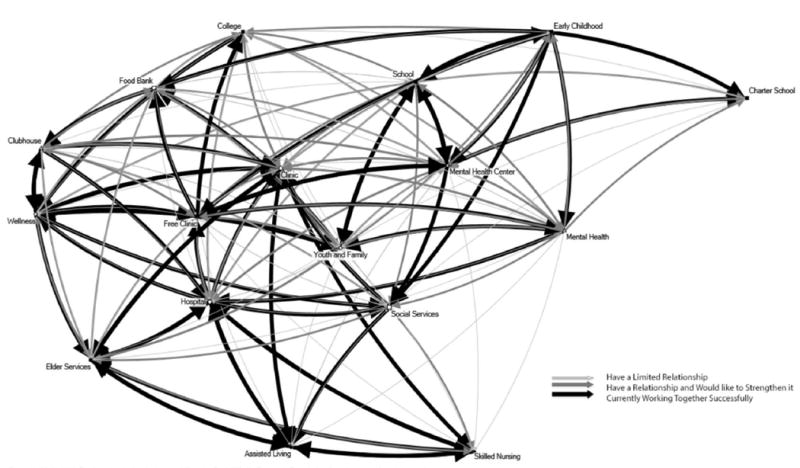
Status of relationships between Ely Community Care Team (CCT) organizations 2015.
Development of NE Rural Iron Range Behavioral Health Network
The CCT created a subgroup, the Behavioral Health Network (BHN), to focus on adult behavioral health, one example of Ely CCT’s success in meeting its mission to “provide collaborative care and support to help you achieve your wellness goals.”63[p. 2] Initial experience with care coordination led to the realization that most individuals referred for care coordination also had a behavioral health diagnosis and that current resources to address needs were insufficient. Additionally, this need was identified by the Ely CCT through the annual survey of network members. To address this need, in fall 2015 the Ely CCT created the BHN, a smaller network of five CCT organizations (a clinic, hospital, community college, mental health center, and clubhouse) to increase focus on development of solutions. The BHN’s goals are 1) to develop cross-agency systems for screening, referral, interventions, and follow-up for behavioral health issues; 2) to build capacity in the community to address behavioral health needs; and 3) to enable the community to embrace mental health as an integral part of health and wellness.
The BHN has obtained state and federal funding to develop its network and to address gaps in service. It has begun planning strategies such as routine screening, referral, and follow-up; a crisis response team; increased access to telemental health services; and methods to share patient data cross-agency. Behavioral Health Network organizations share responsibilities for the network; Well Being Development, the umbrella organization for the Northern Lights Clubhouse, is the fiscal agent and Project Director for the BHN; the team facilitator of the Ely CCT, an employee of EHEC, also facilitates BHN monthly meetings. The organization taking the lead in a particular initiative varies, depending on which one is most appropriate for that initiative. For instance, the local health clinic and mental health center are working closely together to facilitate increased telemental health access in the region; the free clinic and the clubhouse are focusing on a screening pilot; and the hospital and mental health center are taking the lead on expanding crisis management services to the area. The various types of relationships between organizations demonstrate the motivation of BHN members to work together (see Figure 4). For instance, the mental health center has a relationship with each of the other BHN organizations and would like to strengthen those relationships. That interest is reciprocated by three other members.
Figure 4.
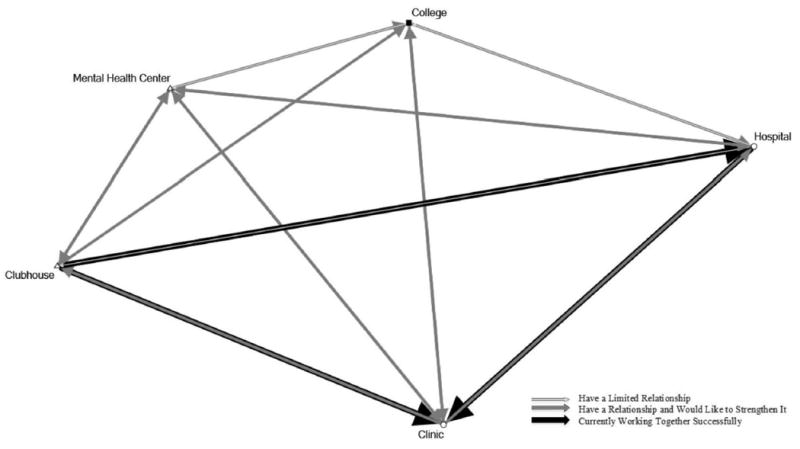
Status of relationships between behavioral health network organizations 2015.
Quality of life of adult patients who participated in care coordination
Adult patients receiving care coordination between 2012 and 2015
One-hundred and sixty-five patients had some level of involvement with care coordination between 2012 and 2015. The first care coordination encounter was October 2012; 66% of the 165 patients had enrolled prior to 2015, the rest in 2015. (An encounter includes face to face contact, a phone call, or other method employed by a care coordinator to interact with a patient; it might not have resulted in provision of services.) Most had been a patient at Ely Clinic for several years, with first contact ranging from April 2002 to March 2015, 88% had been a patient for more than five years. Ninety-five percent were White; 67% female; 22 were children age 2 to 17. The focus of this study is on adults; therefore, the results focus on the 143 adults, especially those who participated in long-term care coordination. The average age of the 143 adults age 18 and older was 41.72 (SD = 19.96, range 18 to 93); 71% were female. Women were on average older than men, with an average age of 44 versus men’s average age of 37 (t(163) = 2.337, p = .021). Eighty percent of adult patients had participated in Significant or Short-term care coordination (see Table 3). The level of intensity of care coordination did not vary by patient’s demographics (age and gender) and risk factors (BMI or whether they smoked). Forty-three percent of the 143 adults were currently smoking; 18% had smoked in the past. The mean BMI was 30.35 (SD 8.81, range from 15.91 to 65.48); 76% were overweight or obese (see Table 4).
Self-reported level of wellness
Adult patients identified as either short or long term recipients of care coordination were invited to participate in a pilot in mid-2015, completing the SF-36 as a measure of wellness (N = 19). The SF-36 was administered again in early 2016 (N = 27).
The level of wellness of people participating in care coordination who completed the survey in mid-2015 was statistically significantly lower than of the participants in the Medical Outcomes Study on seven of the eight concepts (see Table 5).57 Scores did not differ on the measure of general health or health change in the past year. People in both groups rated their health in general to be slightly above 50, or “good.” People in this study rated their health better than one year ago at the same level as the comparison group, slightly above 50, which is “about the same.”
Table 6.
LEVEL OF WELLNESS OF RECIPIENTS OF CARE COORDINATION: 2016
| Ely CCT (N = 27)
|
Medical Outcomes Study (N = 2471)
|
t | df | p | |||
|---|---|---|---|---|---|---|---|
| Time 2, Winter 2016 | Mean | SD | Mean | SD | |||
| Physical Functioning | 63.89 | 28.90 | 70.61 | 27.42 | – | – | NS |
| Role Functioning/Physical | 45.37 | 37.36 | 52.97 | 40.78 | – | – | NS |
| Role Functioning/Emotional | 44.44 | 42.37 | 65.78 | 40.71 | 2.708 | 2496 | .0068 |
| Pain | 52.22 | 26.41 | 70.77 | 25.46 | 3.764 | 2496 | .0002 |
| Energy/Fatigue | 40.19 | 25.81 | 52.15 | 22.39 | 2.756 | 2496 | .0059 |
| Emotional Wellbeing | 57.04 | 25.17 | 70.38 | 21.97 | 3.133 | 2496 | .0018 |
| Social Functioning | 50.00 | 25.00 | 78.77 | 25.43 | 5.848 | 2496 | .0001 |
| General Health | 50.93 | 25.23 | 56.99 | 21.11 | – | – | NS |
| Health Change | 62.04 | 28.898 | 59.14 | 23.12 | – | – | NS |
In 2016, the 27 people who completed the SF-36 scored lower on five of the components of the SF-36 than the participants in the Medical Outcomes Study (see Table 6). The two groups were similar in terms of rating of level of physical functioning, the impact of physical functioning on role, and general health. Patients who participated in this study rated their level of role functioning affected by emotional issues, their energy, emotional wellbeing, and social functioning as lower than participants in the Medical Outcomes Study; they also reported more pain. As with the previous survey results, the two groups did not differ on level of general health and health change. SF-36 scores at Time 1 and Time 2 did not differ.
Individual case study
To understand further who is served through care coordination and its impact, a single patient’s story was compiled. Wanda was chosen as representative of many who have complex medical and social issues and participate in significant care coordination. Wanda, a 30-year-old, White, single female, was referred to care coordination by her primary care provider for assistance with finances and health insurance. She had recently moved following a divorce and was homeless, sleeping on sofas and floors of family and friends where violence was common. Wanda was overwhelmed with grief following the divorce and by lack of experience with managing finances, complicated by chronic mental illness. Her previous health diagnoses included bipolar disorder, anxiety, post traumatic stress disorder, social anxiety, ovarian cysts, esophageal reflux, and gastritis.
As part of care coordination, Wanda set immediate goals: filling her prescriptions, obtaining funding for health care, and counseling. She recognized that consistency in her medication regimen was critical to her stability; to accomplish that she needed funding. Both Supplemental Security Income and Medical Assistance had been discontinued due to an error by the Social Security Administration when recording her change of status. Wanda and the care coordinator worked together, contacting county and federal agencies; ultimately Minnesota’s Disability Linkage Line identified the error, which took 28 days to rectify. The care coordinator connected Wanda with a crisis fund which covered prescription costs in the interim. Wanda was referred to a mental health provider and began counseling. Wanda’s Care Plan Priorities were: 1) I don’t want to cut (self-injury where one cuts one’s skin) anymore; 2) To be comfortable being alone; 3) Get back into drawing and find enjoyment in it; and 4) Like myself. In the first six weeks of participation in care coordination, Wanda had established a primary care provider, care coordination, membership in the clubhouse, an in-home mental health rehabilitative worker, and a relationship with a therapist. Wanda and her care coordinator developed strategies to reduce self-harm, including daily check in with the care coordinator and a relative to reinforce skills learned in counseling. At the 1-Year Care Plan Review, Wanda reviewed her goals and accomplishments: no cutting for four months, increased comfort being alone, an apartment, displayed quilt in community quilt show, developed coping mechanisms (walks, calling others for support), provided service to the community, stood up for herself in difficult interpersonal relationships, and experienced positive days at least 50% of the time. Wanda’s recent successes include participation in Wellness Recovery Action Plan (WRAP) training through the clubhouse and Mental Health First Aid training, increased skills to manage depression and anxiety (reading, art, breathing, reframing, walking), sold a quilt, and went 18 months with only one incident of self-harm. Given the chronic, cyclical nature of her illness, Wanda has experienced another episode of cutting, a depressive episode, and a difficult incident when a member of her support system stole her medications and money and introduced her to street drugs. When these episodes occurred, Wanda worked with her team, including the primary care physician, care coordinator, friend, therapist, in-home mental health worker, and clubhouse staff, to update her care plan. Success is marked by introducing new strategies as needed and returning to “having good days.”62
Emergency department use by people who participated in care coordination
To assess whether people who participated in care coordination had reduced ED use, the 47 people who received significant service were selected. Their average age was 48.43 (SD = 16.43); 75% were female. The average number of care coordination episodes during their participation in care coordination was 28.72 (SD = 30.65). Prior to care coordination, 29 patients had no ED visits, compared with 37 after six months participation in care coordination (see Table 7). Emergency department visits reduced 75%, from 58 ED visits in the six months prior to care coordination to 15 in the six months after.
Table 7.
EMERGENCY DEPARTMENT USE SIX MONTHS PRIOR TO AND AFTER FIRST CARE COORDINATION EPISODE (N = 47)
| 6 Months Pre First Care Coordination Episode
|
6 Months Post First Care Coordination Episode
|
|||||
|---|---|---|---|---|---|---|
| N of Episodes | N of Patients | % of Patients | Total ER visits | Frequency | Percent | Total ER visits |
| 0 | 29 | 61.7 | 0 | 37 | 78.7 | 0 |
| 1 | 11 | 23.4 | 11 | 6 | 12.8 | 6 |
| 2 | 4 | 8.5 | 8 | 3 | 6.4 | 6 |
| 3 | 1 | 2.1 | 3 | 1 | 2.1 | 3 |
| 13 | 1 | 2.1 | 13 | 0 | 0 | 0 |
| 23 | 1 | 2.1 | 23 | 0 | 0 | 0 |
| Total | 47 | 100 | 58 | 47 | 100 | 15 |
Discussion
Addressing the three research questions
Community care teams and interorganizational interactions
Implementation of the CCT, including 1) a network of health, behavioral health, social services, education, and recovery programs and 2) care coordination in a frontier community, was associated with increased collaboration between organizations and decreased health care use among patients with complex health problems.
The number of organizations in the network increased between Time 1 and Time 2. Cohesion (density) increased between Time 2 and Time 3. More satisfactory relationships were reported in Time 3 than previous times. The network also created a second network within the CCT, the BHN, to reduce gaps in services for adults with behavioral health challenges. The increased commitment to the CCT from the five organizations in the BHN demonstrates the network’s capacity to work together to obtain additional external funding for new initiatives and to increase collaboration between organizations for outreach, assessment, referral, and follow-up of people with complex needs including behavioral health needs. Satisfaction of BHN members with the CCT is higher than other members, as measured through an annual electronic, anonymous member survey. This suggests that member engagement around a specific project may increase satisfaction with the CCT as a whole.
When compared with the Prevention Institute study’s nine key components of an ACH, the Ely CCT measures up well.13 It developed 1) a mission early on and 2) initially included multi-sectoral partnerships across health, behavioral health, education, social services, and recovery programs. 3) The EHEC served as the integrator organization, initiating the development of the CCT and serving as the fiscal agent for external funding. Although EHEC plays a key role in management of the CCT, the CCT members share governance responsibilities and develop policy, select objectives and activities on which to focus annually, and share funding to accomplish goals through monthly and subgroup meetings. 4) The CCT governance structure, developed in the first year of the project, includes a team facilitator who recruits new partners, ensures continuous communication between partners, takes the lead in sustainability activities with collaboration from others, and ensures dissemination of information about the project. She is also the liaison with external entities. Feedback from an anonymous annual CCT member survey, which covers needs, satisfaction with the CCT, and next steps, guides annual planning meetings. Decision making is by consensus of CCT members. In this forum, the governance structure is addressed annually. Although satisfaction with the current governance structure has consistently been high, an extra effort is underway this year to examine sustainable models for the network should external funding no longer be available. 5) When the idea of creating a CCT emerged, the planners engaged a research partner from the Essentia Institute of Rural Health to ensure routine data collection. Results were disseminated, both for feedback for network development (process evaluation) and for measuring outcomes of interest to the broader organization and funders, especially reduced ED use. 6) The CCT initially created a workplan, with goals, objectives, and activities. It then created a formal strategic plan and revisits that plan annually. 7) Community engagement is the heart of the Ely CCT, for development of the network, outreach to people with complex health needs, and population health activities designed to improve wellness across the community. 8) The level of communication between network members is high, with monthly meetings of both the CCT as a whole and the BHN, meetings as needed for special projects, emails before and after each monthly meeting, and announcements electronically. Network members also communicate using video and phone conferencing to accommodate the broad geographical distances. 9)The Ely CCT has been funded continuously since 2011, through a variety of private and public funding sources, but ensuring financial sustainability is a challenge. The network is valued and continues to grow; in the past year two other organizations, a free clinic and public housing, have joined the network, because they see the value of the network to their organization and the people they serve.
Patient quality of life and ED use
People participating in care coordination at the clinic and clubhouse completed the SF-36, measuring QOL at two time periods. Patient-reported levels of QOL were lower than national norms on seven of eight QOL concepts in the first administration of the SF-36 and on five of the eight concepts in the second administration. The two SF-36 concepts regarding physical health were similar to national norms at Time 2. The areas that were rated low—emotional issues, energy, emotional wellbeing, social functioning, and pain—are consistent with having chronic behavioral health issues in addition to other health concerns. Determining what might be considered successful outcomes is complex in situations where it is not possible to resolve the underlying issues. It may be unrealistic to expect that care coordination can increase QOL in a linear and positive direction for people with complex needs. Care coordination may be appropriate as an ongoing service, with periods when intense interaction is needed. This may also affect ED use; during periods of crisis, increased use may indicate appropriate interventions. Emergency department use declined dramatically in the six months following enrollment in care coordination.
Limitations of this study
This study’s limitations include those common to case studies, the use of community-based participatory research, and qualitative data. Bias is difficult to control when one community is the unit of analysis, and members of the community being studied are members of the research team. Qualitative data are particularly sensitive to influence by those engaged in the study. The results are not necessarily generalizable to other communities. To address these limitations, the embedded design allowed for multiple sources of evidence; multiple qualitative and quantitative data collection methods and analysis were employed. Diverse members of the research team brought different views to the process and the product. Data were collected over time. The research team, network members, and individuals who participated in care coordination have provided feedback regarding the process and results of the study and informed the case study. Most importantly, the case study design allowed in depth examination of a complex, contemporary development in health care (accountable communities for health) and its impact on communities, organizations, and individuals.
Summary and recommendations
The Ely CCT project has increased interorganizational collaborations and care coordination for people with complex needs. Emergency department use decreased following enrollment in care coordination. The model is being implemented in other rural clinics within the health care system; information about the model has been disseminated regionally and nationally. The nine components of care coordination identified in urban settings provide guidance for replication of the model in rural settings. Both the team leader and time for the team leader to nurture the development of the network are key to the success of the multi-sectoral network. Learnings from this case study suggest that it is essential to work together at whatever level each organization is ready and able to collaborate, rather than one standard for level of collaboration and communication, to more effectively engage organizations in multi-sectoral networks. Engagement of organizations may vary over time.
Not identified in the Prevention Institute study but key to the success of the Ely CCT are champions within organizations that value the CCT and its benefit for patients and the community. Issues that continue to challenge network development and care team coordination include diverse standards regarding privacy of data; ongoing development of roles for community members; and diverse organizational, community, and family cultures. Some components not fully realized in the Ely CCT model that might improve the model as operationalized in other rural communities include: 1) consistent psychiatric consultation based on thorough chart review available through telehealth, especially for medication management and complex situations; 2) an in-house behavioral health specialist; and 3) enhanced relationship with public social service providers, especially for financial, food, medical, and housing assistance. As this model is implemented in other rural communities, additional opportunities exist to learn more about which components of the model are necessary for a successful rural health network and improved patient outcomes, including characteristics of the community, resources within the community, and individuals with complex needs and their families. Adding a more individualized measure of change, such as how patient goals are met through care coordination, longitudinally, will create a more accurate picture of realistic expectations for individuals participating in care coordination and improve measurement of outcomes.
Table 1.
CCT ORGANIZATIONS COMPLETING SNA SURVEY IN 2011, 2013, AND 2015
| Year
|
|||
|---|---|---|---|
| Type of Organization | 2011–12 | 2013–14 | 2015–16 |
| Clinics, Hospital, and Hospice | 3 | 4 | 3 |
| Public Health and Prevention | 2 | 2 | 3 |
| Education | 3 | 5 | 5 |
| Mental Health | 1 | 4 | 3 |
| Social Services | – | 3 | 2 |
| Elder Services | 2 | 3 | 3 |
| Total | 11 | 21 | 19 |
CCT = Community Care Team
SNA = Social Network Analysis
Table 3.
NETWORK METRICS
| Year | Vertices | Unique Edges | Graph Density |
|---|---|---|---|
| 2011–12 | 11 | 63 | .57 |
| 2013–14 | 19 | 191 | .56 |
| 2015–16 | 17 | 180 | .66 |
Table 5.
LEVEL OF WELLNESS OF RECIPIENTS OF CARE COORDINATION: 2015
| Ely CCT (N = 19)
|
Medical Outcomes Study (N = 2471)
|
t | df | p | |||
|---|---|---|---|---|---|---|---|
| Time 1, Spring 2015 | Mean | SD | Mean | SD | |||
| Physical Functioning | 55.26 | 32.21 | 70.61 | 27.42 | 2.43 | 2488 | .0153 |
| Role Functioning/Physical | 34.21 | 38.38 | 52.97 | 40.78 | 1.998 | 2488 | .0458 |
| Role Functioning/Emotional | 42.11 | 38.24 | 65.78 | 40.71 | 2.522 | 2488 | .0117 |
| Pain | 45.92 | 23.20 | 70.77 | 25.46 | 4.241 | 2488 | <.0001 |
| Energy/Fatigue | 39.21 | 22.69 | 52.15 | 22.39 | 2.509 | 2488 | .0122 |
| Emotional Wellbeing | 52.84 | 27.92 | 70.38 | 21.97 | 3.459 | 2488 | .0006 |
| Social Functioning | 48.68 | 25.38 | 78.77 | 25.43 | 5.138 | 2488 | .0001 |
| General Health | 53.42 | 25.00 | 56.99 | 21.11 | – | – | NS |
| Health Change | 57.89 | 31.24 | 59.14 | 23.12 | – | – | NS |
Acknowledgments
Funding Support:
State Innovation Model (SIM) Accountable Communities for Health (ACH) Pilot. Ely Community Care Team Pilot 7/1/11–6/30/12, Second Phase 11/4/14–12/31/16. This project is part of a $45 million State Innovation Model (SIM) cooperative agreement, awarded to the Minnesota Departments of Health and Human Services in 2013 by The Center for Medicare and Medicaid Innovation (CMMI) to help implement the Minnesota Accountable Health Model, awarded to Essentia Health Ely Clinic.
MDH Practice Transformation grant 3/26/15–10/31/2015: Awarded to Well Being Development to plan for behavioral health network.
Essentia Foundation July 1, 2012–June 30, 2013. Ely Community Care Team. Enhanced Evaluation of the Ely Community Care Team 11/1/2012–6/30/2014. Supplementing funding available for evaluation through the SIM programmatic grants.
Ely Community Health Worker Pilot 2/1/2014–6/30/2015. Funds awarded to the Essentia Health Ely Clinic to pilot the use of community health workers. Made possible with funds from the Essentia Health Foundation.
University of Minnesota Clinical and Translational Science Institute, Rural Community Capacity Enhancement 8/1/2012–7/31/2013
North St. Louis County Family Services Collaborative January 1, 2013–December 31, 2013
HRSA Network Planning Grant June 1, 2015–May 31, 2016: Planning and development of the Ely Behavioral Health Network, a network within the Ely Community Care Team, under the Rural Health Network Development Planning Grant Program (Grant # P10RH28450) to Well Being Development. This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.
Contributor Information
Pat Conway, Essentia Institute of Rural Health.
Heidi Favet, Essentia Health Ely Clinic.
Laurie Hall, Essentia Health Ely Clinic.
Jenny Uhrich, Northern Lights Clubhouse.
Jeanette Palcher, Essentia Institute of Rural Health.
Sarah Olimb, Essentia Institute of Rural Health.
Nathan Tesch, Essentia Institute of Rural Health.
Margaret York-Jesme, Essentia Health Ely Clinic.
Joe Bianco, Essentia Health Ely Clinic.
References
- 1.Peterson Center on Healthcare. Health of the healthcare system: an overview. Menlo Park, CA: Henry J Kaiser Family Foundation; 2015. Available at: http://k.org/slideshow/health-of-the-healthcare-system-an-overview/ [Google Scholar]
- 2.Goeres LM, Gille A, Furuno JP, et al. Rural-Urban differences in chronic disease and drug utilization in older Oregonians. J Rural Health. 2016 Jun;32(3):269–79. doi: 10.1111/jrh.12153. Epub 2015 Oct. http://dx.doi.org/10.1111/jrh.12153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.United States Department of Agriculture (USDA) 2010 Frontier and Remote FAR area codes data files. Washington, DC: USDA; 2015. Available at. [Google Scholar]
- 4.United Health Foundation. America’s health rankings annual report. Minnetonka, MN: United Health Foundation; 2015. Available at: http://www.americashealthrankings.org/reports/annual. [Google Scholar]
- 5.University of Wisconsin Population Health Institute. County health rankings and roadmaps 2012 rankings: Minnesota. Madison, WI: University of Wisconsin Population Health Institute; 2012. Available at: http://www.countyhealthrankings.org/sites/default/files/states/CHR2012_MN.pdf. [Google Scholar]
- 6.Craig C, Eby D, Whittington J. IHI Innovation Series white paper. Cambridge, MA: Institute for Healthcare Improvement; 2011. Care coordination model: better care at lower cost for people with multiple health and social needs. [Google Scholar]
- 7.Rich E, Lipson D, Libersky J, et al. Coordinating care for adults with complex care needs in the patient-centered medical home: challenges and solutions. Rockville, MD: Agency for Health care Research and Quality; 2012. [Google Scholar]
- 8.Peikes D, Zutshi A, Genevro J, et al. Early evidence on the patient-centered medical home. Rockville, MD: Agency for Health care Research and Quality; 2012. [Google Scholar]
- 9.Bielaszka-DuVernay C. Vermont’s blueprint for medical homes, community health teams, and better health at lower cost. Health Aff (Millwood) 2011 Mar;30(3):383–6. doi: 10.1377/hlthaff.2011.0169. http://dx.doi.org/10.1377/hlthaff.2011.0169. [DOI] [PubMed] [Google Scholar]
- 10.U. S. Department of Health and Human Services. About the law. Washington, DC: U. S. Department of Health and Human Services; 2015. Available at: http://www.hhs.gov/healthcare/about-the-law/ [DOI] [PubMed] [Google Scholar]
- 11.U. S. Department of Health & Human Services. 2011 report to congress: national strategy for quality improvement in health care. Washington, DC: U. S. Department of Health & Human Services; 2011. Available at: http://www.ahrq.gov/workingforquality/nqs/nqs2011annlrpt.htm. [Google Scholar]
- 12.Institute for a Sustainable Future. Commons health 2015: accelerating integrative approaches to health, community and wellbeing. Duluth, MN: Institute for a Sustainable Future; 2015. Available at: http://www.commonshealth.org/images/CH2015Reportfinal.pdf. [Google Scholar]
- 13.Mikkelsen L, Haar WL. Accountable communities for health: opportunities and recommendations. Washington, DC: Prevention Institute; 2015. Available at: http://healthcareinnovation.vermont.gov/sites/hcinnovation/files/Pop_Health/VT%20ACH%20Opportunities%20and%20Recommendations.pdf. [Google Scholar]
- 14.U.S. Department of Health and Human Services. Washington, DC: U.S. Department of Health and Human Services; 2015. Working for quality: achieving better health and health care for all Americans. Available at: http://www.ahrq.gov/workingforquality/reports/annual-reports/nqs2015annlrpt.pdf. [Google Scholar]
- 15.Hansan J. Cannon, Ida Maude. Richmond, VA: Virginia Commonwealth University; 2014. Available at: http://socialwelfare.library.vcu.edu/people/cannon-ida-maude/ [Google Scholar]
- 16.Dunst CJ, Trivette CM. Capacity-building family-systems intervention practices. J Fam Soc Work. 2009;12(2):119–43. http://dx.doi.org/10.1080/10522150802713322. [Google Scholar]
- 17.Joint principles of the patient-centered medical home. Washington, DC: Patient-Centered Primary Care Collaborative; 2007. Patient-Centered Primary Care Collaborative. Available at: http://www.aafp.org/dam/AAFP/documents/practice_management/pcmh/initiatives/PCMHJoint.pdf. [Google Scholar]
- 18.Witgert K, Kinsler S, Dolatshahi J, et al. Strategies for supporting expanded roles for non-clinicians on primary care teams. Washington, DC: National Academy for State Health Policy; 2014. [Google Scholar]
- 19.Archer J, Bower P, Gilbody S, et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev. 2012 Oct 17;10 doi: 10.1002/14651858.CD006525.pub2. CD006525. http://dx.doi.org/10.1002/14651858.cd006525.pub2. [DOI] [PubMed] [Google Scholar]
- 20.Joo JY, Huber DL. An integrative review of case management for diabetes. Prof Case Manag. 2012 Mar-Apr;17(2):72–85. doi: 10.1097/NCM.0b013e318243d473. http://dx.doi.org/10.1097/NCM.0b013e318243d473. [DOI] [PubMed] [Google Scholar]
- 21.Thota AB, Sipe TA, Byard GJ, et al. Collaborative care to improve the management of depressive disorders: a community guide systematic review and meta-analysis. Am J Prev Med. 2012 May;42(5):525–38. doi: 10.1016/j.amepre.2012.01.019. http://dx.doi.org/10.1016/j.amepre.2012.01.019. [DOI] [PubMed] [Google Scholar]
- 22.Community health workers: closing gaps in families’ health resources. Washington, DC: National Human Services Assembly; 2006. Family Strengthening Policy Center. [Google Scholar]
- 23.Brooks BA, Davis S, Frank-Lightfoot L, et al. Building a community health worker program: the key to better care, better outcomes, & lower costs. Macon, GA: Community Health Works; 2014. [Google Scholar]
- 24.McDonald KM, Sundaram V, Bravata DM, et al. Closing the quality gap: a critical analysis of quality improvement strategies. In: Shojania KG, McDonald KM, Wachter RM, et al., editors. Care coordination. Vol. 7. Rockville, MD: Agency for Health care Research and Quality; 2007. [PubMed] [Google Scholar]
- 25.Odufuwa O, Guerin P, Torres S. Pathways to a healthy Bernalillo county program—a cost study. Albuquerque, NM: University of New Mexico; 2015. [Google Scholar]
- 26.Community Care Coordination Learning Network-The Pathways Community HUB Institute. A companion to the pathways community hub manual. Rockville, MD: Agency for Health care Research and Quality; 2016. Connecting those at risk to care: the quick start guide to developing community care coordination pathways. [Google Scholar]
- 27.Feiden K. Project ECHO: bridging the gap in health care for rural and underserved communities. Princeton, NJ: Robert Wood Johnson Foundation; 2014. Available at: http://www.rwjf.org/content/dam/farm/reports/programresults_reports/2014/rwjf412743. [Google Scholar]
- 28.National Rural Health Association. What’s different about rural health care? Washington, DC: National Rural Health Association; 2016. Available at: http://www.ruralhealthweb.org/go/left/about-rural-health. [Google Scholar]
- 29.Fortney JC, Harman JS, Xu S, et al. The association between rural residence and the use, type, and quality of depression care. J Rural Health. 2010 Summer;26(3):205–13. doi: 10.1111/j.1748-0361.2010.00290.x. http://dx.doi.org/10.1111/j.1748-0361.2010.00290.x. [DOI] [PubMed] [Google Scholar]
- 30.Harman JS, Fortney JC, Dong F, et al. Assessment of the mental health funding marketplace in urban vs rural settings. Boulder, CO: Western Interstate Commission for Higher Education; 2010. [Google Scholar]
- 31.Russell L. Mental health care services in primary care: tackling the issues in the context of health care reform. Washington, DC: Center for American Progress; 2010. Available at: https://www.americanprogress.org/wpcontent/uploads/issues/2010/10/pdf/mentalhealth.pdf. [Google Scholar]
- 32.Substance Abuse and Mental Health Services Administration. Behavioral health barometer: Minnesota, 2013. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. [Google Scholar]
- 33.TwinCities.com. Prescription opiates and heroin in Minnesota. St. Paul, MN: St. Paul Pioneer Press; 2016. Available at: http://extra.twincities.com/car/maps/opiates/defaulthtm. [Google Scholar]
- 34.Homefacts. Ely, MN demographic data. Salt Lake City, UT: RealtyTrac; 2016. Available at: http://www.homefacts.com/demographics/Minnesota/St.-Louis-County/Ely.html. [Google Scholar]
- 35.Health Resources and Services Administration. Medically underserved areas/populations: guidelines for MUA and MUP designation. Rockville, MD: Health Resources and Services Administration; 1995. [Google Scholar]
- 36.Hout M, Lynch SM. Subjective health and income since 1972. Presented at: the Annual Meetings of the Population Association of America; New Orleans (LA). 2008. [Google Scholar]
- 37.Bailey JM, Preston K. Lyons, NE: Center for Rural Affairs; 2012. Census brief 3: poverty on the Great Plains. Available at: http://files.cfra.org/pdf/census-brief3-poverty.pdf. [Google Scholar]
- 38.Housing Assistance Council. Poverty in rural America. Atlanta, GA: Housing Assistance Council; 2012. Available at: http://www.ruralhome.org/storage/research_notes/rrn_poverty.pdf. [Google Scholar]
- 39.Minnesota Department of Health. Poverty & income. Minneapolis, MN: Minnesota Department of Health; 2016. Available at: https://apps.health.state.mn.us/mndata/poverty_basic#year. [Google Scholar]
- 40.Farrigan T, Parker T. The concentration of poverty is a growing rural problem. Washington, DC: U.S. Department of Agriculture Economic Research Service; 2012. [Google Scholar]
- 41.USA City Facts. Washington, DC: USA City Facts; 2015. Ely, MN income and economy. Available at: http://www.usacityfacts.com/mn/st—louis/ely/economy/ [Google Scholar]
- 42.Reid RJ, Coleman K, Johnson EA, et al. The group health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff (Millwood) 2010 May;29(5):835–43. doi: 10.1377/hlthaff.2010.0158. http://dx.doi.org/10.1377/hlthaff.2010.0158. [DOI] [PubMed] [Google Scholar]
- 43.Yin R. Case study research: design and methods. 5. Thousand Oaks, CA: Sage Publishing; 2014. http://dx.doi.org/10.4135/9781473915480.n48, http://dx.doi.org/10.4135/9781473915480.n38. [Google Scholar]
- 44.Simonds VW, Wallerstein N, Duran B, et al. Community-based participatory research: its role in future cancer research and public health practice. Prev Chronic Dis. 2013 May 16;10:E78. doi: 10.5888/pcd10.120205. http://dx.doi.org/10.5888/pcd10.120205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Minkler M, Wallerstein N, editors. Community-based participatory research for health: from process to outcomes. 2. San Francisco, CA: Jossey-Bass; 2008. [Google Scholar]
- 46.Israel BA, Schultz AJ, Parker EA, et al. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. http://dx.doi.org/10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 47.Honigman LS, Wiler JL, Rooks S, et al. National study of non-urgent emergency department visits and associated resource utilization. Western J Emerg Med. 2013 Nov;14(6):609–16. doi: 10.5811/westjem.2013.5.16112. http://dx.doi.org/10.5811/westjem.2013.5.16112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Blumenthal D, Malphrus E, McGinnis M, editors. Vital signs: core metrics for health and health care progress. Washington, DC: The National Academies Press; 2015. [PubMed] [Google Scholar]
- 49.Cross JE, Dickmann E, Newman-Goncha R, et al. Using mixed-method design and network analysis to measure development of interagency collaboration. Am J Eval. 2009 Sep;30(3):310–29. http://dx.doi.org/10.1177/1098214009340044. [Google Scholar]
- 50.Poole DL. Organizational networks of collaboration for community-based living. Nonprofit Management & Leadership. 2008;18(3):275–93. http://dx.doi.org/10.1002/nml.186. [Google Scholar]
- 51.Hansen D, Shneiderman B, Smith MA. Analyzing social media networks with NodeXL: insights from a connected world. Burlington, MA: Elsevier; 2011. [Google Scholar]
- 52.Jiang Y, Hesser JE. Using item response theory to analyze the relationship between health-related quality of life and health risk factors. Prev Chronic Dis. 2009 Jan;6(1):A30. Epub 2008 Dec 15. [PMC free article] [PubMed] [Google Scholar]
- 53.Stewart A, Ware JE, editors. Measuring function and well-being: the medical outcomes study approach. Durham, NC: Duke University Press; 1992. [Google Scholar]
- 54.Balon R, Beresin E. How to write a case report. In: Roberts LW, editor. The academic medicine handbook: a guide to achievement and fulfillment for academic faculty. New York, NY: Springer; 2013. http://dx.doi.org/10.1007/978-1-4614-5693-326. [Google Scholar]
- 55.Smith M, Milic-Frayling N, Shneiderman B, et al. Los Angeles, CA: Social Medica Research Foundation; 2010. NodeXL: a free and open network overview, discovery and exploration add-in for Excel 2007/2010. Available at: http://nodexl.codeplex.com/ [Google Scholar]
- 56.IBM Corp. IBM SPSS statistics for Windows, version 23.0. Armonk, NY: IBM Corp; 2015. [Google Scholar]
- 57.Rand Health. 36-item short form survey (SF-36) scoring instructions. Santa Monica, CA: Rand Corporation; 1994. [Google Scholar]
- 58.Maric M, de Haan E, Hogendoom SM, et al. Evaluating statistical and clinical significance of intervention effects in single-case experimental designs: an SPSS method to analyze univariate data. Behav Ther. 2015 Mar;46(2):230–41. doi: 10.1016/j.beth.2014.09.005. Epub 2014 Sep 19. http://dx.doi.org/10.1016/j.beth.2014.09.005. [DOI] [PubMed] [Google Scholar]
- 59.Rubin A. Statistics for evidence-based practice and evaluation. 3. Boston, MA: Cengage Learning; 2012. [Google Scholar]
- 60.Health Reform Minnesota. About us. Minneapolis, MN: State of Minnesota; 2016. Available at: http://www.dhs.state.mn.us/main/idcplg?IdcService=GET_DYNAMIC_CONVERSION&RevisionSelectionMethod=LatestReleased&dDocName=SIM_About_Us. [Google Scholar]
- 61.Conway P, Favet H, Johnston M. Collaborating on mental health: patient outcomes improved by creative partnership. Minnesota Physician. 2014 May;XXVIII(2):22–3. 32. [Google Scholar]
- 62.Institute of Medicine. Improving the quality of health care for mental and substance-use conditions. Washington, DC: The National Academies Press; 2006. [PubMed] [Google Scholar]
- 63.Ely Area Community Care Team. Ely area Community Care Team (CCT): accountable community for health. St. Paul, MN: Minnesota Department of Human Services; 2016. Available at: http://www.dhs.state.mn.us/main/groups/sim/documents/pub/dhs-286866.pdf. [Google Scholar]


