Abstract
Context:
Dexmedetomidine, α2-adrenergic agonist, when coadministered with local anesthetics, improves the speed of onset, duration of analgesia and decreases the dose of local anesthetic used.
Aims:
The aim of this study was to compare the efficacy of local subcutaneous wound infiltration of ropivacaine alone with ropivacaine plus dexmedetomidine for postoperative pain relief following lower segment cesarean section (LSCS).
Subjects and Methods:
The study was a prospective, randomized control, double-blind study. Sixty female patients belonging to physical status American Society of Anesthesiologists Grade I or II scheduled for LSCS under spinal anesthesia were randomly allocated into two groups of thirty patients each. Group A: local subcutaneous wound infiltration of 0.75% ropivacaine (3 mg/kg) diluted with normal saline to 40 ml. Group B: local subcutaneous wound infiltration of 0.75% ropivacaine (3 mg/kg) plus dexmedetomidine (1.5 μg/kg) of the body weight diluted with normal saline to 40 ml. Standard spinal anesthesia technique was used and LSCS was conducted. The allocated drug was administered by local subcutaneous wound infiltration before closure of the skin. In postoperative period, pain was assessed using visual analog scale (VAS) over a period of 24 h, time of giving first rescue analgesic consumption, mean analgesic consumption, patient satisfaction, and incidence of side effects in 24 h postoperative period was noted.
Statistical Analysis Used:
All observations were tabulated and statistically analyzed using Chi-square test and unpaired t-test.
Results:
A total number of patients requiring rescue analgesic, mean VAS each time rescue analgesic was given, and the mean analgesic required in 24 h postoperative period was lesser in Group B than in Group A.
Conclusions:
Dexmedetomidine added to ropivacaine for the surgical wound infiltration significantly reduces postoperative pain and rescue analgesic consumption in patients undergoing LSCS. No serious adverse effects were noted.
Keywords: Dexmedetomidine, lower segment cesarean section, postoperative pain relief, ropivacaine
INTRODUCTION
Pain relief after cesarean delivery is very important as the consequences of inadequate pain relief are borne not only by the mother but also by the newborn as well, since a parturient who is experiencing pain finds it difficult to feed her newborn.[1] Pain management for a parturient is challenging, as opioids, which otherwise are the mainstay analgesics in the postoperative period are avoided in the parturient because of their excretion in milk predisposing the neonate to their adverse effects.[2] Hence, other modalities for pain relief are often selected. Nowadays, multimodal approach to pain relief is recommended so that adverse effects of individual drugs can be reduced. Neuraxial blocks, peripheral nerve blocks, nonsteroidal anti-inflammatory drugs (NSAIDs), and local anesthetic infiltration of wound have all been used as a part of multimodal approach.[3]
Local wound infiltration is an attractive strategy since it is efficacious and side effects are minimal.[4] Nowadays, there is a trend toward preferring ropivacaine over other local anesthetic agents due to longer duration of action and better safety profile.[5] Local anesthetic infiltration, however, has a limitation in that pain relief is offered till the effects of local anesthetic action lasts. Efforts are being made to prolong the duration of action of local anesthetic skin infiltration, and dexmedetomidine is one such agent which can potentiate and prolong the duration of local anesthetic wound infiltration for pain relief. A lot of literature is available for the role of dexmedetomidine as an adjuvant to ropivacaine for peripheral nerve blocks and intrathecally as a part of spinal anesthesia.[6] However, only limited data are available for the use of dexmedetomidine as an adjuvant to local infiltration of surgical wound.[7,8,9] We, therefore, planned to compare the safety and efficacy of dexmedetomidine as an adjuvant to ropivacaine local infiltration of surgical wound for postoperative pain relief after cesarean delivery.
SUBJECTS AND METHODS
This study was conducted at a tertiary level hospital in a randomized double-blinded manner on a total of sixty parturients belonging to physical status American Society of Anesthesiologists (ASA) Grade I or II, scheduled for cesarean delivery under spinal anesthesia. Prior approval from the Institutional Ethics Committee was obtained, and informed consent was obtained from all patients. The exclusion criteria were a history of drug abuse, psychiatric disease, obesity with weight >100 kg, allergic reaction to local anesthetics, opioids and/or dexmedetomidine, inability to comprehend visual analog scale (VAS), or failed spinal anesthesia with subsequent conversion to general anesthesia. Patients were enrolled in the study after a thorough preanesthetic checkup and routine investigations which included a complete hemogram, coagulation profile, and random blood sugar. All patients were shown and explained regarding the VAS and instructed to its use in the postoperative period, and they were also informed that they can request an analgesic at any time after surgery if they feel pain.
After shifting the patients to the operation theater, preinduction heart rate (HR), noninvasive blood pressure, respiratory rate (RR), oxygen saturation (SpO2), and electrocardiography were recorded. These parameters were monitored throughout the procedure and recorded every 5 min. An intravenous (IV) access was achieved, and normal saline infusion commenced. After preloading with 10 ml/kg body weight of IV fluids, all patients were administered subarachnoid block in the left lateral position under all aseptic precautions using a 26-gauge Quincke's needle at L3–4/L4–5 vertebral level injecting 2.0 ml of 0.5% heavy bupivacaine. The onset of sensory block was defined as the time between intrathecal injection of anesthetic agent and the absence of pain at T8 dermatome, assessed by pinprick. Time for motor block was assumed when modified Bromage score became one. Grade 1 = complete block (unable to move feet or knees); Grade 2 = almost complete block (able to move feet only); Grade 3 = partial block (just able to move knees); Grade 4 = detectable weakness of hip flexion while supine (full flexion of knees); Grade 5 = no detectable weakness of hip flexion while supine; and Grade 6 = able to perform partial knee bend. Surgery was allowed to proceed after complete sensory block was achieved at T8 dermatome as assessed by pinprick. The duration of spinal anesthesia was defined as the period from intrathecal injection of the drug to the first occasion when the patient complained of pain in the postoperative period.
In case of partial/failed spinal anesthesia, general anesthesia was administered, and the patient was excluded from the study. Intraoperative complications such as hypotension, bradycardia, and nausea/vomiting were managed as per departmental policy in both the groups. After the closure of uterus and muscle layer but before closure of skin, the allocated drug as per random grouping based on coded sealed envelope technique was administered by local subcutaneous wound infiltration at the incision site, by the obstetrician who was blinded to the study drug administered. The investigator scoring patient outcome after surgery was also blinded to the protocol.
Patients in Group A were administered local subcutaneous wound infiltration of 0.75% ropivacaine 3 mg/kg (rounded to nearest multiple of ten) diluted with normal saline to a total volume of 40 ml, whereas Group B patients were given local subcutaneous wound infiltration of 0.75% ropivacaine 3 mg/kg (rounded to nearest multiple of ten) plus dexmedetomidine 1.5 μg/kg (rounded to nearest multiple of ten, using a 1 cc syringe) diluted with normal saline to 40 ml.
The time of subcutaneous infiltration of test drug was labeled as 0 and observations started from this time onward and patient shifted to postanesthesia care unit (PACU). On arrival to PACU, patients were asked to rate the pain using VAS rulers having slide indicator with 0–10 analog scale etched on the front. Patients were asked to bring the slider on the scale on to the point that they feel represents their current state of pain with “0” mark corresponding to no pain and “10” mark representing worst imaginable pain. Patients were monitored for postoperative pain and any analgesic requirement for a period of 24 h.
Any patient complaining of pain or reporting VAS ≥4 at any time was administered tramadol 100 mg IV slowly over 2–3 min. If pain was not relieved after 30 min and patients still complained of pain, additional doses of tramadol 50 mg IV were given, and this dose could be repeated every 30 min up to a total dose of 250 mg in 6 hourly and maximum of 400 mg of tramadol over 24 h. Time of first rescue analgesic administration and total rescue analgesic consumed in 24 h postoperatively was noted. Patients were also evaluated for any adverse effects, 24 h postoperatively.
In the PACU, the following parameters were observed and recorded.
HR, blood pressure, RR, SpO2 every 10 min for 1 h, and then every half hourly for the next 2 h followed by every hour till 24 h
Assessment of pain using VAS whenever patient complained of pain and 10 min after giving rescue analgesic
Time of first rescue analgesic administration in the postoperative period
Total analgesic consumption in the 24 h postoperative period
Patients were also observed for any adverse effect such as postoperative nausea with or without vomiting, skin rash (redness or itching), hypotension (defined as blood pressure <15% of baseline values), sedation (as per Ramsay sedation scale[10]), respiratory depression (defined as RR <10/min), need for supplemental oxygen (saturation <93%), bradycardia (HR <60 beats/min), and any redness or signs of inflammation at the skin incision site
-
Patient satisfaction was graded as
-
∘Excellent (4)
-
∘Good (3)
-
∘Moderate (2)
-
∘Poor (1).
-
∘
Analysis of data
After completion of the study, observations obtained were tabulated, and data were expressed as mean and 95% confidence interval of mean for continuous variables (height, weight, duration, and age). Data were analyzed using Statistical Package for the Social Sciences (SPSS) version 15 (SPSS Inc., Chicago, IL, USA). Comparison of continuous data between groups was done using independent t-test (ANOVA of means). Comparison of nominal data was done using Chi-square analysis and ordinal data using Mann–Whitney test. P < 0.05 was considered statistically significant between groups.
Sample size for the study was estimated by taking into consideration the results of a previous study by Kang.[7] This study had found that VAS scores were significantly lower until 24 h after surgery, and fentanyl consumption and the frequency to push button of patient-controlled analgesia (PCA) pump were significantly lower in group receiving local wound infiltration with ropivacaine plus dexmedetomidine until postoperative 12 h (601.54 ± 111.65) compared with that of group receiving ropivacaine alone (735.85 ± 158.43). Based on this, a sample size of 54 patients was needed to detect 10% difference with 90% power and α of 0.05. As dropout cases would be expected due to failure of spinal anesthesia and conversion to general anesthesia, a sample size of sixty was selected for the study.
RESULTS
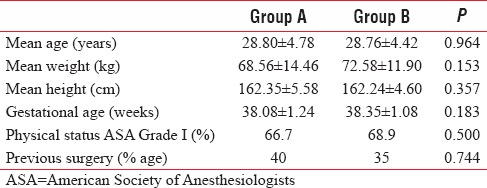
There was no significant difference among the two groups with respect to mean age, height, weight, and gestational age. Majority of the patients had no previous history of cesarean section in either of the groups and belonged to physical status ASA I category [Table 1].
Table 1.
Demographic profile
Postoperatively, the baseline HR was comparable between Group A and Group B (P = 0.373). On intergroup comparison between Group A and Group B, HR was lower in Group B than in Group A at most time intervals and was statistically significant. Intragroup comparison of HR showed gradual fall with time in both the groups, but this gradual decrease in HR was greater in Group B [Figure 1].
Figure 1.
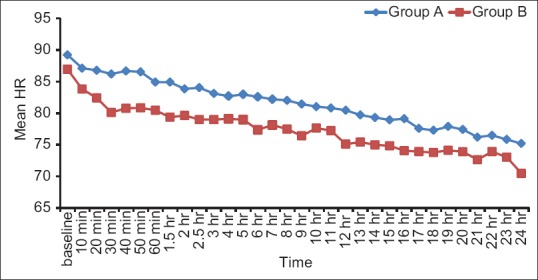
Mean heart rate among the two groups
Baseline mean arterial pressure in the postoperative period was similar in both the groups, being 88.67 ± 12.11 mmHg and 88.47 ± 9.07 mmHg in Groups A and B, respectively (P = 0.927). Intergroup comparison showed no significant difference in mean arterial pressure among the two groups. Overall, there was a trend toward a fall in mean arterial pressure with time and this decline in mean arterial pressure was more in Group B [Figure 2].
Figure 2.
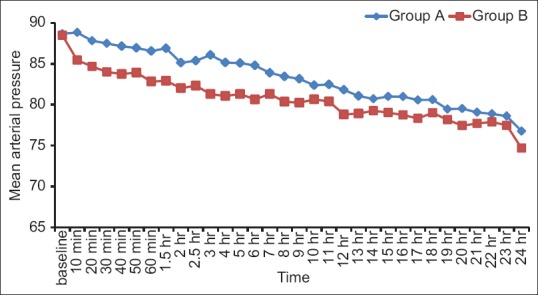
Postoperative mean arterial pressure
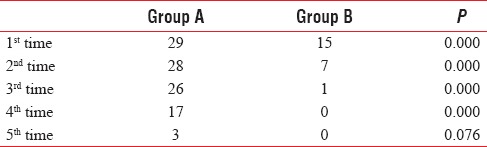
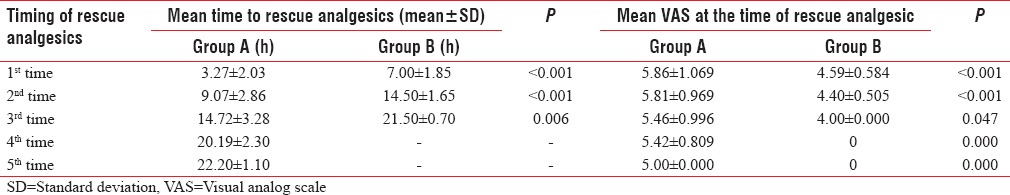
The number of patients administered first, second, and third doses of rescue analgesics were significantly greater in Group A as compared to Group B [Table 2]. None of the patients in Group B needed more than three doses of rescue analgesia, whereas in Group A, 17 patients needed rescue analgesic for 4th time and three patients were administered a rescue analgesic for 5th time. This difference was statistically significant four out of five times of rescue analgesic administration [Table 2].
Table 2.
Total number of patients requiring rescue analgesic in each group
The need for IV rescue analgesic for the first time was at 3.27 ± 2.03 h in Group A and at 7.00 ± 1.85 h in Group B [Table 3]. Thus, the need for the first dose of rescue analgesia was earlier in Group A as compared to Group B and the difference was statistically significant (P < 0.001). Similarly, the need for second and third doses of rescue analgesics was significantly later in Group B and the difference was statistically significant with P < 0.001 and 0.006, respectively. The time for fourth and fifth rescue analgesic was at 20.19 ± 2.30 and at 22.20 ± 1.10 h in Group A, whereas patients in Group B did not require any additional rescue analgesics after that. Mean VAS was higher in ropivacaine alone group at each time rescue analgesic was given, compared to Group B and results were statistically significant [Table 3].
Table 3.
Mean time to rescue analgesics and visual analog scale at that time interval
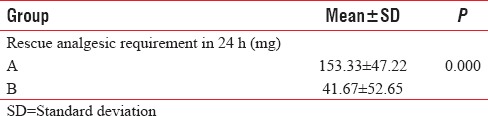
The mean analgesic requirement in Group A was also greater as compared to Group B and the difference was statistically significant (P = 0.000) [Table 4].
Table 4.
Mean cumulative dose of rescue analgesic requirement in 24 h (mg)
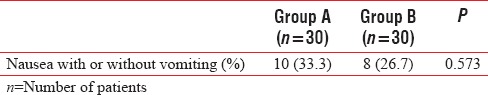
None of the patients developed skin rash, respiratory depression, hypotension, hypoxemia, sedation, bradycardia, or any signs of local wound inflammation. The incidence of nausea with or without vomiting was found to be comparable in both the groups with P = 0.573 [Table 5].
Table 5.
Incidence of adverse effects
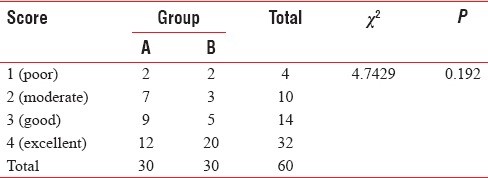
No statistical difference with regard to satisfaction scores was detected [Table 6].
Table 6.
Satisfaction score
DISCUSSION
To the best of our knowledge, only two studies have been conducted to compare the postoperative pain outcomes of local subcutaneous wound infiltration of ropivacaine and ropivacaine with dexmedetomidine in patients undergoing inguinal herniorrhaphy and hemorrhoidectomy, respectively.[7,8]
Opioids are the most commonly used analgesics for the relief of postoperative pain after cesarean section, either by intrathecal or epidural administration before section or oral, subcutaneous, transdermal, parenteral administration postoperatively. However, the risk of complications such as respiratory depression, urinary retention, pruritus, nausea, and vomiting can cause discomfort to the patient. On the other hand, nonopioid systemic analgesics such as cyclooxygenase inhibitors mainly NSAIDs, α2-agonists, nitric oxide, and N-methyl-aspartate are not potent enough to allow effective pain control after cesarean section. In addition, NSAIDs are associated with an increased incidence of gastrointestinal problems, kidney dysfunction, and bleeding diathesis.
In addition to the above-mentioned interventions, incisional infiltration with local anesthetics has been demonstrated as an effective technique for postoperative pain relief after lower segment cesarean section (LSCS) as part of a multimodal approach and is simple to give, safe, and cost effective.[11,12] Patient is not only pain free but also remains alert and cooperative with only a few of the side effects of narcotics. Local anesthetics also have the advantage of encouraging early mobilization and possibility of reducing the risk of deep vein thrombosis. The mother–child contact can be established earlier, and this contributes to their psychologic well-being. The use of this analgesic technique does not lead to any increase in wound dehiscence or infection in LSCS cases.[13] Hence, we have chosen local anesthetic wound infiltration for postoperative pain relief in our study.
Ropivacaine is the local anesthetic of choice in our study whose potency, duration of action, and cost are comparable to bupivacaine with a significantly reduced cardiotoxicity. The delay in local diffusion because of intrinsic vasoconstrictive property makes it at a lower risk for cardiovascular side effects due to decreased systemic absorption. The recommended dosage of ropivacaine for minor nerve block and wound infiltration for surgical anesthesia, in an adult weighing 60 kg or more, is 225 mg of 7.5 mg/ml solution and for postoperative analgesia is up to 200 mg of 2 mg/ml solution[14] although recent studies on ropivacaine have demonstrated a longer duration of skin analgesia with higher doses than used before.[13,15,16]
We have selected a dose of 3 mg/kg body weight so that the total dose remains well below the maximum safe dose of 300 mg[15,17] since systemic absorption and plasma concentration, which is proportional to the weight, may be of importance in ensuring drug safety.
Incisional wound infiltration of ropivacaine directly into the wound to relieve post-LSCS pain has been supported by authors, but, it has a limited duration of action (30 min to 6 h)[14] and no intrinsic sedative properties, leading to increased demand of sedatives and hence respiratory depression in the immediate postoperative period. A variety of adjuvants such as epinephrine, α2-adrenoceptor agonists, ketorolac, magnesium, sodium bicarbonate, and hyaluronidase to local anesthetics have been investigated and used to overcome these problems.
Dexmedetomidine, an α2-adrenoceptor agonist, provides analgesia and sedation without respiratory depression when administered by IV, epidural, and intrathecal route. A synergistic interaction between dexmedetomidine and local anesthetics has been observed when given by these routes.[18,19,20] However, scant studies are available to know the analgesic efficacy of wound infiltration of local anesthetics with dexmedetomidine for postoperative pain relief and none after LSCS. We have given dexmedetomidine in a dose of 1.5 mcg/kg of body weight based on the studies,[7,9] wherein authors have administered subcutaneous dexmedetomidine in the range of 1–2 μg/kg for postoperative pain relief.
None of the patients were excluded from our study. Both the groups were statistically comparable with respect to demographic profile.
The total number of patients who demanded rescue analgesic in Group B was 15 as compared to 29 in Group A. This reflects 50% decrease in patient suffering in terms of pain with the use of ropivacaine plus dexmedetomidine in local infiltration. Total analgesic requirement for postoperative pain relief in the form of IV tramadol was significantly less in Group B (P = 0.000). Mean value of tramadol required in Group A in 24 h was 153.33 ± 47.22 mg, whereas it was 41.67 ± 52.65 mg in Group B. Thus, surgical incision infiltration with ropivacaine plus dexmedetomidine decreases the total rescue analgesic demand by 72% in 24 h postoperative period. VAS values at each time patient complained of pain and rescue analgesic was given, were significantly low in Group B patients compared to Group A patients (P = 0.000). Furthermore, rescue analgesic was required up to five times in group with plain ropivacaine but only 3 times in group with ropivacaine and dexmedetomidine in 24 h. Thus, less number of patients reported pain and demanded rescue analgesic in Group B over 24 h indicating better pain relief with the use of dexmedetomidine.
Our results correlate well with the observations of Kang,[7] who studied the effect of dexmedetomidine added to preemptive ropivacaine infiltration on postoperative pain after inguinal herniorrhaphy and found reduction in postoperative pain after surgery. A significant reduction in pain scores, fentanyl consumption, and frequency of pushing the PCA button was noted in group of patients with ropivacaine and dexmedetomidine as compared to ropivacaine alone.
Our results are also consistent with the findings of Kim and Kang,[8] who studied the effect of preemptive perianal ropivacaine and ropivacaine with dexmedetomidine on pain after hemorrhoidectomy and found that perianal ropivacaine with dexmedetomidine is effective. Significant reduction in VAS scores, fentanyl use for analgesia, and frequency with which the PCA was pushed (P < 0.005) were found until the 24 h postoperative period.
The incidence of nausea and vomiting was not found to be statistically different among the two groups. Possible explanation for no such difference could be a smaller number of patients included to reach the level of significance for postoperative nausea and vomiting. No significant differences were detected between both groups in terms of patient satisfaction.
Although our study showed that additional local infiltration of dexmedetomidine improves postoperative pain and reduces the need for rescue analgesic, the underlying mechanism of analgesic effect of dexmedetomidine remains unclear. The possible mechanisms suggested for this phenomenon, include:
Inhibition of the impulse conduction in primary afferents, especially C fibers
Anti-inflammatory effects by decreasing the production of inflammatory cytokines
Prolongation of analgesic duration by vasoconstriction through α2-adrenergic receptor on vascular smooth
Inhibition of pain generation by inhibition of tetrodotoxin-sensitive Na(+) channels, and
Supraspinal analgesia secondary to the absorption of dexmedetomidine to systemic circulation.[21,22,23,24]
Our study has some limitations worth mentioning. First of all, the surgeries were conducted by different surgeons, thus causing differences in tissue handling and local anesthetic infiltration. Second, dose of dexmedetomidine was arbitrarily selected, and blood levels of ropivacaine and dexmedetomidine were not measured. Third, all of our patients belonged to physical status ASA Grade I and II with no severe underlying disease; therefore, the results of the present study should not be generalized to all the patients.
On the other hand, few advantages of our study are worth mentioning. First, only elective cesarean sections were included to avoid the type, nature, and duration of pain associated with different types of surgery. Second, all the VAS measurements were carried out by a single observer to eliminate any interobserver variability.
Nevertheless, reduction in a total number of patients requiring rescue analgesics with reduced VAS pain scores, lesser tramadol consumption, and no sedation was observed in patients receiving ropivacaine with dexmedetomidine. The quality of analgesia as evidenced by reduced pain intensity and total postoperative rescue analgesic demand was better with ropivacaine plus dexmedetomidine as compared to ropivacaine alone. Thus, dexmedetomidine seems to be an attractive adjuvant to ropivacaine for subcutaneous wound infiltration in patients undergoing LSCS.
CONCLUSIONS
Dexmedetomidine added to ropivacaine for the surgical wound infiltration significantly reduces postoperative pain and rescue analgesic consumption in patients undergoing LSCS patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Klaus MH, Kennell JH, Plumb N, Zuehlke S. Human maternal behavior at the first contact with her young. Pediatrics. 1970;46:187–92. [PubMed] [Google Scholar]
- 2.Dahl JB, Jeppesen IS, Jørgensen H, Wetterslev J, Møiniche S. Intraoperative and postoperative analgesic efficacy and adverse effects of intrathecal opioids in patients undergoing cesarean section with spinal anesthesia: A qualitative and quantitative systematic review of randomized controlled trials. Anesthesiology. 1999;91:1919–27. doi: 10.1097/00000542-199912000-00045. [DOI] [PubMed] [Google Scholar]
- 3.Sujata N, Hanjoora VM. Pain control after cesarean birth – What are the options? J Gen Pract. 2014;2:164. [Google Scholar]
- 4.Rawal N, Axelsson K, Hylander J, Allvin R, Amilon A, Lidegran G, et al. Postoperative patient-controlled local anesthetic administration at home. Anesth Analg. 1998;86:86–9. doi: 10.1097/00000539-199801000-00017. [DOI] [PubMed] [Google Scholar]
- 5.Whiteside JB, Wildsmith JA. Developments in local anaesthetic drugs. Br J Anaesth. 2001;87:27–35. doi: 10.1093/bja/87.1.27. [DOI] [PubMed] [Google Scholar]
- 6.Abdallah FW, Brull R. Facilitatory effects of perineural dexmedetomidine on neuraxial and peripheral nerve block: A systematic review and meta-analysis. Br J Anaesth. 2013;110:915–25. doi: 10.1093/bja/aet066. [DOI] [PubMed] [Google Scholar]
- 7.Kang H. The effect of dexmedetomidine added to preemptive ropivacaine infiltration on post-operative pain after inguinal herniorrhaphy: A prospective, randomized, double-blind, placebo-controlled study. Eur Surg. 2012;44:274–80. [Google Scholar]
- 8.Kim BG, Kang H. The effect of preemptive perianal ropivacaine and ropivacaine with dexmedetomidine on pain after hemorrhoidectomy: A prospective, randomized, double-blind, placebo-controlled study. Indian J Surg. 2014;76:49–55. doi: 10.1007/s12262-012-0622-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ulgey A, Gunes I, Bayram A, Bicer C, Kurt FM, Muderis I. The analgesic effects of incisional levobupivacaine with dexmedetomidine after total abdominal hysterectomy. Erciyes Med J. 2015;37:64–8. [Google Scholar]
- 10.Ramsay MA, Savege TM, Simpson BR, Goodwin R. Controlled sedation with alphaxalone-alphadolone. Br Med J. 1974;2:656–9. doi: 10.1136/bmj.2.5920.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Trotter TN, Hayes-Gregson P, Robinson S, Cole L, Coley S, Fell D. Wound infiltration of local anaesthetic after lower segment caesarean section. Anaesthesia. 1991;46:404–7. doi: 10.1111/j.1365-2044.1991.tb09558.x. [DOI] [PubMed] [Google Scholar]
- 12.Ganta R, Samra SK, Maddineni VR, Furness G. Comparison of the effectiveness of bilateral ilioinguinal nerve block and wound infiltration for postoperative analgesia after caesarean section. Br J Anaesth. 1994;72:229–30. doi: 10.1093/bja/72.2.229. [DOI] [PubMed] [Google Scholar]
- 13.Nguyen NK, Landais A, Barbaryan A, M’barek MA, Benbaghdad Y, McGee K, et al. Analgesic efficacy of pfannenstiel incision infiltration with ropivacaine 7.5 mg/mL for caesarean section. Anesthesiol Res Pract 2010. 2010 doi: 10.1155/2010/542375. pii: 542375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kuthiala G, Chaudhary G. Ropivacaine: A review of its pharmacology and clinical use. Indian J Anaesth. 2011;55:104–10. doi: 10.4103/0019-5049.79875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pettersson N, Berggren P, Larsson M, Westman B, Hahn RG. Pain relief by wound infiltration with bupivacaine or high-dose ropivacaine after inguinal hernia repair. Reg Anesth Pain Med. 1999;24:569–75. doi: 10.1016/s1098-7339(99)90051-2. [DOI] [PubMed] [Google Scholar]
- 16.Gottschalk A, Burmeister MA, Radtke P, Krieg M, Farokhzad F, Kreissl S, et al. Continuous wound infiltration with ropivacaine reduces pain and analgesic requirement after shoulder surgery. Anesth Analg. 2003;97:1086–91. doi: 10.1213/01.ANE.0000081733.77457.79. [DOI] [PubMed] [Google Scholar]
- 17.Wulf H, Worthmann F, Behnke H, Böhle AS. Pharmacokinetics and pharmacodynamics of ropivacaine 2 mg/mL, 5 mg/mL, or 7.5 mg/mL after ilioinguinal blockade for inguinal hernia repair in adults. Anesth Analg. 1999;89:1471–4. doi: 10.1097/00000539-199912000-00029. [DOI] [PubMed] [Google Scholar]
- 18.Wahlander S, Frumento RJ, Wagener G, Saldana-Ferretti B, Joshi RR, Playford HR, et al. A prospective, double-blind, randomized, placebo-controlled study of dexmedetomidine as an adjunct to epidural analgesia after thoracic surgery. J Cardiothorac Vasc Anesth. 2005;19:630–5. doi: 10.1053/j.jvca.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 19.Saadawy I, Boker A, Elshahawy MA, Almazrooa A, Melibary S, Abdellatif AA, et al. Effect of dexmedetomidine on the characteristics of bupivacaine in a caudal block in pediatrics. Acta Anaesthesiol Scand. 2009;53:251–6. doi: 10.1111/j.1399-6576.2008.01818.x. [DOI] [PubMed] [Google Scholar]
- 20.Gupta R, Bogra J, Verma R, Kohli M, Kushwaha JK, Kumar S. Dexmedetomidine as an intrathecal adjuvant for postoperative analgesia. Indian J Anaesth. 2011;55:347–51. doi: 10.4103/0019-5049.84841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gaumann DM, Brunet PC, Jirounek P. Hyperpolarizing afterpotentials in C fibers and local anesthetic effects of clonidine and lidocaine. Pharmacology. 1994;48:21–9. doi: 10.1159/000139158. [DOI] [PubMed] [Google Scholar]
- 22.Kim MH, Hahn TH. The effect of clonidine pretreatment on the perioperative proinflammatory cytokines, cortisol, and ACTH responses in patients undergoing total abdominal hysterectomy. Anesth Analg. 2000;90:1441–4. doi: 10.1097/00000539-200006000-00035. [DOI] [PubMed] [Google Scholar]
- 23.Ebert TJ, Hall JE, Barney JA, Uhrich TD, Colinco MD. The effects of increasing plasma concentrations of dexmedetomidine in humans. Anesthesiology. 2000;93:382–94. doi: 10.1097/00000542-200008000-00016. [DOI] [PubMed] [Google Scholar]
- 24.Maruta T, Nemoto T, Satoh S, Kanai T, Yanagita T, Wada A, et al. Dexmedetomidine and clonidine inhibit the function of Na(V) 1.7 independent of a(2)-adrenoceptor in adrenal chromaffin cells. J Anesth. 2011;25:549–57. doi: 10.1007/s00540-011-1168-6. [DOI] [PubMed] [Google Scholar]


