Abstract
Background:
Treatment decisions in multiple sclerosis (MS) are affected by many factors and are made by the patient, doctor, or both. With new disease-modifying therapies (DMTs) emerging, the complexity surrounding treatment decisions is increasing, further emphasizing the importance of understanding decision-making preferences.
Methods:
North American Research Committee on Multiple Sclerosis (NARCOMS) Registry participants completed the Fall 2014 Update survey, which included the Control Preferences Scale (CPS). The CPS consists of five images showing different patient/doctor roles in treatment decision making. The images were collapsed to three categories: patient-centered, shared, and physician-centered decision-making preferences. Associations between decision-making preferences and demographic and clinical factors were evaluated using multivariable logistic regression.
Results:
Of 7009 participants, 79.3% were women and 93.5% were white (mean [SD] age, 57.6 [10.3] years); 56.7% reported a history of relapses. Patient-centered decision making was most commonly preferred by participants (47.9%), followed by shared decision making (SDM; 42.8%). SDM preference was higher for women and those taking DMTs and increased with age and disease duration (all P < .05). Patient-centered decisions were most common for respondents not taking a DMT at the time of the survey and were preferred by those who had no DMT history compared with those who had previously taken a DMT (P < .0001). There was no difference in SDM preference by current MS disease course after adjusting for other disease-related factors.
Conclusions:
Responders reported most commonly considering their doctor's opinion before making a treatment decision and making decisions jointly with their doctor. DMT use, gender, and age were associated with decision-making preference.
Treatment decisions for people with multiple sclerosis (MS) are complex and can involve both medical and personal considerations. Disease history, previous treatments, health-care delivery, current disability status, risk tolerance, and potential adverse effects or events are just some of the many considerations that can affect a treatment choice. There is a wide range of treatment options for those with relapsing MS, and, with new disease-modifying therapies (DMTs) continuing to emerge, the process of selecting the appropriate therapy involves taking multiple factors into account. Shared decision making (SDM) is a collaborative process for making treatment decisions that involves the patient and his or her health-care providers.1,2 Research in multiple disease areas has shown that increased patient participation in decision making has resulted in better treatment compliance and patient satisfaction outcomes.3 In communicating the risks and expected outcomes of the multiple possible DMT choices, clinicians and other health-care providers should account for the patient's values and preferences in the decision-making process.3
Most SDM research in MS has focused on decisions and interventions in the clinical setting3–6 and how to increase patient engagement in the decision.7,8 According to Elwyn and colleagues,9 at least three conditions are required for SDM to become part of mainstream clinical practice: 1) access to evidence-based information about treatment options, 2) guidance on how to balance the risks and benefits of different options, and 3) an understanding by health-care providers that facilitates patient engagement. These factors are associated with the health literacy of the patient, the desired level of patient autonomy by both the patient and the health-care provider, and the patient's willingness to accept risk (ie, risk tolerance). Literacy, risk tolerance, and autonomy with decision making can vary with age, race, sex, and disability level.10 Previous research using the North American Research Committee on Multiple Sclerosis (NARCOMS) Registry data has shown a high level (75%–81%) of health literacy in people with MS.11 Fox and colleagues12 found that although most patients accept at least some therapy-related risk, up to 23% are not willing to accept any risk associated with therapy. Reasons for choosing or changing DMTs for MS may be affected by demographic and disease characteristics as well as financial considerations. Recent studies have shown that although treatment switches were initiated nearly equally by patients and physicians, the primary reason for selecting a new therapy was most commonly the physician recommendation.13
The Control Preferences Scale (CPS) assesses how much decision-making control a patient prefers. The CPS is easily administered, is valid in health-care decision making,14 and has been used across varying disease types.15–18 In addition, it has been adapted for self-administration without the need for detailed instructions19 using a 5-point visual scale (Figure 1). Research using the CPS in MS has shown high levels of autonomy in decision making and role preference variations with age, sex, and disease course.4,19 However, the previous studies had only a limited ability to investigate the impact of these characteristics on autonomy. Therefore, we used the CPS to examine and better understand the role preferences in a large, demographically diverse cohort of individuals with MS in the NARCOMS Registry.
Figure 1.
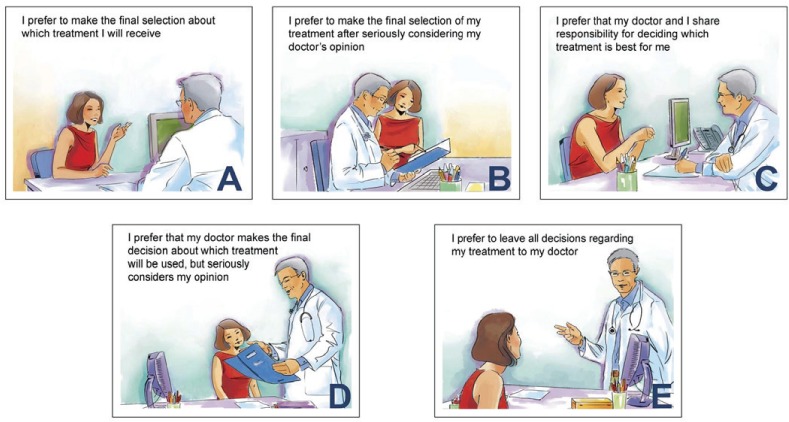
Control Preferences Scale
A–E, defined as shown. © Solari A, Giordano A, Kasper J, et al. Role preferences of people with multiple sclerosis: image-revised, computerized self-administered version of the Control Preference Scale. PLoS One. 8(6):e6612719 (https://doi.org/10.1371/journal.pone.0066127).
Methods
NARCOMS Registry
The NARCOMS Registry is a voluntary longitudinal registry capturing health-related information from adults (≥18 years) with MS. Registry participants complete an enrollment questionnaire, followed by semiannual update surveys submitted either online or by mail according to participant preference. All data used in this study were self-reported and de-identified before analysis. Participants' consent was obtained for all surveys; this study was approved by the institutional review board at The University of Alabama at Birmingham. The present study involved Registry participants who completed the Fall 2014 Update survey.
Clinical and Demographic Characteristics
Sociodemographic Characteristics and Location of Care
Education was included as a measure of socioeconomic status, with categories of less than 12 years, high school diploma, associate's degree, technical degree, bachelor's degree, and postgraduate degree. Health insurance status was captured as the current insurance at the time of the survey (yes/no). Current employment status was captured as yes, full-time; yes, part-time; and no (not working). The location where or doctor from whom participants receive most of their MS care was captured as specialized MS center, private neurologist, general practitioner, other, and “I do not receive care for my MS.” For this analysis, “other” and “I do not receive care” were combined into a single group owing to their small cell size.
MS Course, Treatment, and Disability
Current type (course) of MS was self-reported from the following options: clinically isolated syndrome, relapsing-remitting MS, secondary progressive MS, primary progressive MS, progressive relapsing MS, do not know, and other. Disability level was assessed using the Patient-Determined Disease Steps (PDDS) scale, which is a validated measure of self-reported disability that correlates highly with the physician-scored Expanded Disability Status Scale (EDSS).20,21 The PDDS scale is scored from 0 (normal) to 8 (bedridden), where a score of 0 approximates an EDSS score of 0, a score of 3 represents early gait disability not requiring an assistive device and approximates an EDSS score of 4.0 to 4.5, and scores of 4, 5, and 6 represent EDSS scores of 6 to 6.5, requiring an assistive device. Participants were also asked whether they had ever used a DMT before enrollment in the NARCOMS Registry (ever/never), had used a DMT in the past 6 months (yes/no), or had a change to their DMT in the past 6 months (including stopping, starting, drug holiday, adding, or change in dosing).
Symptom Tracking
Participants were asked to report how they tracked their symptoms and any related changes by selecting all that applied from the following options: My doctor tracks my symptoms (MD); I keep copies of my medical records; I keep a handwritten/paper diary; I use an MS-specific application (app); I use a non-MS electronic diary or app; and I use the NARCOMS Registry PDDS scale or Performance Scales. The last five options were considered self-tracking methods. For analysis, responses were categorized into four groups: did not answer, MD only (selected MD and no self-tracking), track own only (selected only self-tracking options), or track own + MD (selected MD and at least one of the self-tracking options).
CPS Administration
Full electronic administration of the CPS requires a monitor measuring 15 inches or larger, with multiple iterations of the presentation and selection of CPS cartoons (Figure 1). However, to promote inclusiveness there are no requirements for screen size for participation in the NARCOMS Registry. Furthermore, mail survey responders were not able to participate in an iterative assessment. Therefore, in this study, Registry participants were asked to select a single cartoon frame by letter (A–E), as shown in Figure 1, to answer the following question: “Considering how you interact with the physician who treats your MS, what is the most accurate letter from the pictures below that shows how you make decisions about your DMT treatment (including not taking any DMT treatment)?” The response options range from the individual making their own treatment decisions through joint decisions between the individual and the physician to the physician making treatment decisions.
Statistical Analysis
For inclusion in this analysis, respondents to the Fall 2014 survey had to report a current DMT status (yes/no), indicate whether they had any changes to DMT use in the previous 6 months (yes/no), and complete the CPS. To reflect the lack of DMT options for non-relapsing types of MS, it was necessary to investigate how a preference for autonomy might be affected by MS courses that involved relapses and those that had no history of relapses. Current type (course) of MS was thus categorized as 1) relapsing, including relapsing-remitting MS, secondary progressive MS (with history of relapse), progressive relapsing MS, or reporting a relapse in the previous 6 months; 2) progressive, including primary progressive MS (no report of relapse in the previous 6 months); or 3) other, including responders who did not know their current course (with no relapse history) or did not answer the question. The PDDS scale scores were collapsed into groups based on level of disability and use of assistive devices: normal (0), mild/moderate (1 and 2), gait disability (3), early/late cane (4 and 5), and bilateral support, wheelchair/scooter, bedridden (6, 7, and 8).
Descriptive measures are presented as number (percentage) or mean (SD), as applicable. Group comparisons were made for categorical outcomes using the likelihood ratio, χ2 test, or Fisher exact test and for continuous outcomes using analysis of variance or Wilcoxon tests, as applicable. Nominal logistic regression models were used to determine associations between CPS selection and current PDDS scale score (in groups), current employment, current health insurance status, current DMT use, relapse in the previous 6 months, gender, age at survey, disease duration at survey, relapse ever at enrollment, and DMT ever at enrollment. The CPS was administered as described previously herein, and responses were collapsed into three groups to minimize the number of regression models conducted.22 Responses A and B were considered patient-centered decisions (CPS A+B), response C was considered a shared decision (CPS C), and responses D and E were considered physician-centered decisions (CPS D+E). Covariates were selected based on association shown in previous research or found in unadjusted analyses of the CPS. Statistical analyses were performed using SAS version 9.4 and JMP Pro version 12 (SAS Institute Inc, Cary, NC); P ≤ .05 was considered significant.
Results
Participant Characteristics
Of the 12,482 participants invited to complete the NARCOMS Registry Fall 2014 Update survey, 7601 (60.9%) responded. A total of 7009 respondents (92.2%) completed both the DMT and CPS questions and were included in this analysis (Table 1). Non-responders to the Fall 2014 survey were similar to the analysis group with respect to age at diagnosis, gender, and disability level at enrollment in the NARCOMS Registry but were slightly less likely to be white or married or have relapsing disease (data not shown). Of the 7009 participants, 2160 (30.8%) completed the CPS via the paper survey, and 4849 (69.2%) completed the CPS via the online survey. Most respondents were women (79.3%) and white (93.5%) and had a mean (SD) age of 57.6 (10.3) years at the time of the survey and 39.0 (9.7) years at diagnosis. Almost all responders reported having health insurance in the previous 6 months (99.0%), with most receiving care either from a private neurologist (55.7%) or at a specialized MS center (29.9%). Most responders were not employed (67.9%), and 22.4% were employed full-time. Characteristics by CPS selection are given in Supplementary Table 1 (379.4KB, pdf) , which is published in the online version of this article at ijmsc.org.
Table 1.
Demographic and clinical characteristics of responders overall and by symptom tracking
DMT Use
Most respondents reported DMT use in the previous 6 months (65.9%), and, of these, 1148 (24.9%) reported a change in their DMT status during the same period. The most common change was a switch in DMT (40.8%), followed by a change in dose of the same DMT (28.8%), stopping of all DMTs (18.6%), an interruption in DMT use (8.7%), or addition of a second DMT (4.5%). Participants could select multiple reasons for a change in DMT use. Reasons given for a change in DMT use included adverse effects (26.0%), perceived lack of efficacy (19.2%), availability of new treatment options (13.8%), and financial reasons (7.1%).
CPS Selection
Participants most commonly indicated a preference for patient-centered decision making (CPS A+B; A 9.1% + B 38.8% = 47.9% [n = 3359]), followed by SDM (CPS C; 42.8% [n = 3000]) and physician-centered decision making (CPS D+E; D 7.1% + E 2.1% = 9.2% [n = 650]) (Table 1).
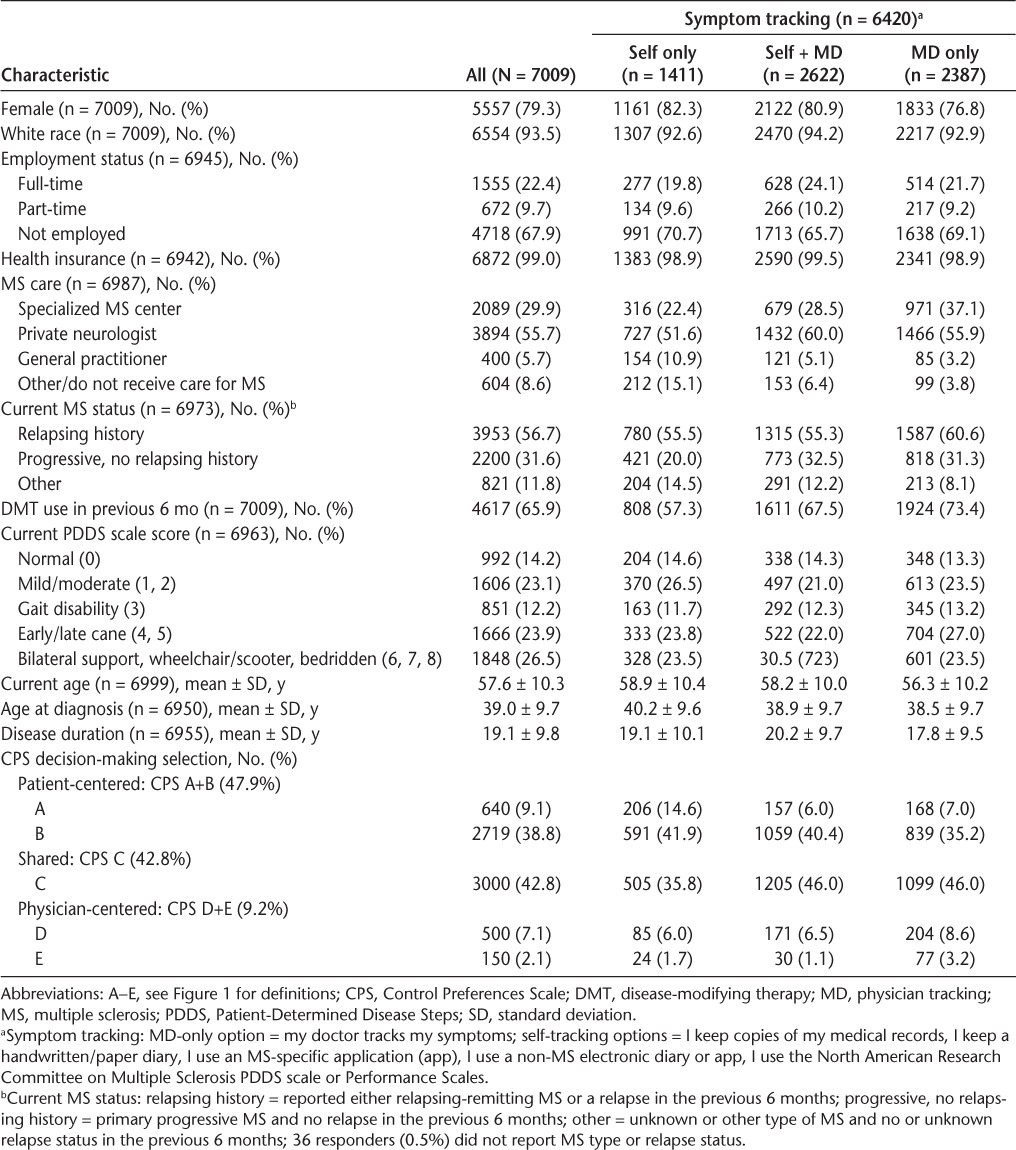
CPS and DMT Use (Without Covariate Adjustment)
Considering all 7009 respondents without covariate adjustment, a higher proportion of those who preferred patient-centered decision making reported no past DMT use compared with those who preferred SDM or physician-centered decision making (both P < .0001) (Figure 2); however, there was no difference in current DMT use between the SDM and physician-centered decision-making groups (P = .30). Among respondents who reported currently taking a DMT (n = 4617), there was no difference in the proportions of each CPS category between those who reported a change to DMT compared with those who did not report a change to DMT in the previous 6 months (P = .29; comparison of “DMT yes, with change” proportions) (Figure 2).
Figure 2.
Percentage of respondents reporting disease-modifying therapy (DMT) use by Control Preferences Scale (CPS) group, unadjusted for covariates
See Figure 1 for definitions of A–E.
CPS Selection: Covariate-Adjusted Model
A single covariate-adjusted logistic regression model evaluating the association of covariates with CPS selection was based on 6842 participants who had complete data for the covariates discussed later herein. Overall, CPS selection was not related to current health insurance status, reporting of a relapse in the previous 6 months, or ever having a relapse (all P > .05). Age at the time of the survey (P < .0001), current employment status (P < .01), current PDDS scale score (P = .0001), interaction between current DMT use at update and DMT history at enrollment (P = .0001), and gender by disease duration at update (P = .02) were associated with CPS selection. All the results later herein are from the covariate-adjusted model.
CPS and DMT Use
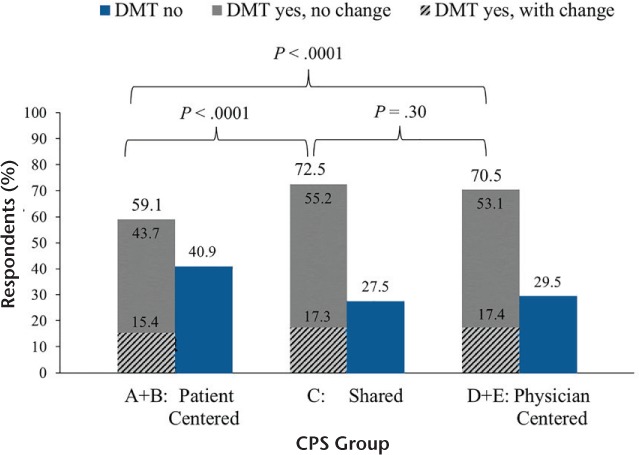
Considering DMT use at the time of enrollment and again at the time of the update, participants overall were most likely to prefer patient-centered decision making versus physician-centered decision making (P < .001) and SDM versus physician-centered decision making (P = .03) (Figure 3). The proportion reporting SDM was higher among those who were currently using a DMT (DMT use at update, yes) than those who were not (DMT use at update, no). The proportion reporting physician-centered decision making was also higher among those currently using a DMT than those who were not. The lowest proportion reporting physician-centered decision making was among those who had never taken a DMT at enrollment and were not on a DMT at the update (Figure 3).
Figure 3.
Predicted probability of Control Preferences Scale selection for current disease-modifying therapy (DMT) use by history of DMT use reported at enrollment (DMT ever at enrollment)
See Figure 1 for definitions of A–E.
For individuals currently taking a DMT (DMT use at update, yes) (Figure 3), there was no difference in the proportion indicating patient-centered decision making between those with a history of DMT use (41.3%; DMT history at enrollment) and those who had no history of DMT use (39.4%; no DMT history at enrollment), and neither were there differences between those indicating SDM (46.2% vs. 46.8%) and those indicating physician-centered decision making (12.5% vs. 13.8%, both P > .05). However, for those with no current DMT use (DMT use at update, no), a higher proportion without a history of DMT use selected patient-centered decision making (CPS A+B; 67.4%) than those who had previously taken a DMT (58.1%, P < .01). For those not currently taking a DMT but with a history of DMT use at enrollment, a higher proportion preferred SDM and physician-centered decision making (33.0% and 8.9%, respectively) compared with those with no history of DMT use (28.0% and 4.6%, respectively; P = .02 and P < .0001 for history of DMT and no history of DMT at enrollment, respectively). In general, patient-centered decision making was preferred most by respondents with no current DMT use, and SDM and physician-centered decision making were preferred most by those currently taking a DMT.
CPS and Disability
Overall, patient-centered decision making was the most common selection among all disability groups, followed by SDM and then physician-centered decision making (Supplementary Figure 1 (379.4KB, pdf) ). The likelihood of preferring patient-centered decision making to SDM was not different across disability levels (all P > .05). The likelihood of preferring patient-centered decision making or SDM compared with physician-centered decision making was greater for all disability levels (all P < .05). There was no difference in the likelihood of selecting patient-centered decision making or SDM versus physician-centered decision making between the normal, mild/moderate, gait, or early/late cane use groups (all P > .05). However, the likelihood of preferring patient-centered decision making and SDM versus physician-centered decision making was lower for those with higher disability levels (PDDS scale scores 6, 7, and 8) than for the normal group (PDDS scale score 0; P = .001 and .02, respectively).
CPS, Age, and Duration of Disease
The CPS selection varied by age (P < .0001) (Figure 4A). Preference for patient-centered decision making was high at most ages but decreased as age increased; conversely, SDM and physician-centered decision-making preferences increased with age. In general, selection of patient-centered decision making decreased as disease duration increased for both men and women (Figure 4B). However, preference for SDM became more common among women but less common among men as disease duration increased. Selection of physician-centered decision making remained stable for women but increased for men as disease duration increased. However, as disease duration increased, the likelihood of SDM compared with physician-centered decision making selection was higher for women compared with men (P < .01).
Figure 4.
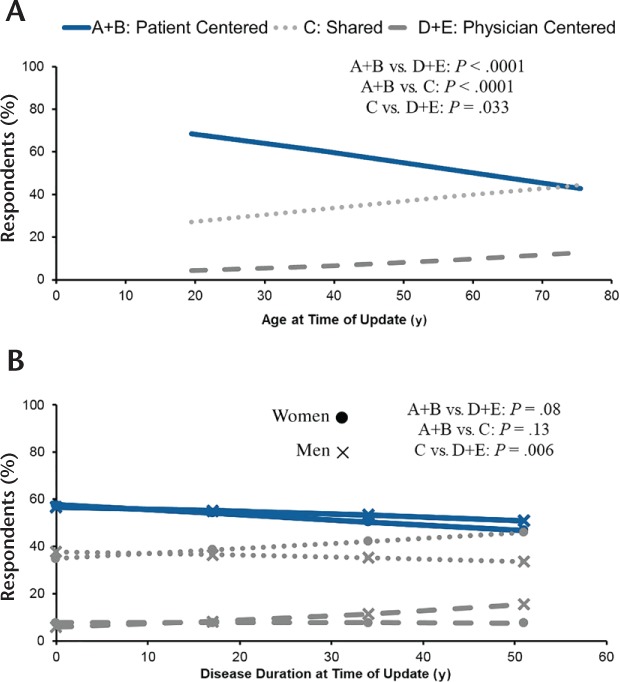
Predicted probability of Control Preferences Scale selection by current age (A) and gender and disease duration (B)
See Figure 1 for definitions of A–E.
CPS and Employment Status
Participants who were currently employed full-time were more likely to prefer patient-centered decision making versus physician-centered decision making (P = .02) and SDM versus physician-centered decision making (P = .03) compared with participants who were not employed. There was no difference in CPS selection between participants working part-time and those who were not employed (all P > .05).
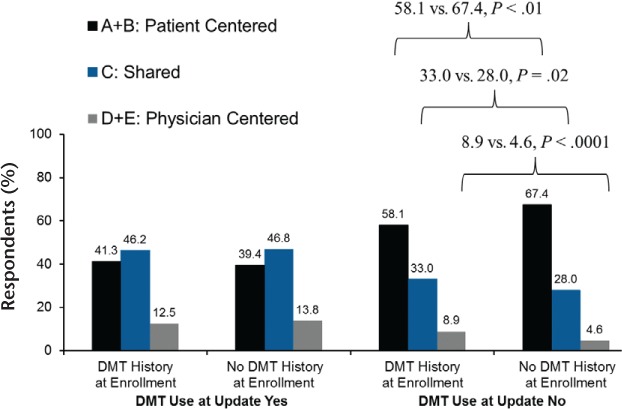
CPS and Symptom Tracking
Of the 7009 responders included in the analysis, 589 (8.4%) did not answer the symptom-tracking questions, 2387 (34.1%) exclusively relied on their doctor to track symptoms, and 4033 (57.5%) tracked their own symptoms with or without physician tracking (Figure 5). Of respondents who indicated how they track their symptoms, physician-only tracking was highest for those preferring physician-centered decision. Self-tracking, in conjunction with physician tracking, of symptoms was the most common method among those who preferred shared and patient-centered decision making (P < .0001). However, among those reporting patient-centered decision making, a higher proportion reported tracking their own symptoms compared with responders with other decision-making preferences. Women, those receiving MS care from a general practitioner, and those not currently using a DMT were more likely to track their own symptoms (all P < .0001) (Table 1).
Figure 5.
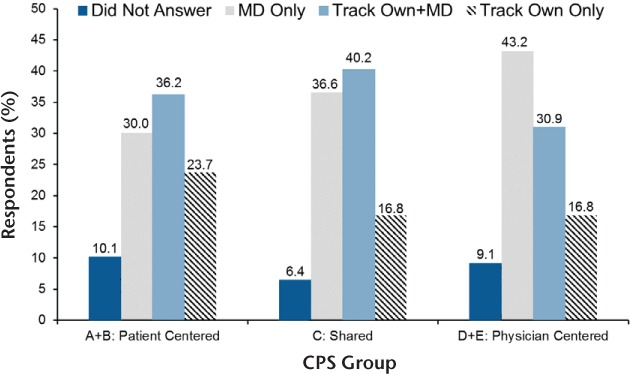
Control Preferences Scale (CPS) selection and symptom tracking
See Figure 1 for definitions of A–E. MD, physician tracking.
Discussion
This study investigated 7009 people with MS with a wide range of demographic and clinical characteristics on their role preference in their medical decision making regarding DMT selection and symptom tracking. This study found that most responders preferred their role in decision making to be at the more autonomous end of the spectrum, consistent with previous research.4,5,8,19,23 Although some factors associated with role preference (age, gender, DMT use) were consistent with other reports,4,5 MS type alone (relapsing history vs. history of progressive without relapsing) was not associated with CPS selection in the present study. This could be due to factors such as current age, disease duration, DMT use, and current disability level being closely associated with MS type. NARCOMS Registry participants have also shown a high level of health literacy and understanding of risks associated with treatment and may, therefore, be more comfortable with complex medical decisions across all types of MS.11–13
Factors associated with the selected role preference were age, employment status, current disability level, DMT use, gender, and disease duration. As age increased, participants were less likely to choose patient-centered decision making and more likely to choose SDM. Role preference was generally consistent across disability levels, but this study did not specifically address whether changes in disability affect the role that participants prefer in their decision making. Further investigation into changes in role preference and the factors that drive those changes would be useful for health-care professionals. A similar effect was seen for disease duration regarding the patient-centered decision-making preference. However, as disease duration increased, men were more likely to choose physician-centered decision making and women were more likely to choose SDM.
As may be expected, participants indicating a physician-centered decision-making preference were also more likely to rely on their physician to track their MS symptoms. Interestingly, approximately 30% of those who indicated a patient-centered decision-making preference nevertheless relied on their physician to track their symptoms. Multiple resources in addition to the traditional paper diaries are currently available for self-tracking of symptoms, such as apps for smartphones, tablets, and computers. These convenient high-tech resources could potentially facilitate more patient involvement in decision making regarding symptom and disease management as well as encourage dialogue and recall about those symptoms between visits. However, such causal conclusions cannot be made based on cross-sectional data alone.
This study has several strengths. Role preference was investigated in a large, sociodemographically diverse cohort, and several factors that may be associated with role preference were examined. Participants reported a range of MS care locations, treatment types, and disease statuses, with both online and paper submissions included to reduce potential bias associated with survey type. Although choice of DMT is a major decision for people with MS, there are several other medical decisions required during the course of the disease to which the SDM approach still applies. To address this issue, we chose to use the CPS to capture role preference regarding medical decisions in a general context rather than regarding the most recent decision or a change in DMT, which would have excluded patients who are not receiving a DMT.
The limitations of this study should also be recognized. NARCOMS Registry participants are volunteers and may not fully represent the MS population, although the characteristics of the Registry population are similar to those reported elsewhere.24–26 Participants self-reported their level of disability but did so using the PDDS scale that has been validated previously.21,27 Owing to the self-report nature of the NARCOMS Registry survey (not clinic based), the CPS was not administered in the iterative format for patients to choose between successive sets of SDM options; rather, respondents simply selected the image they felt most closely reflected their SDM preference. In addition, the categories at each end of the CPS were combined with the categories next to them for analysis purposes, which could potentially affect the associations observed in this study. However, because the proportion of responders selecting one of the end categories was relatively small (11.2% selecting A or E) (Figure 1), this approach is not likely to affect the conclusions. The single response method used herein produced similar results to previous research with the iterative selection process and allowed for inclusion of a large, diverse MS population that did not require an in-person visit or technical requirements beyond access to the survey. Also, due to the self-report nature of the NARCOMS Registry, the full range of explanatory variables is not collected through the routine surveys; thus, the present analysis was not able to incorporate the perspective of health-care providers or physicians on the decision-making process. However, previous research has shown that health-care providers prefer patient-centered roles in decision making.8
Role preference is an essential factor for health-care providers to understand in SDM situations. Assessing and accommodating a patient's role preference has the potential to improve the interactions in patient encounters and ensure that the decisions made reflect the patient's needs and preferences. The images from the CPS are an easy way for health-care providers to determine whether a patient prefers SDM or is on the patient- or physician-centered side of the spectrum. Knowledge of each individual's role preference could also assist health-care providers in taking the steps needed to ensure that their patients are equipped with accurate and up-to-date information for them to be involved in decision making at the level they prefer.
PracticePoints
Most people with MS prefer to be highly involved in decision making regarding their disease.
In discussing an optimal course of treatment, health-care providers should account for the patient's values and preferences in the decision-making process.
Further investigation is warranted to assess whether tools for people with MS to track their own symptoms could serve a role in encouraging and enhancing shared decision making between patients and health-care providers.
Supplementary Material
Acknowledgments
Survey design, data collection, and analysis were conducted by NARCOMS.
Financial Disclosures
Dr. Cofield has received consulting fees from the Department of Defense, American Shoulder and Elbow Surgeons, and for Data and Safety Monitoring Committee service from MedImmune Inc and grant support from Pfizer. Ms. Thomas is an employee of Genentech Inc. Dr. Fox has received personal compensation for consulting activities with Allozyne, Avanir, Biogen, EMD Serono, Novartis, Questcor, Teva, and Xenoport and research support from Biogen and Novartis. Drs. Tyry and Salter have no conflicts of interest to disclose.
Funding/Support
The NARCOMS Registry is supported (in part) by the Consortium of Multiple Sclerosis Centers (CMSC) and the Foundation of the CMSC. Additional funding for this project was provided by Genentech Inc. Third-party writing support for the manuscript was provided by Health Interactions and Articulate Science and was funded by Genentech Inc.
Disclaimer
Genentech Inc did not have direct access to the data and did not perform any statistical analyses but did collaborate with interpretation and writing of results.
References
- 1. National Learning Consortium. . Shared Decision Making Fact Sheet. https://www.healthit.gov/sites/default/files/nlc_shared_decision_making_fact_sheet.pdf. Published December 2013. Accessed April 14, 2016.
- 2. Informed Medical Decisions Foundation. . The Six Steps of Shared Decision Making. http://cdn-www.informedmedicaldecisions.org/imdfdocs/SixStepsSDM_CARD.pdf. Accessed April 14, 2016.
- 3. Elwyn G, Frosch D, Thomson R, . et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012; 27: 1361– 1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Heesen C, Kasper J, Segal J, . et al. Decision role preferences, risk knowledge and information interests in patients with multiple sclerosis. Mult Scler. 2004; 10: 643– 650. [DOI] [PubMed] [Google Scholar]
- 5. Heesen C, Köpke S, Richter T, Kasper J.. Shared decision making and self management in multiple sclerosis: a consequence of evidence. J Neurol. 2007; 254 suppl 2: II/116– II/121. [DOI] [PubMed] [Google Scholar]
- 6. Kasper J, Köpke S, Mulhauser I, . et al. Informed shared decision making about immunotherapy for patients with multiple sclerosis (ISDIMS): a randomized controlled trial. Eur J Neurol. 2008; 15: 1345– 1352. [DOI] [PubMed] [Google Scholar]
- 7. Heesen C, Köpke S, Solari A, . et al. Patient autonomy in multiple sclerosis: possible goals and assessment strategies. J Neurol Sci. 2013; 331: 2– 9. [DOI] [PubMed] [Google Scholar]
- 8. Rieckmann P, Boyko A, Centonze D, . et al. Achieving patient engagement in multiple sclerosis: a perspective from the Multiple Sclerosis in the 21st Century Steering Group. Mult Scler Relat Disord. 2015; 4: 202– 218. [DOI] [PubMed] [Google Scholar]
- 9. Elwyn G, Laitner S, Coulter A, . et al. Implementing shared decision making in the NHS. BMJ. 2010; 341: c5146. [DOI] [PubMed] [Google Scholar]
- 10. Say R, Murtagh M, Thomson R.. Patients' preference for involvement in medical decision making: a narrative review. Patient Educ Couns. 2006; 60: 102– 114. [DOI] [PubMed] [Google Scholar]
- 11. Marrie RA, Salter AR, Tyry T, . et al. Health literacy association with health behaviors and health care utilization in multiple sclerosis: a cross-sectional study. Interact J Med Res. 2014; 3: e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fox RJ, Salter AR, Alster JM, . et al. Risk tolerance to MS therapies: survey results from the NARCOMS registry. Mult Scler Relat Disord. 2015; 4: 241– 249. [DOI] [PubMed] [Google Scholar]
- 13. Salter AR, Marrie RA, Agashivala N, . et al. Patient perspectives on switching disease-modifying therapies in the NARCOMS registry. Patient Prefer Adherence. 2014; 8: 971– 979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Degner LF, Sloan JA, Venkatesh P.. The Control Preferences Scale. Can J Nurs Res. 1997; 29: 21– 43. [PubMed] [Google Scholar]
- 15. De Las Cuevas C, Peñate W, de Rivera L.. To what extent is treatment adherence of psychiatric patients influenced by their participation in shared decision making? Patient Prefer Adherence. 2014; 8: 1547– 1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hageman MG, Reddy R, Makarawung DJ, . et al. Do upper extremity trauma patients have different preferences for shared decision-making than patients with nontraumatic conditions? Clin Orthop Relat Res. 2015; 473: 3542– 3548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Moise N, Ye S, Alcántara C, Davidson KW, Kronish I.. Depressive symptoms and decision-making preferences in patients with comorbid illnesses. J Psychosom Res. 2017; 92: 63– 66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Singh JA, Sloan JA, Atherton PJ, . et al. Preferred roles in treatment decision making among patients with cancer: a pooled analysis of studies using the Control Preferences Scale. Am J Manag Care. 2010; 16: 688– 696. [PMC free article] [PubMed] [Google Scholar]
- 19. Solari A, Giordano A, Kasper J, . et al. Role preferences of people with multiple sclerosis: image-revised, computerized self-administered version of the Control Preference Scale. PLoS One. 2013; 8: e66127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hohol MJ, Orav EJ, Weiner HL.. Disease steps in multiple sclerosis: a longitudinal study comparing disease steps and EDSS to valuate disease progression. Mult Scler. 1999; 5: 349– 354. [DOI] [PubMed] [Google Scholar]
- 21. Learmonth YC, Motl RW, Sandroff BM, . et al. Validation of Patient Determined Disease Steps (PDDS) scale scores in persons with multiple sclerosis. BMC Neurol. 2013; 13: 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Chewning B, Bylund C, Shah B, . et al. Patient preferences for shared decisions: a systematic review. Patient Educ Couns. 2012; 86: 9– 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Köpke S, Kern S, Ziemssen T, . et al. Evidence-based patient information programme in early multiple sclerosis: a randomised controlled trial. J Neurol Neurosurg Psychiatry. 2014; 85: 411– 418. [DOI] [PubMed] [Google Scholar]
- 24. Culpepper WJ, Wallin MT, Magder LS, . et al. VHA Multiple Sclerosis Surveillance Registry and its similarities to other contemporary multiple sclerosis cohorts. J Rehabil Res Dev. 2015; 52: 263– 272. [DOI] [PubMed] [Google Scholar]
- 25. Marrie RA, Cutter G, Tyry T, . et al. Validation of the NARCOMS registry: diagnosis. Mult Scler. 2007; 13: 770– 775. [DOI] [PubMed] [Google Scholar]
- 26. Vollmer T, Ni W, Stanton S, Hadjimichael O.. The NARCOMS patient registry: a resource for investigators. Int J MS Care. 1999; 1: 12– 15. [Google Scholar]
- 27. Marrie RA, Goldman M.. Validity of performance scales for disability assessment in multiple sclerosis. Mult Scler. 2007; 13: 1176– 1182. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


