Abstract
Purpose
The Mollerussa prospective cohort was created to study pre-diabetes in a population-based sample from the primary care setting in the semirural area of Pla d’Urgell in Catalonia (Spain). The aims of the study were to assess the prevalence of pre-diabetes in our population, the likelihood to develop overt diabetes over time and to identify risk factors associated with the progression of the condition.
Participants
The cohort includes 594 subjects randomly selected between March 2011 and July 2014 from our primary care population, who were older than 25 years, consented to participate and did not have a recorded diagnosis of diabetes.
Findings to date
At baseline, we performed a clinical interview to collect demographic, clinical and lifestyle (including a nutritional survey) characteristics; carotid ultrasound imaging to assess subclinical cardiovascular disease was also performed, and a blood sample was collected, with an overall <5% rate of missing data. An additional blood draw was performed 12 months after initial recruitment to reassess laboratory results in patients initially identified as having pre-diabetes, with an 89.6% retention rate. Several studies investigating various hypotheses are currently ongoing.
Future plans
All subjects recruited during the cohort creation will be followed long-term through annual extraction of data from health records stored in the electronic Clinical station in Primary Care database. The Mollerussa cohort will thus be a sound population-based sample for multiple future research projects to generate insights into the epidemiology and natural history of pre-diabetes in Spain.
Keywords: prediabetes, diabetes mellitus, primary health care, cohort study
Strengths and limitations of this study.
The Mollerusssa cohort contains data from subjects with pre-diabetes identified in a primary care setting that were collected prospectively during 12 months, minimising recall bias.
There was a potential selection bias, with higher rates for women and middle-aged among enlisted subjects than among eligible but not enlisted subjects, which will be minimised through a weighting process during the analyses.
Subjects will be followed long-term through annual extraction of data included in the individuals’ electronic medical records, a design that will minimise losses to follow-up.
The long-term follow-up will allow the accurate estimation of time trends and clinical features associated with progression from pre-diabetes to overt diabetes
A potential limitation of the long-term follow-up is that it will rely on data that may be incomplete or inconsistently measured between subjects
Introduction
According to the American Diabetes Association (ADA), diabetes is broadly classified into four categories: type 1 diabetes mellitus (T1DM), type 2 diabetes mellitus (T2DM), gestational diabetes and specific types of diabetes due to other causes.1 However, there is a group of individuals that, in spite of having higher than normal glucose levels, do not meet criteria for diabetes, a condition referred to as pre-diabetes.
There are different definitions of pre-diabetes, but the most common one, the ADA criteria, considers one of the following instances1: (a) impaired fasting plasma glucose (IFG), defined as fasting plasma glucose (FPG) between 100 and 125 mg/dL (5.6–5.9 mmol/L); or (b) impaired glucose tolerance (IGT), defined as a 2-hour plasma glucose value after a 75g oral glucose tolerance test (OGTT) between 140 and 199 mg/dL (7.8–11.0 mmol/L); or (c) glycated haemoglobin (HbA1c) levels between 5.7% and 6.4% (39–46 mmol/mol).
The prevalence of pre-diabetes varies across countries and depending on the parameter used for the estimations. Based solely on IGT, its worldwide prevalence among adults has been estimated by the International Diabetes Federation to be 6.7% in 2015, with half of them (50.1%) younger than 50 years.2 In England, solely based on HbA1c levels, the prevalence was 35.5% among the adult population in 20113; in Spain, isolated IFG and isolated IGT were present in 3.4% and 2.9%, respectively, and combined IFG–IGT in 2.2% of the adult population in 20104; and in the USA, using the ADA definition (HbA1c levels or IFG or IGT) the prevalence was as high as 38% in 2012.5
Understanding the epidemiology and natural history of pre-diabetes has become a health priority, in particular at the primary care setting, because it is a source of avoidable morbidity and mortality. First, individuals with IFG and/or IGT have a clinical phenotype that resembles patients with T2DM, as they tend to be older, have a higher body mass index (BMI), have more frequent insulin resistance and dyslipidaemia and have higher arterial blood pressure (BP) than people with normal glucose tolerance.6 Second, people with pre-diabetes are at increased risk of developing diabetes: according to the ADA, up to 70% of them will eventually develop overt diabetes7; the annual incidence of progression to diabetes is around 5%–10% depending on the population characteristics and the definition of pre-diabetes; 6%–9% in subjects with isolated IFG, 4%–6% in those with isolated IGT, up to 15%–19% among those with both IFG and IGT8 9 and subjects with HbA1c levels from 5.7% to <6.5% have a 7.5-year predicted risk of 43.1% for incident diabetes.10 Finally, individuals with pre-diabetes are at increased risk of cardiovascular disease (CVD) and premature mortality: a meta-analysis found that the risk of CVD is increased regardless of type of blood glucose assessment in comparison to subjects with normoglycaemia11; and another recent meta-analysis found that risks of all-cause and CVD mortality compared with normoglycaemic subjects were increased in individuals with pre-diabetes with ADA defined IFG, IGT or both criteria combined, although not with isolated IFG.12
Based on epidemiological and clinical evidence, it is important from a prediction and prevention perspective to target segments of the population with metabolic and cardiovascular (CV) signatures associated with an increased risk of developing diabetes and CVD.1 The Mollerussa cohort was designed to identify undiagnosed diabetes or pre-diabetes in the adult primary care population from a semirural area of Catalonia (Spain), and to further obtain extensive epidemiological, clinical (including subclinical atherosclerotic disease) and lifestyle data. In the following phases, the cohort will be run as prospective observational studies involving identified at-risk individuals to determine the progress over time regarding risk factors, incident diabetes, incidence of CV events, rates of hospitalisation and global mortality.
Cohort description
Mollerussa is a prospective observational cohort study conducted in Pla d’Urgell, a semirural area of Catalonia (Spain), among subjects from the general population with healthcare coverage from the Catalan Institute of Health (Institut Català de la Salut).
Based on an estimated prevalence of pre-diabetes in the area of Lleida of 11% (10%–19%) in 2011,13 we initially calculated that we would need a representative sample of 940 adults considering a 95% CI and a margin of error of ±2%. However, literature published after the initiation of the recruitment phase, using HbA1c levels and ADA criteria, reported pre-diabetes prevalence between 35.5% and 38%.3 5 Using this datum, a random sample of 505 subjects was sufficient to assess an estimated prevalence of about 30% with a 95% CI and a margin of error of ±4%.
Recruitment
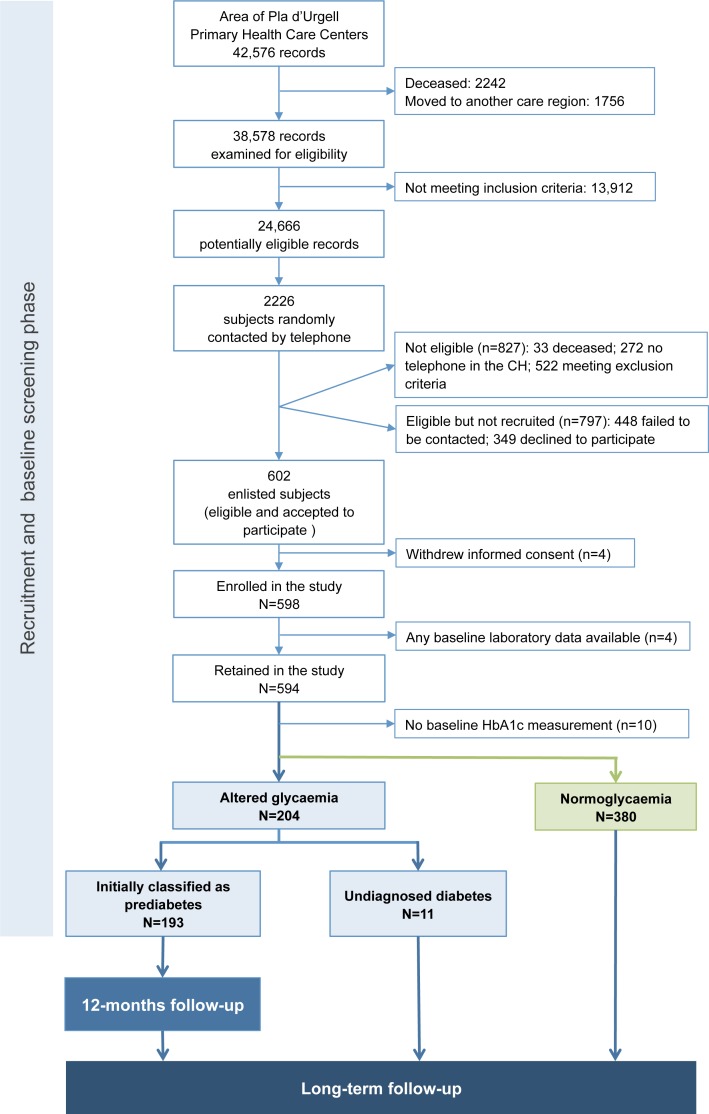
Using the electronic Clinical station in Primary Care (eCAP) health records database implemented in all primary care centres in Catalonia, a code number was given to each registered adult. During the recruitment phase, 24 666 registered health records met inclusion criteria, namely subjects older than 25 years and attending any Primary Healthcare Centre in the same health area in Pla d’Urgell (box 1; figure 1); among them, 2226 random individuals (about 5% of the total number of individuals registered at each centre) were contacted by telephone (up to three attempts) and invited to participate (figure 1). Randomisation was carried out using a randomiser programme (SPSS software V.16.0 for Windows; SPSS), following the principles of simple random sampling.
Box 1. Summary of inclusion and exclusion criteria.
Inclusion criteria
Age ≥25 years
Attended a primary health care centre in the area
Exclusion criteria
Patient information about having diabetes provided in the first contact or existing ICD-10 code of diabetes (E11, E14 or E13) registered by a physician or confirmed based on clinical data:
HbA1c ≥6.5%
IGT: 2-hour plasma glucose in the 75g OGTT ≥200 mg/dL (11.1 mmol/L)
IFG: FPG ≥126 mg/dL (7 mmol/L)
Specific subtypes of diabetes other than T1DM and T2DM:
Gestational diabetes
Genetic defect of beta-cell action
Genetic defect in insulin action
Diseases of the exocrine pancreas (eg, pancreatitis, haemochromatosis, pancreatic cancer, cystic fibrosis)
Endocrinopathies (eg, Cushing’s syndrome, glucagonoma, somatostatinoma, hyperthyroidism, pheochromocytoma, acromegaly)
Chemical-induced diabetes
Diabetes secondary to infections
Autoimmune diabetes
Use of oral antidiabetic drugs: metformin, dipeptidyl peptidase-4 inhibitors, sulfonylureas and glitazones
Presence of cardiovascular disease:
Previous hospitalisation to treat heart disease
Heart failure
Left bundle branch block or second degree atrioventricular block
Aortic stenosis
Systolic BP >180 mm Hg or diastolic BP >105 mm Hg
Cancer treated in the preceding 5 years, except non-melanoma skin cancers (basal-cell and squamous-cell carcinoma)
Kidney disease, defined as plasma creatinine ≥1.4 mg/dL in men and ≥1.3 mg/dL in women or proteinuria >2+
Anaemia, defined as haematocrit <36% in men and <33% in women
Hepatitis, defined as transaminases more than 10 times the upper the limit of normal
Gastrointestinal diseases (pancreatitis, irritable bowel disease and inflammatory bowel disease)
Recent abdominal surgery
Chronic pulmonary obstructive disease requiring domiciliary oxygen therapy
Chronic infectious diseases (eg, HIV, active tuberculosis, HBV and HCV)
Use of systemic glucocorticoids or beta blockers
Major psychiatric disorder with psychotic symptoms
BP, blood pressure; FPG, fasting plasma glucose; HbA1c, glycated haemoglobin; HBV, hepatitis B virus; HCV, hepatitis C virus; ICD, International Classification of Diseases; IFG, impaired fasting plasma glucose; IGT, impaired glucose tolerance; OGGT, oral glucose tolerance test; T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus.
Figure 1.
Mollerussa study flow chart. CH, clinical history; HbA1c, glycated haemoglobin.
Main exclusion criteria (box 1) included a previous diagnosis of diabetes (T1DM, T2DM and any specific subtype of diabetes), and subjects on treatment with oral antidiabetic drugs to avoid the inclusion of individuals with actual diabetes but optimal glycaemic control, or even without diabetes but using metformin as treatment for other conditions. Based on their willingness to join the study and exclusion criteria, a total of 602 subjects were recruited and subsequently invited for an appointment, of whom four withdrew consent and, for four, we did not obtain any baseline laboratory data, therefore giving a final study population of 594 subjects.
Data collection
The research plan included a first phase involving two visits to the primary healthcare centre for baseline screening, a second phase conducted 12 months after the baseline visits and a third phase of long-term follow-up of the cohort.
First phase or baseline screening
The following variables were collected/explored by trained research staff in the first visit to the subject’s primary healthcare centre: (a) Sociodemographic variables: age; gender; education level according to the International Standard Classification of Education14; sector of working activity (primary, secondary or manufacturing, tertiary or services); self-perceived work activity (minimum, light, moderate, heavy); report on physical activity according to the Spanish-validated International Physical Activity Questionnaire15; family history of hypertension, dyslipidaemia, hypertriglyceridaemia, diabetes mellitus and acute myocardial infarction or angina pectoris; personal history of hypertension, dyslipidaemia, hypertriglyceridaemia, alcohol consumption and smoking habit as reported by the patient; and current medication. (b) Anthropometric measures and physical examination: BP recorded according to the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure guidelines16; heart rate; body weight; waist circumference; and calculation of BMI. (c) Nutritional survey: food intake was assessed using a Spanish-validated version of the semiquantitative Food Frequency Qquestionnaire17; and we estimated the degree of adherence to the traditional Mediterranean diet through the Mediterranean Diet score.18 (d) Carotid ultrasound imaging to measure intima-medial thickness and to assess the presence of carotid atherosclerotic plaques as previously described.19 Briefly, both carotids were examined following a standardised operational procedure and the Mannheim consensus,20 consisting of a cross-sectional view of the common, bulb and internal segments of the carotid arteries to identify atherosclerotic plaques (defined as a focal encroachment into the lumen of the carotid), and an online average measurement of the carotid intima-media thickness (c-IMT) of these three areas, with values of c-IMT above 1.5 mm considered as plaques.21
In a second appointment, the following laboratory measurements were obtained in fasting conditions: complete blood count, lipid, liver, kidney and thyroid profile. The study of glycaemia included the measurement of FPG and HbA1c. According to the ADA HbA1c criteria,1patients were classified into three groups: (1) without glucose metabolism disorders (HbA1c <5.7%), (2) with pre-diabetes (HbA1c between 5.7% and 6.4%) or with undiagnosed diabetes (HbA1c ≥6.5%). When the investigator detected a case of undiagnosed diabetes, the individual was re-contacted and advised to visit a general practitioner at his/her corresponding primary healthcare centre.
The baseline assessment will allow a first estimation of the prevalence of pre-diabetes in our population, its associated factors, and whether these subjects also have a higher prevalence of subclinical carotid atheroscleroses (and are therefore at high risk of CVD) compared with normoglycaemic subjects. Moreover, it will build on previous estimates of the prevalence of undiagnosed diabetes in primary healthcare in Catalonia.22
Second phase or short-term follow-up
Twelve months after the baseline visits, subjects initially fulfilling pre-diabetes criterion underwent a second visit to perform another blood draw to reassess the laboratory results. This was based on the ADA recommendation to repeat testing in the absence of unequivocal hyperglycaemia.1 Based on re-evaluated HbA1c levels, those subjects with HbA1c levels between 5.7% and 6.4% were confirmed as pre-diabetes; those with a subsequent increase from pre-diabetes values at baseline to HbA1c ≥6.5% after 12 months were considered as incident diabetes (and as well re-contacted and advised to visit a general practitioner); and those with a further decrease from pre-diabetes values at baseline to HbA1c <5.7% after 12 months as regression to normoglycaemia, although they will be followed up to rule out a temporary improvement, and thus a false case of regression to normal mean HbA1c values.
The 12-month follow-up will give a real estimation of pre-diabetes prevalence, valuable information on the 1-year probability of progression to diabetes and which risk factors were relevant to the further development of the disease (eg, metabolic traits and lifestyle).
Third phase or long-term follow-up
In addition to the 12-month follow-up, we also plan to follow all subjects enrolled in the Mollerussa cohort annually through cross-sectional extraction of data stored in the primary care electronic medical records of the eCAP database.23 This is based on the ADA recommendation to follow pre-diabetes in asymptomatic adults yearly.1 We will extract data for the following variables: any diagnosis of T2DM (International Classification of Disease (ICD-10) codes E11 or E14)22; time since diagnosis; estimated glomerular filtration rate using the Modified Diet in Renal Disease formula; standardised HbA1c values, using the most recent value of the preceding 12 months; presence of CVD, including coronary artery disease (ICD-10 codes I20, I21, I22, I23 or I24), stroke (ICD-10 codes I63, I64, G45 or G46) and peripheral artery disease (ICD-10 code I73.9); risk factors, including BMI (most recent value in the last 12 months), cholesterol levels (total, low-density lipoproteins or LDL-cholesterol and high-density lipoproteins or HDL-cholesterol; most recent value in the last 12 months), BP (systolic and diastolic mean value in the last 12 months); and data on prescribed glucose-lowering, lipid-lowering, antihypertensive and antithrombotic medications. This information will be supplemented with data registered in the Conjunto Mínimo Básico de Datos de Altas Hospitalarias (Set of Minimum Basic Data Set of Hospital Admissions),24 which records all admissions to public and private hospitals in the region and contains information on diagnostics, procedures and discharge reports.
With this additional longitudinal approach, we will be able to obtain the patient’s data on progression to overt diabetes and/or initiation of antidiabetic treatment over time (if directly related to diabetes). This is important because besides the annualised incidence rate of progression to diabetes, the time course progression of dysglycaemia has not been studied at large. From the few available studies, the mode of onset of diabetes in subjects with pre-diabetes follows a non-linear pattern, with a rapid rather than gradual onset of diabetes over a 3-year time.25 Moreover, we will be able to obtain data on the incidence of other diabetes-associated chronic conditions also present at the pre-diabetes stages, such as nephropathy, neuropathy or retinopathy; the incidence of macrovascular complications over time; the likelihood of initiation of hypoglycaemic agents among progressors; rates and cause of hospitalisations; and overall mortality.
This study was approved by the Ethics Committee of the Primary Healthcare University Research Institute (Institut d'Investigació en Atenció Primària, IDIAP) Jordi Gol (P12/043), and all patients signed a written informed consent form prior to participation. The study was conducted in accordance with the Declaration of Helsinki (1964).
Findings to date
The Mollerussa study completed its recruitment phase between August 2011 and July 2014, and the 12-month short-term follow-up in July 2015. The enlisted sample (n=602) was different from the eligible but not enlisted population (n=784) in terms of gender and age (table 1); the enlisted sample had a significantly higher proportion of women (58.6% vs 44.0%; p<0.001), and was older (mean age 48.1 years vs 45.7 years; p<0.001).
Table 1.
Age and gender characteristics between subjects eligible but not enlisted and subjects eventually enlisted in the Mollerussa cohort
| Eligible but not enlisted | Enlisted (n=602) |
|||
| Failed to be contacted (n=448) |
Declined to participate (n=349) |
All (n=797) |
||
| Gender (female), n (%) | 181 (40.4) | 170 (48.7) | 351 (44.0) | 353 (58.6)* |
| Age, years, mean (SD) | 44 (15.0) | 47.9 (16.3) | 45.7 (15.7) | 48.1 (13.4)† |
| Age group, years, n (%) | ||||
| <40 | 218 (48.7) | 140 (40.1) | 358 (44.9) | 168 (28.2) |
| 40–60 | 160 (35.7) | 125 (35.8) | 285 (35.8) | 315 (52.9) |
| >60 | 70 (15.6) | 84 (24.1) | 154 (19.3) | 113 (19.0) |
*χ2 test, p<0.001.
†Kruskal-Wallis non-parametric test, p<0.001.
Demographic characteristics of participants who provided a blood sample during the first phase (baseline visit) are summarised in table 2.
Table 2.
Demographic characteristics of study population enrolled in the Mollerussa cohort
| Characteristic | Total valid N | Statistic |
| Gender, women, n (%) | 594 | 347 (58.4) |
| Age, years, mean (SD) | 594 | 50.6 (13.3) |
| Weight, kg, mean (SD) | 574 | 73.1 (14.5) |
| Waist, cm, mean (SD) | 573 | 94.2 (12.5) |
| Body mass index, kg/m2, mean (SD) | 573 | 26.3 (4.7) |
| <25.0, n (%) | 236 (41.2) | |
| 25.0–29.9, n (%) | 235 (41.0) | |
| ≥30.0, n (%) | 102 (17.8) | |
| Education level, n (%) | 575 | |
| Not even primary school | 24 (4.2) | |
| Completed primary school | 122 (21.2) | |
| Secondary/high school | 366 (63.7) | |
| Graduate or higher | 63 (11) | |
| Work activity, n (%) | 572 | |
| Employed | 393 (68.7) | |
| Unemployed | 65 (11.4) | |
| Disability | 12 (2.1) | |
| Retired | 102 (17.8) | |
| Hypertension, n (%) | 571 | 102 (17.9) |
| Dyslipidaemia, n (%) | 571 | 131 (22.9) |
| Hypertriglyceridaemia, n (%) | 554 | 22 (4.0) |
| Smokers, n (%) | 594 | |
| Current | 152 (25.6) | |
| Former | 148 (24.9) | |
| Alcohol consumption, n (%) | 573 | 286 (49.9) |
After the first phase, the rate of missing data was less than 5% across variables of interest (table 3), which is far below the 20% maximum recommended lost to follow-up rate in a cohort study.26 Twelve months after the baseline screening, we obtained a second blood draw from 89.6% of subjects found to have altered glycaemia levels at baseline (n=193 excluding undiagnosed diabetes), a retention rate also indicating acceptable validity of the results (table 3; figure 1).
Table 3.
Summary of missing data for variables recorded during the first and second phase of the Mollerussa cohort
| Variable of interest | Missing data, n (%) |
| First phase (baseline screening); n=594 | |
| No clinical interview | 17 (2.9) |
| No nutritional survey | 28 (4.7) |
| No carotid echography | 17 (2.9) |
| No laboratory results | 0 (0.0) |
| No HbA1c measurement | 10 (1.7) |
| No sample for biobank | 22 (3.7) |
| Second phase (12 months follow-up); n=193 | |
| No laboratory results | 20 (10.4) |
HbA1c, glycated haemoglobin.
We are currently in the phase of longitudinal follow-up of all subjects with subjects identified during the first and second phase (figure 1), and developing protocols for the analyses to explore hypotheses on different features of the epidemiology and natural history of pre-diabetes in our primary care setting. The first paper from the Mollerussa project (now in preparation) will describe results derived from the short-term follow-up of the cohort, namely the prevalence of pre-diabetes and undiagnosed diabetes, the clinical and demographic profile of patients with pre-diabetes versus those with normal glycaemic levels, a first estimation of the annual incidence of overt diabetes among subjects with pre-diabetes and the metabolic, CV and lifestyle disease-associated conditions.
Strengths and limitations
The main strength of the Mollerussa cohort is that it includes adult patients from primary care health centres prospectively collected, and the opportunity to follow participants in the long term through healthcare electronic registries, which ensures that it will be of use for multiple future research projects. The combined short-term prospective and long-term longitudinal design has both advantages and limitations.
The prospective phase (baseline screening and 12-month short-term follow-up) prevents recall bias because the risk for diabetes was assessed before the onset of the disease, and the measurement of events in a temporal sequence allows for causes to be distinguished from effects. However, we must acknowledge a potential selection bias, since we had higher rates of women and middle-aged subjects among enlisted people than among eligible but not enlisted subjects. The influence of this potential bias will be minimised through a weighting process on the prevalence estimates, although how this original unbalance may impact the results is not clear, because IFG and HbA1c detect different categories of individuals as being at risk: IFG is substantially more common among men, and its prevalence tends to plateau in middle age, while the prevalence of pre-diabetes using HbA1c increases with age (maximum peak in those aged 60–74 years) but does not differ by gender.27 28 Finally, we did not perform an OGTT among enrolled individuals. Although IGT is more common than IFG in most populations, it is more sensitive but slightly less specific for identifying people who will develop diabetes.29 Additionally, the OGTT has low reproducibility and it is inconvenient in terms of costs and time consumption.30 Conversely, HbA1c measurement is cost-effective and improves the sensitivity of FPG in the detection of early T2DM in high-risk individuals.28 31
On the other hand, the longitudinal, long-term phase has the advantage that cohort membership is not dependent on continuing to visit the practice from which the members were recruited. While the main strength is that this will minimise losses to follow-up, the primary limitation is that it will rely on data that may be incomplete or inconsistently measured between subjects. An additional advantage of this design is that, since the latency from pre-diabetes to overt diabetes may be longer than the initial 12 months follow-up,25 the long-term follow-up will allow a more accurate estimation of the time trends (cumulative incidences) and clinical features associated with progression to diabetes.
Collaboration
The Mollerussa study is open to future joint studies with external study groups. Investigators with an interest in hypotheses related to pre-diabetes are welcome to contact a member of the Institut Universitari d’Investigació en Atenció Primària Jordi Gol (IDIAP Jordi Gol) to submit a joint study proposal to the Scientific Committee of the institution. The group will consider these proposals if they are in accordance with the study objectives, and do not overlap with other studies already under way. If accepted, a formal written agreement will be established with the collaborative group.
Acknowledgments
We acknowledge Mònica Gratacòs and Amanda Prowse for providing support in the manuscript preparation and editing. CIBER of Diabetes and Associated Metabolic Diseases is an initiative from Instituto de Salud Carlos III (Plan Nacional de I+D+I and Fondo Europeo de Desarrollo Regional).
Footnotes
Contributors: MF, JRM and DM conceived and designed the study; MBV, JF-N, and AM participated in the study design; MBV, MF, ER, NA, MG-C, NM and AM collected the data; EC built and managed the database; JRM managed the database, contributed to data cleaning, performed the statistical analyses and contributed to interpretation of the data; MBV, DM, JF-N and MM-C wrote the manuscript. All authors critically reviewed the manuscript and approved the final version to be published.
Funding: This study was funded by Institut Universitari d’Investigació en Atenció Primària Jordi Gol (IDIAP Jordi Gol). The funding source had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; or preparation, review or approval of the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: Ethics Committee of the Primary Health Care University Research Institute (IDIAP) Jordi Gol (P12/043).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: This article describes the establishment of a longitudinal cohort and early findings, and full results will be submitted for peer-reviewed publication in due course. The authors are willing to share unpublished data with interested parties upon request because they contain identifying human information and are unsuitable for public deposition. Requests may be made to the corresponding author (didacmauricio@gmail.com).
Correction notice: This paper has been amended since it was published Online First. Owing to a scripting error, some of the publisher names in the references were replaced with 'BMJ Publishing Group'. This only affected the full text version, not the PDF. We have since corrected theseerrors and the correct publishers have been inserted into the references.
References
- 1. ADA. American Diabetes Association. 2. classification and diagnosis of diabetes. Diabetes Care 2016;39:S13–S22. [DOI] [PubMed] [Google Scholar]
- 2. IDF. International Diabetes Federation Diabetes Atlas. 7th ed, 2015. http://www.diabetesatlas.org/ (accessed Sept 2016).
- 3. Mainous AG, Tanner RJ, Baker R, et al. . Prevalence of prediabetes in England from 2003 to 2011: population-based, cross-sectional study. BMJ Open 2014;4:e005002 10.1136/bmjopen-2014-005002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Soriguer F, Goday A, Bosch-Comas A, et al. . Prevalence of diabetes mellitus and impaired glucose regulation in Spain: the Di@bet.es Study. Diabetologia 2012;55:88–93. 10.1007/s00125-011-2336-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Menke A, Casagrande S, Geiss L, et al. . Prevalence of and trends in diabetes among adults in the United States, 1988-2012. JAMA 2015;314:1021–9. 10.1001/jama.2015.10029 [DOI] [PubMed] [Google Scholar]
- 6. Ferrannini E. Definition of intervention points in prediabetes. Lancet Diabetes Endocrinol 2014;2:667–75. 10.1016/S2213-8587(13)70175-X [DOI] [PubMed] [Google Scholar]
- 7. Nathan DM, Davidson MB, DeFronzo RA, et al. . Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care 2007;30:753–9. 10.2337/dc07-9920 [DOI] [PubMed] [Google Scholar]
- 8. Gerstein HC, Santaguida P, Raina P, et al. . Annual incidence and relative risk of diabetes in people with various categories of dysglycemia: a systematic overview and meta-analysis of prospective studies. Diabetes Res Clin Pract 2007;78:305–12. 10.1016/j.diabres.2007.05.004 [DOI] [PubMed] [Google Scholar]
- 9. Tabák AG, Herder C, Rathmann W, et al. . Prediabetes: a high-risk state for diabetes development. Lancet 2012;379:2279–90. 10.1016/S0140-6736(12)60283-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ackermann RT, Cheng YJ, Williamson DF, et al. . Identifying adults at high risk for diabetes and cardiovascular disease using hemoglobin A1c National Health and Nutrition Examination Survey 2005-2006. Am J Prev Med 2011;40:11–17. 10.1016/j.amepre.2010.09.022 [DOI] [PubMed] [Google Scholar]
- 11. Levitan EB, Song Y, Ford ES, et al. . Is nondiabetic hyperglycemia a risk factor for cardiovascular disease? A meta-analysis of prospective studies. Arch Intern Med 2004;164:2147–55. 10.1001/archinte.164.19.2147 [DOI] [PubMed] [Google Scholar]
- 12. Huang Y, Cai X, Chen P, et al. . Associations of prediabetes with all-cause and cardiovascular mortality: a meta-analysis. Ann Med 2014;46:684–92. 10.3109/07853890.2014.955051 [DOI] [PubMed] [Google Scholar]
- 13. Sánchez V. El sínfrome metabólico en Lleida desde Una perspectiva clínico-epidemiológica. Department of Medicine, University of Lleida, 2011. Doctoral thesis https://repositori.udl.cat/handle/10803/31999?show=full (accessed 08 Oct 2016). [Google Scholar]
- 14. ISCED. OECD/Eurostat/UNESCO Institute for Statistics ISCED 2011 Operational Manual: guidelines for Classifying National Education Programmes and Related Qualifications. Paris: OECD Publishing, 2011. [Google Scholar]
- 15. Roman-Viñas B, Serra-Majem L, Hagströmer M, et al. . International physical activity questionnaire: reliability and validity in a spanish population. Eur J Sport Sci 2010;10:297–304. 10.1080/17461390903426667 [DOI] [Google Scholar]
- 16. Chobanian AV, Bakris GL, Black HR, et al. . The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA 2003;289:2560–72. 10.1001/jama.289.19.2560 [DOI] [PubMed] [Google Scholar]
- 17. Vioque J. Validez de la evaluación de la ingesta dietética : Serra Majem L, Aranceta Bartrina J, Nutrición Y Salud Pública. Métodos, bases científicas y aplicaciones. 2nd ed Barcelona: Masson-Elsevier, 2006:199–220. [Google Scholar]
- 18. Trichopoulou A, Costacou T, Bamia C, et al. . Adherence to a mediterranean diet and survival in a Greek population. N Engl J Med 2003;348:2599–608. 10.1056/NEJMoa025039 [DOI] [PubMed] [Google Scholar]
- 19. Rubinat E, Marsal JR, Vidal T, et al. . Subclinical carotid atherosclerosis in asymptomatic subjects with type 2 diabetes mellitus. J Cardiovasc Nurs 2016;31:E1–E7. 10.1097/JCN.0000000000000236 [DOI] [PubMed] [Google Scholar]
- 20. Touboul PJ, Hennerici MG, Meairs S, et al. . Mannheim carotid intima-media thickness consensus (2004-2006). An update on behalf of the advisory board of the 3rd and 4th watching the risk Symposium, 13th and 15th European Stroke Conferences, Mannheim, Germany, 2004, and Brussels, Belgium, 2006. Cerebrovasc Dis 2007;23:75–80. 10.1159/000097034 [DOI] [PubMed] [Google Scholar]
- 21. Karim R, Hodis HN, Detrano R, et al. . Relation of Framingham risk score to subclinical atherosclerosis evaluated across three arterial sites. Am J Cardiol 2008;102:825–30. 10.1016/j.amjcard.2008.05.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mata-Cases M, Mauricio D, Real J, et al. . Is diabetes mellitus correctly registered and classified in primary care? A population-based study in Catalonia, Spain. Endocrinol Nutr 2016;63:440–8. 10.1016/j.endonu.2016.07.004 [DOI] [PubMed] [Google Scholar]
- 23. Bolíbar B, Fina Avilés F, Morros R, et al. . [SIDIAP database: electronic clinical records in primary care as a source of information for epidemiologic research]. Med Clin 2012;138:617–21. [DOI] [PubMed] [Google Scholar]
- 24. Generalitat de Catalunya Servei Català de la Salut. Registre del conjunt mínim bàsic de dades dels hospitals d'aguts (CMBD-HA.) Especificacions de la validació de les dades, 2010. http://www20.gencat.cat/ (accessed 07 Oct 2016).
- 25. Nichols GA, Hillier TA, Brown JB. Progression from newly acquired impaired fasting glusose to type 2 diabetes. Diabetes Care 2007;30:228–33. 10.2337/dc06-1392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Song JW, Chung KC. Observational studies: cohort and case-control studies. Plast Reconstr Surg 2010;126:2234–42. 10.1097/PRS.0b013e3181f44abc [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mann DM, Carson AP, Shimbo D, et al. . Impact of A1C screening criterion on the diagnosis of pre-diabetes among U.S. adults. Diabetes Care 2010;33:2190–5. 10.2337/dc10-0752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Droumaguet C, Balkau B, Simon D, et al. . Use of HbA1c in predicting progression to diabetes in French men and women: data from an Epidemiological Study on the Insulin Resistance Syndrome (DESIR). Diabetes Care 2006;29:1619–25. 10.2337/dc05-2525 [DOI] [PubMed] [Google Scholar]
- 29. Unwin N, Shaw J, Zimmet P, et al. . Impaired glucose tolerance and impaired fasting glycaemia: the current status on definition and intervention. Diabet Med 2002;19:708–23. [DOI] [PubMed] [Google Scholar]
- 30. Gossain VV, Aldasouqi S. The challenge of undiagnosed pre-diabetes, diabetes and associated cardiovascular disease. Int J Diabetes Mellit 2010;2:43–6. 10.1016/j.ijdm.2009.10.004 [DOI] [Google Scholar]
- 31. Perry RC, Shankar RR, Fineberg N, et al. . HbA1c measurement improves the detection of type 2 diabetes in high-risk individuals with nondiagnostic levels of fasting plasma glucose: the Early Diabetes Intervention Program (EDIP). Diabetes Care 2001;24:465–71. 10.2337/diacare.24.3.465 [DOI] [PubMed] [Google Scholar]