Abstract
OBJECTIVES
Irritable bowel syndrome (IBS) is a stress-sensitive disorder associated with early adverse life events (EALs) and a dysregulated hypothalamic-pituitary-adrenal (HPA) axis. Resilience is the ability to recover and adapt positively to stress but has not been well studied in IBS. The aims of this study are to compare resilience in IBS and healthy controls (HCs) and to assess its relationships with IBS symptom severity, quality of life (QOL), EALs, and HPA response.
METHODS
256 subjects (154 IBS, 102 HCs) completed questionnaires for resilience (Conner Davidson Resilience Scale [CD-RISC] and Brief Resilience Scale [BRS]), IBS symptoms, IBS-QOL, and EALs. Ninety-six of these subjects had serial serum adrenocorticotropic hormone (ACTH) and cortisol levels to exogenous corticotropin releasing hormone (CRH) and ACTH measured. The relationship between IBS status, resilience, and other variables of interest was assessed by regression analysis after adjusting for demographics and neuroticism, a predictor of resilience.
RESULTS
Resilience was significantly lower in IBS compared to HCs (CD-RISC: 72.16±14.97 vs. 77.32±12.73, p=0.003; BRS: 3.29±0.87 vs. 3.93±0.69, p<0.001); however, only BRS was significant after controlling for neuroticism (p=0.001). Lower BRS scores were associated with greater IBS symptom severity (p=0.002), poorer IBS-QOL (p<0.001), and a higher number of EALs (p=0.01). There was a significant interaction between BRS resilience and IBS status for ACTH stimulated cortisol response (p=0.031); more resilient IBS subjects, had lower cortisol response, and more resilient HCs, had higher cortisol response.
CONCLUSIONS
Lower resilience is associated with IBS status, worse IBS symptom severity, lower IBS-QOL, greater EALs, and stress hyperresponsiveness.
Graphical abstract
IBS patients have decreased resilience, particularly the ability to bounce back from adversity, compared to healthy controls. Lower resilience in IBS was associated with worse symptoms and quality of life, early life adversity and altered cortisol response.
BACKGROUND
Resilience is characterized by the ability to maintain homeostasis against internal and external stressors, and recover from and adapt positively to stress and adversity (1–5). In some disorders such as PTSD, fibromyalgia, rheumatoid arthritis, and osteoarthritis, it has been associated with positive coping and less emotional distress (2,6,7). Furthermore, in a large survey of the general population in the United States, between 50–60% of individuals experience traumatic events, yet only 7.8% developed posttraumatic stress disorder (PTSD) in their lifetime (8). This suggests that many individuals are resilient. The study of resilience is a growing area of research that represents a shift from a vulnerability and disease-centered approach in treatment seeking populations, to an effort to identify factors that promote wellness through positive adaptations and to appreciate the full complexity of human behavior including the strengths that allow individuals to survive and grow despite adversity. Resilience has been found to be associated with structural changes in brain regions involved in cognitive and affective processes involved in the modulation of stress and emotional responses (9). A greater understanding of the role of resilience and its neurobiologic correlates may provide insights on the pathophysiology and vulnerability to developing a stress-sensitive disorder such as irritable bowel syndrome (IBS). In addition, resilience measures have the potential to be predictive of symptom severity, stress responsiveness, and outcomes in IBS.
IBS is a gastrointestinal (GI) disorder characterized by abdominal pain and associated with alterations in stool form and/or frequency (10). Three studies measured resilience in IBS using a validated instrument, the Connor-Davidson Resilience Scale (CD-RISC) (11–13). Two of these studies were conducted in Iran and found that resilience scores were lower in IBS patients compared to healthy controls (HCs) (11,13). However, these studies did not appear to control for neuroticism, which has been shown to be a significant predictor of resilience (14,15). Neuroticism is generally defined as a disposition to experience negative emotions such as anxiety, anger, sadness, guilt, and hatred (14). A third study was conducted in Israel and included IBS patients diagnosed by a gastroenterologist without the use of symptom criteria. The authors found that lower resilience in IBS was associated with greater psychological distress and depressive symptoms (11). Thus, it is valuable to delineate an independent relationship between the resilience and IBS separate from neuroticism, negative emotionality, and psychological sensitivity to stress. Furthermore, to our knowledge, there are no studies that have evaluated the association of resilience to IBS symptom severity or stress-related biologic measures such as cortisol.
Several survey instruments measure resilience, including the CD-RISC, which is one of the more widely used resilience questionnaires. The CD-RISC captures personal qualities embodying resilience including personal competence, tolerance of negative affect, adaptability, sense of control over one’s life, and spiritual faith (2). The Brief Resilience Scale (BRS) was developed to concisely assess resilience, specifically the ability to “bounce back” or recover from stress, as this was considered to be the fundamental definition of resilience (i.e., as opposed to resistance to illness). When studying patients who are already ill, assessing the specific ability to recover may have value compared to assessing the ability to resist illness (15). Both the CD-RISC and the BRS have been tested in clinical samples and in the general population with good internal consistency and test-retest reliability (2,15). The BRS has not been previously used in IBS patients as a measure of resilience.
Predisposing factors that can affect resilience include early life experience, genetic factors, and developmental environment (3). Early adverse life events (EALs) have been found to increase the risk of developing IBS and can be associated with alterations in the central stress response systems, including the hypothalamic-pituitary-adrenal (HPA) axis (16–18). In addition, studies have supported a dysregulated HPA axis in IBS even in the absence of EALs (19,20). There is some data in the current literature suggesting that resilience can affect the response to stress, and that resilience scores are associated with changes in brain regions involved in stress responsiveness (9,11–13); however, to our knowledge, this has not been examined in IBS in regards to symptom severity, quality of life, and physiologic markers of stress.
The aims of this study are: (i) to compare resilience in IBS patients and healthy controls (HCs) using two measures, the CD-RISC and BRS; (ii) to examine the relationships between resilience and IBS symptom severity and disease related quality of life (QOL); (iii) to determine if resilience is associated with EALs and IBS status; and (iv) to determine if resilience is associated with the HPA axis response to a hormone challenge. We hypothesized that resilience, as measured by CD-RISC and BRS is: (i) lower in IBS subjects compared to HCs even when controlling for neuroticism; (ii) negatively correlated with IBS symptom severity and positively correlated with IBS-QOL; (iii) lower in subjects with a history of EALs, particularly in those with IBS; and (iv) lower in subjects with a greater HPA axis response to a hormone challenge.
METHODS
Study Subjects
Male and female participants who were at least 18 years of age and participating in studies conducted at our clinical research center between November 2012 and September 2016 were recruited. IBS subjects were predominantly recruited from newspaper or Internet community advertisements and fulfilled Rome III diagnostic criteria (21). The diagnosis was confirmed by a clinician with expertise in IBS. HC subjects were recruited by advertisement and did not have a history of IBS or other chronic GI or pain conditions, and were not taking psychotropic medication or participating in psychotherapy. Subjects were compensated for the completion of a medical history, physical examination, and questionnaires.
The study was approved by the UCLA Institutional Review Board, and all subjects signed a written informed consent prior to starting the study.
Questionnaires
The Conner-Davidson Resilience Scale (CD-RISC)
The Conner-Davidson Resilience Scale (CD-RISC) is a 25-item self-rated assessment developed to measure and qualify resilience as the ability to cope with stress and adversity; higher scores reflect greater resilience (score range 0–100). The CD-RISC was developed with the goal of establishing norms for resilience in the general population and clinical samples, and to assess the extent to which resilience scores change in response to treatment (2).
The Brief Resilience Scale (BRS)
The Brief Resilience Scale (BRS) is a questionnaire that specifically measures “the ability to bounce back” or recover from stress. It is composed of 6 questions with an equal number of positively and negatively-worded questions and each question is rated on a 5-point scale. Higher scores reflect greater bounce back resilience (score range 0–5). (15)
IBS health-related symptoms and outcomes
IBS health-related symptoms and outcomes were surveyed using the Irritable Bowel Syndrome-Quality of Life (IBS-QOL) surveys. The IBS-QOL (22) is a validated IBS specific survey which contains 41 questions assessing disease-specific QOL over the past 30-days, on a 5-point scale; lower scores signify poorer health-related QOL (score range 1–100). In addition, the overall IBS symptom severity and abdominal pain over the past week were assessed using a 0–20 numeric rating scale (none to most intense imaginable), and usual severity of IBS symptoms (“How bad are your symptoms usually? 1=none, 2=mild, 3=moderate, 4=severe, 5=very severe).
Other Psychological Measures
The Early Trauma Inventory Self Report- Short Form (ETI-SR)
The Early Trauma Inventory Self Report- Short Form (ETI-SR) inventories the occurrence (before the age of 18) of 27 EAL items in the following domains: general trauma (11 items), physical (5 items), emotional (5 items), and sexual abuse (6 items). Each of the 27 items is scored as ‘Yes’ = 1 or ‘No’ = 0 (score range 0–27). (23) The ETI-SR has previously been used in studies of EALs in IBS (16,18).
The Hospital Anxiety and Depression (HAD) Scale
The Hospital Anxiety and Depression (HAD) Scale (24) measures current anxiety and depression symptoms (score range 0–21).
The Perceived Stress Score (PSS)
The Perceived Stress Score (PSS) (25) is a validated 10-item questionnaire used to evaluate the association of perceived stress over the past 1-month with disease severity in chronic conditions (score range 0-40).
Personality
Personality Traits including neuroticism and extraversion were measured using the Mini-International Personality Item Pool (IPIP) (26,27), a twenty item questionnaire measuring the Big Five factors of personality (i.e. extraversion, agreeableness, conscientiousness, neuroticism, and intellect/imagination) (score range 10–50). Example items for neuroticism include, “I have frequent mood swings.”, “I get upset easily.”, and for extraversion include, “I am the life of the party.”, “I don’t talk a lot” (negatively scored).
Hormone Challenge Tests
A subset of patients who completed the resilience questionnaires underwent tests to measure the hypothalamic-pituitary-adrenal (HPA) axis response to a hormone challenge. The results of the hormone challenge tests in a larger group of IBS and HC subjects were previously published (19).
Corticotropin releasing factor (CRF) stimulation test
An intravenous (IV) catheter was placed at 1300 h. Blood samples for ACTH and cortisol levels were collected from 1500 h (−60 min) to 1600 h (0 min) in 30-min intervals. At 1600 h, 1 μg/kg bovine CRF (Acthrel, Ferring, New York) was given by IV. Blood samples were collected at 5, 15, 30, 60, 90, and 120 min after the administration of CRF.
ACTH stimulation test
The ACTH stimulation test was performed at least one week after the CRF stimulation test. IV catheters were placed into a forearm vein at 0800 h. Blood samples for base-line ACTH and cortisol were collected at 0830 h and 0900 h. 250 μg Cortrosyn (Organon, West Orange, N.J.) was administered by IV at 0900 h. Blood samples for cortisol were collected at 30, 60, 90, 120, 150, and 180 min after ACTH was given. Participants were fasting.
Samples were collected, processed, and assayed according to the standard operating procedures of the UCLA Clinical and Translational Research Center. The assays for ACTH and cortisol were performed using the IMMULITE system (Siemens Healthcare Diagnostics Inc). Baseline values were calculated as the average of the values prior to CRF/ACTH administration.
Statistical Methods
Continuous variables were summarized as means and standard deviation and categorical variables as count (%) and simple comparison tests (i.e. Wilcoxon or Chi-square tests) were used to compare differences between IBS and HC. Linear regression analyses were used to estimate the relationships among the variables of interest and were adjusted for age, sex and education. The regression analysis to assess whether the relationship between resilience and IBS status differed by sex was controlled for age and education. As previously mentioned, because resilience has been shown to be negatively correlated with neuroticism in patient populations (7,14,15), we tested to see if any differences between resilience and the presence of IBS remained after adjusting for neuroticism. When testing the relationships between resilience scores and GI symptom severity and IBS-QOL, we also evaluated whether PSS could affect these relationships by testing the interaction between PSS with GI symptoms or IBS-QOL on resilience. We wanted to determine if the relationships between resilience and IBS symptom severity and QOL were not mainly due to current perceived stress rather than chronic stress responsiveness.
The responses to the hormone challenge tests were analyzed by calculating the area under the curve with respect to the minimum value (AUCi) using the trapezoidal method. The rise slope was calculated using the slope of the regression line from the baseline to peak. The decline slope was calculated using the slope of the regression line from peak to the lowest value after the peak.
Statistical analyses were conducted in SAS v. 9.4, statistical significance was assessed at the 0.05 level and all tests were two-tailed.
Sample size calculation
We planned the sample size for our study using estimates provided by Zarpour and Besharat (11) in which IBS subjects (mean resilience of 90.61 and a standard deviation of 13.26) had lower mean resilience compared to healthy controls (mean resilience of 96.35 with a standard deviation of 16.94) using the Conner-Davidson Resilience Scale (CD-RISC). Using G*Power 3.1.9.2 and a two-sample t-test based with an α error rate of 5%, a total of 176 subjects (88 IBS and 88 HC) were needed to detect decreased resilience (Effect Size: Cohen’s d=0.377) in IBS subjects compared to HC with 80% power.
RESULTS
Subject characteristics
A total of 256 subjects participated in the study, 102 were HCs (61% women, mean age=28.6) and 156 were patients with IBS (71% women, mean age=29.4) (Table 1). There were no statistically significant differences between the two groups for sex, age, and education. IBS patients had higher psychological symptom scores compared to those for HCs.
Table 1.
Subject Characteristics
| All Subjects | Hormone Challenge Subjects Only | |||||
|---|---|---|---|---|---|---|
| Variable | HCs (n=102) | IBS (n=154) | p-value | HCs (n=37) | IBS (n=54) | p-value |
| Age | 28.64 (9.77) | 29.42 (9.7) | 0.457 | 27.59 (9.24) | 28.96 (10.78) | 0.599 |
| Female: n (%) | 62 (61%) | 109 (71%) | 0.127 | 21 (57%) | 36 (67%) | 0.46 |
| Education: n (%) | 0.381 | 0.019 | ||||
| Some High School | 0 (0%) | 2 (1%) | 0 (0%) | 0 (0%) | ||
| High School Graduate | 6 (6%) | 4 (3%) | 4 (12%) | 0 (0%) | ||
| Some College | 35 (38%) | 60 (36%) | 11 (33%) | 29 (54%) | ||
| College Graduate | 28 (30%) | 38 (25%) | 11 (33%) | 11 (20%) | ||
| Any Post-Graduate | 24 (26%) | 48 (32%) | 7 (22$) | 14 (26%) | ||
| BMI | 25.9 (5.53) | 23.97 (4.5) | <0.001 | 26.46 (4.96) | 24.79 (5.07) | 0.08 |
| BRS Score (0–5) | 3.93 (0.69) | 3.29 (0.87) | <0.001 | 3.82 (0.68) | 3.51 (0.77) | 0.048 |
| CD-RISC Score (0–100) | 77.32 (12.73) | 72.16 (14.97) | <0.001 | 75.37 (12.57) | 75.18 (13.25) | 0.965 |
| IPIP | ||||||
| Neuroticism (10–50) | 21.43 (6.99) | 26.86 (7.69) | <0.001 | 21.16 (5.91) | 26.09 (7.31) | p<0.001 |
| Extraversion (10–50) | 34.79 (7.1) | 33.91 (9.17) | 0.379 | 35.04 (5.55) | 35.66 (8.02) | 0.445 |
| ETI-SR | ||||||
| General Score (0–31) | 1.43 (1.43) | 2.33 (2.11) | <0.001 | 1.38 (1.44) | 1.75 (1.86) | 0.444 |
| Physical Score (0–9) | 1.28 (1.48) | 1.35 (1.63) | 0.897 | 1.53 (1.48) | 1.5 (1.72) | 0.647 |
| Emotional Score (0–7) | 0.85 (1.44) | 1.76 (1.88) | <0.001 | 1.14 (1.59) | 1.83 (1.84) | 0.051 |
| Sexual Score (0–15) | 0.27 (0.84) | 0.63 (1.31) | <0.001 | 0.38 (1.06) | 0.52 (1.23) | 0.499 |
| Total Score (0–62) | 3.86 (3.65) | 5.97 (5.16) | <0.001 | 4.47 (3.8) | 5.6 (4.94) | 0.403 |
| HAD Anxiety (0–21) | 4.29 (3.16) | 8.12 (4.32) | <0.001 | 4.49 (3) | 7.89 (4.13) | p<0.001 |
| HAD Depression (0–21) | 1.61 (2) | 3.51 (3.05) | <0.001 | 1.86 (2.03) | 3.3 (3) | 0.025 |
| PSS Score (0–40) | 12.28 (6.44) | 18.15 (6.78) | <0.001 | 12.54 (5.92) | 17.96 (6.39) | p<0.001 |
| Bowel Habits | ||||||
| IBS-C | 31 (20%) | 10 (19%) | ||||
| IBS-D | 38 (25%) | 13 (24%) | ||||
| IBS-M | 80 (52%) | 30 (56%) | ||||
| IBS-U | 5 (3%) | 1 (1%) | ||||
| GI Symptoms | ||||||
| Overall Severity (0–20) | 9.38 (4.35) | 8.98 (3.97) | ||||
| Abdominal Pain (0–20) | 8.84 (4.2) | 9.36 (3.44) | ||||
| Usual Severity (1–5) | 3.35 (0.69) | 3.4 (0.6) | ||||
| IBS Quality of Life (1–100) | 64.1 (21.98) | 63.39 (19.92) | ||||
Abbreviations: Healthy controls (HC), Irritable bowel syndrome (IBS), Body mass index (BMI), Brief Resilience scale (BRS), Connor-Davidson Risk Scale (CD-RISC), International Personality Item Pool (IPIP), Early Trauma Inventory Self Report- Short form (ETI-SR), Hospital anxiety and depression scale (HAD), Perceived stress score (PSS), IBS with constipation (IBS-C), IBS with diarrhea (IBS-D), unsubtyped IBS (IBS-U), mixed IBS (IBS-M)
Resilience in IBS vs Healthy Controls
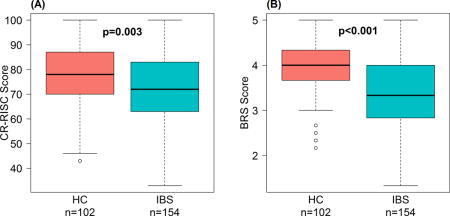
After adjusting for sex, age, and education, IBS patients were found to have significantly lower mean resilience scores compared to HCs as measured by both the CD-RISC (72.16 ± 14.97 vs. 77.32 ± 12.73, p=0.003) and BRS (3.29 ± 0.87 vs. 3.93 ± 0.69, p<0.001) (Figure 1). There were no sex differences for resilience in IBS and HCs with CD-RISC (t=0.79, p=0.43) and BRS (t=1.62, p=0.11); alternatively, in spite of controlling for sex, resilience was lower in IBS compared to that in HCs. When resilience scores were adjusted for neuroticism, patients with IBS had significantly lower resilience scores compared to HCs with BRS only (t= −3.33, p=0.001).
Figure 1. IBS patients have lower resilience scores compared to healthy controls.
Differences in resilience scores between IBS and HCs are shown after adjusting for sex, age, and education. (A) CD-RISC resilience in IBS (72.16 ± SD 14.97) vs. HCs (77.32 ± SD 12.73); (p=0.003). (B) BRS resilience in IBS (3.29 ± SD 0.87) vs. HCs (3.93 ± SD 0.69); (p<0.001).
Association between resilience and IBS outcomes
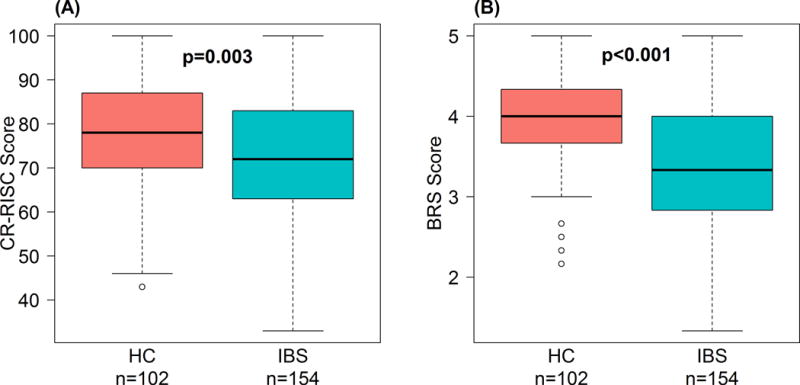
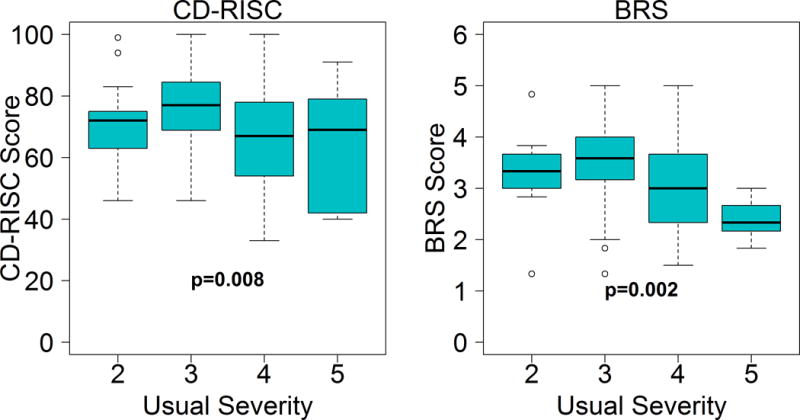
Among patients with IBS, increased usual symptom severity was associated with decreased resilience as measured by CD-RISC (t= −2.65, p=0.008) and BRS (t= −3.11, p=0.002) (Figure 2). Lower resilience scores were also associated with poorer IBS-QOL using CD-RISC (t=3.876, p<0.001) and BRS (t=4.70, p<0.001) (Figure 3). The relationships between resilience with GI symptom severity and IBS-QOL were not different when adjusted for PSS. In other words, the association between lower resilience and worse usual symptom severity and poorer disease-specific QOL were not explained by having higher current perceived stress. This association was tested because higher PSS scores were associated with lower resilience scores in IBS using the CD-RISC (t=−9.343, p<0.001) and BRS (t=−8.54, p<0.001). There were no associations between resilience and current overall IBS symptom severity, abdominal pain, or bloating ratings.
Figure 2. Resilience is associated with lower IBS usual severity.
IBS usual severity scored on a 1–5 scale (1-none, 2- mild, 3-moderate, 4-severe, 5- very severe). Compared to healthy controls, resilience scores as measured by A) CD-RISC (p=0.008) and B) BRS (p=0.002) were lower in IBS patients.
Figure 3. Resilience is positively correlated with quality of life in IBS.
Higher resilience scores were positively associated with IBS-QOL using CD-RISC (p<0.001) and BRS (p<0.001).
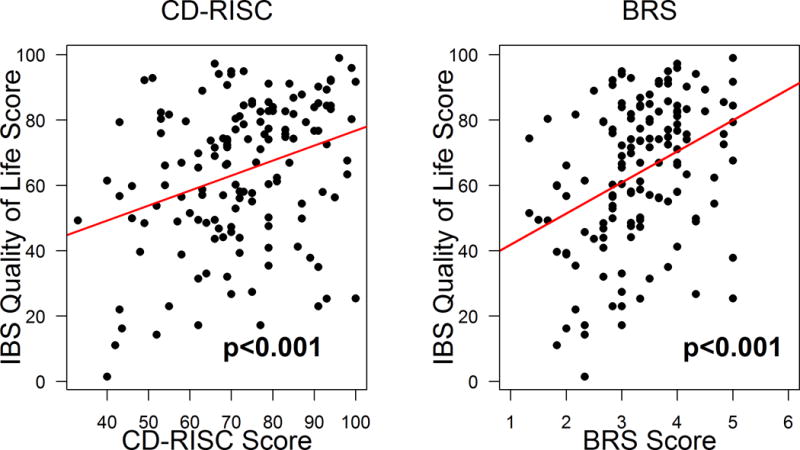
Association between EALs and resilience
There was a negative association between resilience scores and ETI-SR scores. An increased number of EAL events, as measured by the ETI-SR score, was significantly associated with a decreased resilience score as measured by both the CD-RISC (t=−2.65, p=0.009) and BRS (t=−2.55, p=0.011) across all subjects. In addition, IBS subjects had significantly lower resilience scores as measured by the CDRISC (p=0.019) and BRS (p<0.001) compared to HCs after controlling for ETI-SR scores (Figure 4). That is, if IBS and HC subjects have experienced a similar number of EAL events, IBS subjects have lower resilience scores than HC subjects.
Figure 4. Association of resilience scores and EALs.
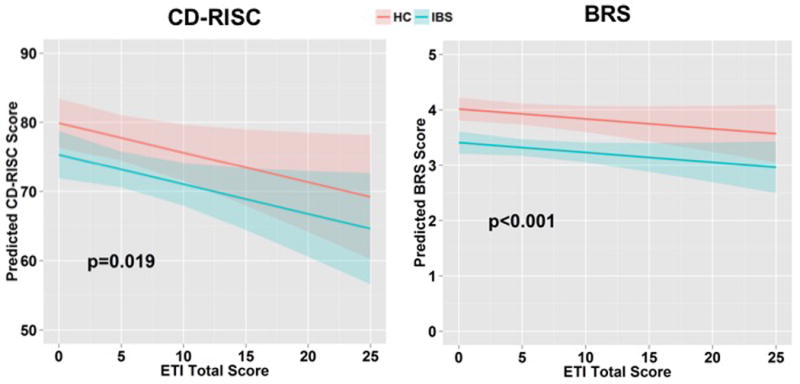
IBS subjects have significantly lower resilience scores compared to HCs when ETI-SR scores are controlled for with CDRISC (p=0.019) and BRS (p<0.001).
Association between HPA axis response and resilience
Out of 256 subjects, 91 (37 IBS and 54 HCs) underwent the hormone challenge study and completed the resilience surveys. The clinical characteristics for this subset were similar to the larger group of IBS and HC subjects (Table 1). There was a significant interaction between BRS resilience scores and IBS status on AUCi for ACTH stimulated cortisol response (p=0.031) (Figure 5). There was also a significant interaction between CD-RISC resilience scores and IBS status for the decline slope in the recovery of cortisol to baseline after ACTH stimulation (p=0.013). Less resilient HCs had a lower cortisol response to ACTH stimulation and a slower recovery to baseline compared to more resilient HCs. In contrast, less resilient IBS subjects had an enhanced cortisol response and faster recovery to baseline compared to more resilient IBS subjects. There were no significant associations between resilience scores and CRH-stimulated ACTH or cortisol response measures.
Figure 5. A greater cortisol response was associated with lower BRS resilience in IBS.
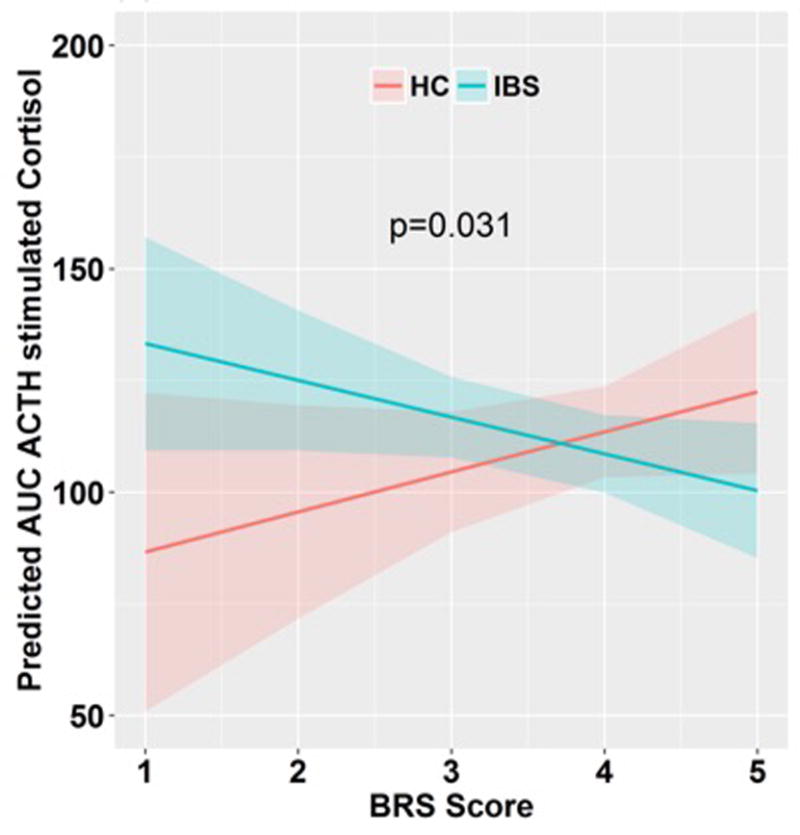
There was a significant interaction between BRS resilience scores and IBS status with AUCi for ACTH stimulated cortisol response (p=0.031). Less resilient HCs had a lower cortisol response to ACTH stimulation.
DISCUSSION
Resilience, a measure of successful stress coping ability, plays a role in the vulnerability to and the experience of disease, and can impact response to therapy (2,6,7). For example, in patients with PTSD, patients who demonstrated clinical improvement with short term pharmacotherapy had a greater increase in resilience scores compared to patients who did not improve (2). Studies of resilience in IBS, which are limited, have shown that patient with IBS have higher levels of neuroticism, less extraversion, and lower resilience (as measured by the CD-RISC and NEO Five Factor Inventory) compared to HCs and concluded that these personality variables can partially predict the development of IBS(10–12). Similar to these previous smaller studies, we found that IBS subjects had lower resilience compared to that in HCs as measured by the CD-RISC (11,13). However, we found that this difference in resilience measured by CD-RISC did not maintain significance when we controlled for neuroticism. The HCs may not represent the general population as we excluded control subjects with a history of chronic GI and pain conditions, use of psychotropic medication, or participation in psychotherapy. However, some HCs endorsed psychological symptoms, a history of EALs and/or perceived stress. Furthermore, mean CD-RISC scores of our HCs were similar or even lower than those of the general population in other studies. (2,11)
As the evolving definition of resilience is multidimensional, the BRS sought to measure resilience in its original and most basic construct, the ability to bounce back. In our study, even after adjusting for neuroticism, bounce-back resilience was a salient factor associated with IBS status, usual symptom severity, and disease-related QOL. Furthermore, the effect of resilience on disease related severity and QOL was not due to increased perceived stress, suggesting that lowered resilience in IBS is primarily due to a decreased ability to bounce back from stress or adversity. Less resilient IBS patients had a greater severity of usual symptoms, but not for current symptoms, which is not surprising as resilience probably has a greater impact on chronic outcomes. When used in a symptomatic patient population, the BRS can assess the ability to recover, rather than to simply resist illness. From a clinical practice perspective, patients with IBS who are less resilient may recover more slowly from disease flares, infections, surgeries or stressors. This innate ability to bounce back may be a mediator of other protective resources. In healthy individuals, fibromyalgia, and cardiac rehab patients, resilience was found to be positively correlated with optimism, social support, and purpose in life (15). These can be considered as targets for intervention. For example, more exercise days are correlated with higher resilience in cardiac rehabilitation patients (15). It is unclear if more resilient patients are more likely to exercise or if exercise can help to further build resilience; nonetheless, this may be a beneficial target for intervention and could be applicable to IBS. Physical exercise has been shown to be associated with decreased IBS symptom severity (29) and it is possible that an exercise program increases resilience as well.
We have shown that the more EALs an individual experiences, the lower their resilience tends to be; furthermore, this relationship is more prominent in patients with IBS. When HC and IBS subjects were exposed to the same number of EALs, HCs had higher resilience scores compared to those in patients with IBS, suggesting that the association of IBS with decreased resilience is independent of EALs. It is conceivable that subjects who have lower resilience go on to develop negative coping mechanisms and a hyperresponsive stress response in the face of childhood adversity, and become predisposed to disease.
To our knowledge, the association between resilience and HPA axis response has not been previously studied in IBS. We found a significant interaction between IBS status, resilience, and the stress hormone response, particularly the cortisol response to ACTH stimulation and the recovery of cortisol levels to baseline. We have previously shown that the ACTH-stimulated cortisol response is divergent with greater responses in IBS men vs. HC men and a blunted response in IBS women vs. HC women (19). In prior studies evaluating the relationship between resilience and HPA axis response, more resilient healthy individuals were found to have lower cortisol levels in response to a psychosocial stressor (30,31). These studies differ from ours because the hormone challenge method used in our study provides an isolated measurement of the HPA axis function, while the HPA axis response to a mental stressor task reflects changes in several components of the integrated response to stress, including inputs from the amygdala and other regions of the emotional arousal network which enhance HPA axis response (32). We previously demonstrated that healthy individuals with low resilience have compromised cortico-limbic inhibition. Such compromised modulation of emotional responses to stress is likely associated with enhanced HPA axis responses, making such individuals more vulnerable to stressful life events (9). IBS patients in general have decreased cortico-limbic inhibition (9,33) and an enhanced HPA axis response (20) particularly in less resilient patients. Interestingly, IBS and HC subjects had differing relationships between cortisol response and only BRS residence scores and between cortisol recovery to baseline levels and only CD-RISC scores. These findings suggest that the ability to bounce back from stress is reflected by stress responsiveness, while the multiple facets of resilience influences one’s adaptive response and ability to maintain homeostasis. However, further studies are needed to better understand and confirm these findings.
In conclusion, resilience is lower in IBS patients compared to HCs. In addition, resilience is negatively associated with IBS symptom severity, positively associated IBS-QOL, and negatively associated with EALs in HCs and IBS. Both the CD-RISC and BRS are useful measures of resilience in IBS, however the BRS is preferred for measuring bounce-back resilience, which was independent of neuroticism and current stress. Resilience has neurobiologic correlates as it is associated with morphologic changes in brain regions involved in executive control and emotional arousal as well as an individual’s response to stress. Future studies should focus on resilience and other factors that promote wellness and positive traits that may be associated with greater coping during adversity, less vulnerability to disease and negative outcomes, and improved treatment response.
Key Points.
Resilience is the ability to recover from and adapt positively to stress and adversity; limited studies have suggested that resilience is lower in patients with irritable bowel syndrome (IBS), a stress-sensitive disorder.
Decreased resilience, particularly the ability to bounce back from adversity, is more prevalent in IBS patients compared to healthy controls and is associated with worse symptoms and quality of life, early life adversity and altered cortisol response.
Future studies should focus on resilience and other factors that promote wellness and positive traits that may be associated with greater coping during adversity, less vulnerability to disease and negative outcomes, and improved treatment response.
Acknowledgments
We thank the study participants and the staff of the G. Oppenheimer Center for Neurobiology of Stress and Resilience and the Clinical and Translational Research Center at UCLA. We specifically want to thank Cathy Liu for management of the database and Arlene Licudine, Stephanie Yee, and Nafeesa Islam for their work as study coordinators.
Grant support: NIH/NIDDK P50 DK64539, R01 DK048351, T32 DK07180-40, P30 DK 41301
Abbreviations
- AUC
Area under the curve
- AUCi
Area under the curve with respect to minimum value
- BMI
Body mass index
- BRS
Brief Resilience scale
- CD-RISC
Connor-Davidson Risk Scale
- EALs
Early adverse life events
- ETI-SR
Early Trauma Inventory Self Report- Short form
- GI
Gastrointestinal
- HAD
Hospital anxiety and depression scale
- HCs
Healthy controls
- HPA axis
Hypothalamic-pituitary-adrenal axis
- IBS
Irritable bowel syndrome
- IPIP
International Personality Item Pool
- PSS
Perceived stress score
- QOL
Quality of life
Footnotes
Competing Interests: The authors have have no competing interests.
Author Contributions:
1. Sarah H. Park: study concept and design, analysis and interpretation of data, drafting of the manuscript; critical revision of the manuscript for important intellectual content
2. Bruce Naliboff: study concept and design, analysis and interpretation of data, critical revision of the manuscript for important intellectual content
3. Wendy Shih: acquisition of data, analysis and interpretation of data, statistical analysis, critical review and editing of manuscript
4. Angela P. Presson: analysis and interpretation of data, critical review and editing of the manuscript
5. Elizabeth Videlock: critical revision and editing of the manuscript for important intellectual content
6. Tiffany Ju: acquisition of data, critical revision and editing of the manuscript for important intellectual content
7. Lisa Kilpatrick: critical revision and editing of the manuscript for important intellectual content
8. Arpana Gupta: critical revision and editing of the manuscript for important intellectual content
9. Emeran Mayer: funding, critical revision of the manuscript for important intellectual content
10. Lin Chang: study concept and design, analysis and interpretation of data, acquisition of data, analysis and interpretation of data, critical revision of the manuscript for important intellectual content, funding, administrative and material support, study supervision
References
- 1.Rutter M. Resilience in the Face of Adversity Protective Factors and Resistance to Psychiatric Disorder *. Br J Psychiatry. 1985:598–611. doi: 10.1192/bjp.147.6.598. [DOI] [PubMed] [Google Scholar]
- 2.Connor KM, Davidson JRT. Development of a new Resilience scale: The Connor-Davidson Resilience scale (CD-RISC) Depress Anxiety. 2003;18:76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 3.Bowes L, Jaffee SR. Biology, genes, and resilience: toward a multidisciplinary approach. [Internet] Trauma Violence Abuse. 2013;14:195–208. doi: 10.1177/1524838013487807. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23649831. [DOI] [PubMed] [Google Scholar]
- 4.Bonanno GA. Loss, Trauma, and Human Resilience. 2004;59:20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- 5.Masten AS. Ordinary Magic. 2001;56:227–238. doi: 10.1037//0003-066x.56.3.227. [DOI] [PubMed] [Google Scholar]
- 6.Notario-Pacheco B, Martínez-Vizcaíno V, Trillo-Calvo E, et al. Validity and reliability of the Spanish version of the 10-item CD-RISC in patients with fibromyalgia. [Internet] Health Qual Life Outcomes. 2014;12:1–9. doi: 10.1186/1477-7525-12-14. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3922630&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith BW, Zautra AJ. Vulnerability and Resilience in Women With Arthritis : Test of a Two-Factor Model. 2008;76:799–810. doi: 10.1037/0022-006X.76.5.799. [DOI] [PubMed] [Google Scholar]
- 8.Kessler RC, Sonnega A, Nelson CB, et al. Posttraumatic Stress Disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 9.Gupta A, Love A, Kilpatrick LA, et al. Morphological brain measures of cortico-limbic inhibition related to resilience [Internet] J Neurosci Res. 2016 doi: 10.1002/jnr.24007. [cited 2017 Mar 3] Available from: http://doi.wiley.com/10.1002/jnr.24007. [DOI] [PMC free article] [PubMed]
- 10.Lacy BE, Mearin F, Chang L, et al. Bowel Disorders [Internet] Gastroenterology. 2016;150:1393–1407.e5. doi: 10.1053/j.gastro.2016.02.031. [cited 2017 Mar 4] Available from: http://linkinghub.elsevier.com/retrieve/pii/S0016508516002225. [DOI] [PubMed] [Google Scholar]
- 11.Zarpour S, Besharat MA. Comparison of personality characteristics of individuals with irritable bowel syndrome and healthy individuals [Internet] Procedia - Soc Behav Sci. 2011;30:84–88. Available from: http://dx.doi.org/10.1016/j.sbspro.2011.10.017. [Google Scholar]
- 12.Ben-ezra M, Hamama-raz Y, Palgi S, et al. Cognitive Appraisal and Psychological Distress Among Patients with Irritable Bowel Syndrome. 2015;52 [PubMed] [Google Scholar]
- 13.Roshan N, Yarahmadi Y, Parhizkar B. The compare resilience in patients with irritable bowel syndrome and normal individuals in Sanandaj city [Internet] Shenakht J Psychol psychiatry. 2016;3:80–88. [cited 2017 Mar 3] Available from: http://shenakht.muk.ac.ir/browse.php?a_code=A-10-250-1&slc_lang=en&sid=1&sw=irritable+bowel. [Google Scholar]
- 14.Campbell-Sills L, Cohan SL, Stein MB. Relationship of resilience to personality, coping, and psychiatric symptoms in young adults. Behav Res Ther. 2006;44:585–599. doi: 10.1016/j.brat.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 15.Smith BW, Dalen J, Wiggins K, et al. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15:194–200. doi: 10.1080/10705500802222972. [DOI] [PubMed] [Google Scholar]
- 16.Park SH, Videlock EJ, Shih W, et al. Adverse childhood experiences are associated with irritable bowel syndrome and gastrointestinal symptom severity. Neurogastroenterol Motil. 2016;28:1252–1260. doi: 10.1111/nmo.12826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Videlock EJ, Adeyemo M, Licudine A, et al. Childhood Trauma Is Associated With Hypothalamic-Pituitary-Adrenal Axis Responsiveness in Irritable Bowel Syndrome [Internet] Gastroenterology. 2009;137:1954–1962. doi: 10.1053/j.gastro.2009.08.058. Available from: http://dx.doi.org/10.1053/j.gastro.2009.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bradford K, Shih W, Videlock EJ, et al. Association between early adverse life events and irritable bowel syndrome. [Internet] Clin Gastroenterol Hepatol. 2012;10:385–90. doi: 10.1016/j.cgh.2011.12.018. –3.[cited 2017 Jan 6] Available from: http://www.cghjournal.org/article/S1542356511013334/fulltext. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Videlock EJ, Shih W, Adeyemo M, et al. The effect of sex and irritable bowel syndrome on HPA axis response and peripheral glucocorticoid receptor expression [Internet] Psychoneuroendocrinology. 2016;69:67–76. doi: 10.1016/j.psyneuen.2016.03.016. Available from: http://dx.doi.org/10.1016/j.psyneuen.2016.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chang L. The role of stress on physiologic responses and clinical symptoms in irritable bowel syndrome. [Internet] Gastroenterology. 2011;140:761–5. doi: 10.1053/j.gastro.2011.01.032. [cited 2017 Jan 6] Available from: http://www.gastrojournal.org/article/S0016508511000874/fulltext. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Longstreth GF, Thompson WG, Chey WD, et al. Functional bowel disorders. [Internet] Gastroenterology. 2006;130:1480–91. doi: 10.1053/j.gastro.2005.11.061. [cited 2016 Nov 8] Available from: http://www.gastrojournal.org/article/S0016508506005129/fulltext. [DOI] [PubMed] [Google Scholar]
- 22.Patrick DL, Drossman DA, Frederick IO, et al. Quality of Life in Persons with Irritable Bowel Syndrome Development and Validation of a New Measure. 1998;43:400–411. doi: 10.1023/a:1018831127942. [DOI] [PubMed] [Google Scholar]
- 23.Bremner DJ, Bolus R, Mayer EM. Psychometric Properties of the Early Trauma Inventory – Self Report. 2007;195:211–218. doi: 10.1097/01.nmd.0000243824.84651.6c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 25.Cohen S, Kamarck T, Mermelstein R. A Global Measure of Perceived Stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 26.Goldberg LR, Johnson JA, Eber HW, et al. The international personality item pool and the future of public-domain personality measures. J Res Pers. 2006;40:84–96. [Google Scholar]
- 27.Donnellan MB, Oswald FL, Baird BM, et al. The mini-IPIP scales: tiny-yet-effective measures of the Big Five factors of personality [Internet] Psychol Assess. 2006;18:192–203. doi: 10.1037/1040-3590.18.2.192. Available from: http://dx.doi.org/10.1037/1040-3590.18.2.192%5Cnhttp://www.ncbi.nlm.nih.gov/pubmed/16768595%5CnC:%5CUsers%5CChristopherLeifeld%5CDocuments%5CCitavi 4%5CProjects%5CDissCL%5CCitaviFiles%5CDonnellan,Oswaldetal2006-Themini-IPIPscales.pdf. [DOI] [PubMed] [Google Scholar]
- 28.Costa PT, McCrae RR. Normal personality assessment in clinical practice: The NEO Personality Inventory. [Internet] Psychol Assess. 1992;4:5–13. [cited 2017 Mar 3] Available from: http://doi.apa.org/getdoi.cfm?doi=10.1037/1040-3590.4.1.5. [Google Scholar]
- 29.Johannesson E, Simrén M, Strid H, et al. Physical Activity Improves Symptoms in Irritable Bowel Syndrome: A Randomized Controlled Trial [Internet] Am J Gastroenterol. 2011;106:915–922. doi: 10.1038/ajg.2010.480. [cited 2017 Mar 3] Available from: http://www.ncbi.nlm.nih.gov/pubmed/21206488. [DOI] [PubMed] [Google Scholar]
- 30.Mikolajczak M, Roy E, Luminet O, et al. Resilience and hypothalamic-pituitary-adrenal axis reactivity under acute stress in young men. 2017:3890. doi: 10.1080/10253890701850262. [DOI] [PubMed] [Google Scholar]
- 31.Ruiz-Robledillo N, Romero-Martínez A, Moya-Albiol L. Lower cortisol response in high-resilient caregivers of people with autism: the role of anger [Internet] Stress Heal. 2016 doi: 10.1002/smi.2713. [cited 2017 Mar 3] Available from: http://doi.wiley.com/10.1002/smi.2713. [DOI] [PubMed]
- 32.Smith SM, Vale WW. The role of the hypothalamic-pituitary-adrenal axis in neuroendocrine responses to stress. [Internet] Dialogues Clin Neurosci. 2006;8:383–95. doi: 10.31887/DCNS.2006.8.4/ssmith. [cited 2017 Mar 3] Available from: http://www.ncbi.nlm.nih.gov/pubmed/17290797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mayer EA, Tillisch K. The brain-gut axis in abdominal pain syndromes. [Internet] Annu Rev Med. 2011;62:381–96. doi: 10.1146/annurev-med-012309-103958. [cited 2017 Mar 3] Available from: http://www.ncbi.nlm.nih.gov/pubmed/21090962. [DOI] [PMC free article] [PubMed] [Google Scholar]


