Abstract
Background
Due to the importance of pain control after abdominal surgery, several methods such as transversus abdominis plane (TAP) block are used to reduce the pain after surgery. TAP blocks can be performed using various ultrasound-guided approaches. Two important approaches to do this are ultrasound-guided lateral and posterior approaches. This study aimed to compare the two approaches of ultrasound-guided lateral and posterior TAP blocks to control pain after cesarean section.
Materials and methods
In this double-blind clinical trial study, 76 patients scheduled for elective cesarean section were selected and randomly divided into two groups of 38 and underwent spinal anesthesia. For pain management after the surgery, one group underwent lateral TAP block and the other group underwent posterior TAP block using 20cc of ropivacaine 0.2% on both sides. Pain intensity was evaluated based on Numerical Analog Scale (NAS) at rest and when coughing, 2, 4, 6, 12, 24 and 36 hours after surgery.
Results
The pain at rest in the posterior group at all hours post surgery was lower than the lateral group, especially at 6, 12 and 24 hours after the surgery and the difference was statistically significant (p=0.03, p<0.004, p=0.001).
Conclusion
The results of this study show that ultrasound-guided posterior TAP block compared with the lateral TAP block was more effective in pain control after cesarean section.
Keywords: posterior TAP block, lateral TAP block, ultrasound, ropivacaine, cesarean section, ultrasound
Introduction
Patients undergoing gynecologic and midwifery surgeries with cross-section incision in the lower abdomen have severe pain, especially in the first 2 days after surgery.1–3 Various approaches such as opioids, epidural catheter insertion and abdominal blocks have been used to reduce postoperative pain. The most common method of analgesics administration after surgery is applying a multi-modal approach using opioids and non steroidal anti inflammatory drugs, but the use of opiates has side effects such as respiratory depression, nausea and vomiting, urinary retention and constipation.4,5 Using pain control approaches without the use of opioids is effective in improving the quality of post-surgical recovery.4 Transversus abdominis plane (TAP) block can reduce the need for morphine after abdominal surgery including cesarean section.6,7
To perform ultrasound-guided TAP block there are many approaches such as lateral TAP block and posterior TAP block. Posterior approach was also effective in reducing the use of opioid analgesics after surgery but previous studies have not properly investigated the quality of analgesia, duration of analgesia and dosage of postoperative opioid consumption between these two approaches.8
This study aimed to compare the two approaches of ultrasound-guided lateral and posterior TAP blocks in terms of pain control and level of opioid consumption after cesarean section.
Materials and methods
This randomized double-blind clinical trial study was registered in the Iranian registry of clinical trials (IRCT2016120431225N1). The principle of the study protocol was approved by the Ethic Committee of Iran University of Medical Sciences. The study population included pregnant women referred to the University Hospital for cesarean section. Inclusion criteria were 18- to 45-year-old American Society of Anesthesiologists (ASA) class I pregnant women who underwent cesarean section with spinal anesthesia. The method of the study and advantages and potential disadvantages of the block methods were explained to the participants and those who gave written consent entered the study. The sample size calculation formula was: n=([Zα/2+Zβ]2×2[standard deviation]2/[µ1–µ2]2) where n=sample size required in each group, µ1=mean pain score in posterior TAP block, µ2=mean pain score at second post-operation hour in lateral TAP block group, µ1–µ2=clinically significant difference, Zα/2: 5% level of significance (1.96), Zβ: 95% power (1.96) and standard deviation=1.195. Since no previous study was available on this subject, a pilot study was performed among 10 patients (5 in each group) in which µ1 was measured as 4.25 and µ2 as 5. Therefore, n was calculated as 30 for each group which gave us a total sample size of 60. Then, to account for a 25% drop among patients the final sample size was decided to be 76. Sampling was stopped after reaching the required number of patients. Then, the 76 patients were randomly divided into two groups (N=38). Exclusion criteria included: lack of written consent, drug abuse, allergic reactions to local anesthetics, BMI >35, weigh less than 60 kg, coagulopathies and requiring general anesthesia. Spinal anesthesia was administered to all women and pulse oximetry monitoring, non invasive blood pressure, electrocardiogram and fluid therapy were carried out with 500 cc of Ringer’s lactate solution. Patients were turned to the left lateral position and were administered spinal anesthesia in sterile conditions using 25-G needle with 10 mg of 0.5% ropivacaine (Molteni, Italy). The operation was started after attaining a T4 sensor blockade.
In the event of a >30% decrease in systolic blood pressure, or a systolic blood pressure <80 mm Hg, 10 mg of ephedrine (Darupakhsh co, Iran) was injected bolus. In case of a heart rate below 50 beats per minute, atropine 0.5 mg (Alborzdaru, Iran) was injected. Fluid therapy and calculation of blood transfusions were performed using the ASA method.9 In case of nausea and vomiting 4 mg of ondansetron was slowly injected. After the cesarean and during the recovery, the patients were divided into two groups based on the Block Randomization Table. When the spinal anesthesia sensory level dropped for three levels after patients arrived to recovery room (this evaluation was performed using pinprick method and cotton alcohol on the anterior abdominal area) for one group the lateral TAP block was performed and for the other group ultrasound-guided bilateral posterior TAP block (Sonosite S-Nerve Ultrasound System) was performed using linear probes (6–15MHz) with 40 cc of ropivacaine 0.2% (Ropivacaine Molteni, Italy). The anesthesiologist performing the block was aware of the block type and recorded it, but the patient and the anesthesiology residents were blinded to the intervention (lateral or posterior TAP block). The anesthesiology residents assessed the patients postoperatively, absolutely unaware of the block types. To perform the lateral TAP blocks, the patient was in supine position. Then the ultrasound probe was located in the midaxillary line and local anesthetic injection was administered between the two muscle layers of the internal oblique and transverse abdominis. For posterior TAP block, the patient was turned to the semi-lateral position, the probe was located across the posterior axillary area and local anesthetic was injected in the posterior junction of the transverse abdominal plane and the anterolateral border of the quadratus lumborum muscle. The success of the injection was confirmed by the spread of local anesthetic under fascia.
Pain intensity according to the Numerical Analog Scale (NAS) at rest and while coughing along with nausea and vomiting were analyzed and recorded at 2, 4, 6, 12, 24 and 36 hours after TAP block.
The amount of drug used for analgesia in the first 36 hours after surgery, the first request for pain relief medication by the patient, complications during block including bleeding, peritoneal injection, needle breaking, liver injury and infection were recorded.
Patients’ analgesic satisfaction 36 hours after surgery was measured as: 0=weak, 1=medium, 2=good, 3=very good and 4=excellent. Pain control in these patients was performed using multi-modal method; so that in addition to lateral abdominal block, 1 g apotel (Acetaminophen, UniPharma, Greece) was also injected intravenously every 8 hours within 15 minutes and 25 mg of meperidine (Caspiantamin, Iran) was injected intravenously in case of NAS >3.
Statistical analysis
To compare the two groups, Student’s t-test for continuous variables and Chi-square test for categorical variables were used. All analyses were performed using IBM SPSS for Windows version 19, with a two-tailed p<0.05 being considered significant.
Results
From a total of 79 randomly selected patients who were candidates for cesarean section, 3 were excluded according to exclusion criteria and 76 cases entered the study. The patients were randomized into two groups of posterior TAP block and lateral TAP block each with 38 subjects (Figure 1).
Figure 1.
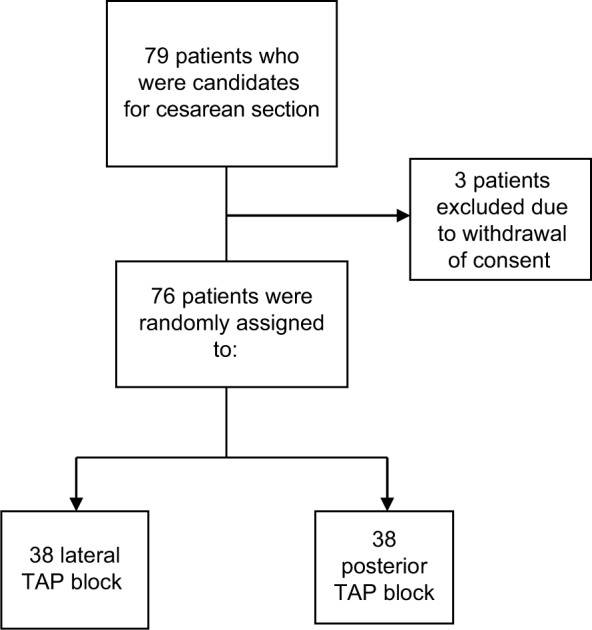
The study participant’s selection flowchart.
Abbreviation: TAP, transversus abdominis plane.
Characteristics of the study participants according to their group are shown in Table 1. As illustrated there was no significant difference regarding the age and weight of the participants as well as the frequency of comorbidities among two groups. Table 2 shows the mean of NAS scores in resting position in different hours after surgery according to posterior and lateral block groups. NAS was significantly lower in the posterior block group 6, 12 and 24 hours after operation; 2.65 (0.62) vs 2.94 (0.51), p=0.03, 3.15 (0.67) vs 4.63 (0.75), p<0.001 and 3.47 (0.76) vs 4.02 (0.85), p=0.004, respectively. Mean values of coughing NAS scores according to posterior and lateral block groups are shown in Table 3 and only the 12-hour postoperative coughing NAS score was significantly lower in the posterior block group (p<0.001). Table 4 shows the level of patients’ postoperative satisfaction among posterior and lateral block groups. Overall, patients’ satisfaction was significantly higher in the posterior group (p=0.012). As illustrated in Table 5, patients in the posterior group requested significantly less postoperative analgesics and regarding the time of their request, it took a significantly longer time for patients in the posterior group to request analgesics. Finally, comparing the incidence of nausea after surgery, no significant difference was observed between two groups (p=0.74).
Table 1.
Baseline characteristics of the study participants in the posterior and lateral block groups
| Variables | Posterior block, N=38 | Lateral block, N=38 | p-value |
|---|---|---|---|
| Age, years | 29.2 (4.46) | 29.5 (4.99) | 0.79 |
| Weight, kg | 78.1 (7.30) | 76.0 (9.16) | 0.27 |
| Comorbidities, % | 0.07 | ||
| Hypertension | 5.3 | 5.3 | – |
| Diabetes | 2.6 | 5.3 | – |
| None | 92.1 | 89.5 | – |
Notes: Data are presented as mean (±SD). p-values are calculated using Student’s t-test or Chi-square tests as appropriate.
Table 2.
Means of postoperative NAS scores of the posterior and lateral block groups in resting position
| Postoperative resting NAS scores, hours | Posterior block | Lateral block | p-value |
|---|---|---|---|
| 2 | 1.39 (0.49) | 1.60 (0.63) | 0.11 |
| 4 | 2.34 (0.53) | 2.55 (0.64) | 0.12 |
| 6 | 2.65 (0.62) | 2.94 (0.51) | 0.03 |
| 12 | 3.15 (0.67) | 4.63 (0.75) | <0.001 |
| 24 | 3.47 (0.76) | 4.02 (0.85) | 0.004 |
| 36 | 4.71 (0.69) | 4.84 (0.85) | 0.46 |
Notes: Data are presented as mean (±SD). p-values are calculated using Student’s t-test.
Abbreviation: NAS, Numerical Analog Scale.
Table 3.
Mean values of postoperative NAS scores of the posterior and lateral block groups while coughing
| Post-op coughing NAS scores, hours | Posterior block | Lateral block | p-value |
|---|---|---|---|
| 2 | 1.55 (0.68) | 1.71 (0.73) | 0.33 |
| 4 | 3.18 (0.69) | 3.44 (0.68) | 0.10 |
| 6 | 3.52 (0.68) | 3.78 (0.47) | 0.56 |
| 12 | 3.92 (0.63) | 5.81 (0.80) | <0.001 |
| 24 | 4.26 (0.75) | 4.63 (0.81) | 0.46 |
| 36 | 6.07 (0.81) | 6.05 (0.80) | 0.88 |
Notes: Data are presented as mean values (±SD). p-values are calculated using Student’s t-test.
Abbreviation: NAS, Numerical Analog Scale.
Table 4.
Level of patients’ 36-hour postoperative analgesic satisfaction among posterior and lateral block groups
| Postoperative level of satisfaction | Posterior block, % | Lateral block, % | p-value |
|---|---|---|---|
| Excellent | 5.3 | 0 | 0.012 |
| Very good | 47.4 | 18.4 | |
| Good | 28.9 | 57.9 | |
| Moderate | 18.4 | 23.7 |
Notes: Data are presented as frequency. p-values are calculated using Chi-square test.
Table 5.
Mean of postoperative time of first requirement for analgesics (hour) and mean meperidine requirement (mg) 36 hours after surgery among posterior and lateral groups
| Variable | Posterior block | Lateral block | p-value |
|---|---|---|---|
| Hours post-op | 13.3 (2.32) | 6.73 (2.91) | <0.001 |
| Meperidine dose (mg) | 29.2 (10.7) | 41.8 (18.5) | 0.002 |
Notes: Data are presented as mean (±SD). p-values are calculated using Student’s t-test.
Discussion
According to the results of previous studies, the efficacy of using local anesthesia has been shown to reduce the need for analgesic medications and to reduce pain after surgery.4 Using TAP block for pain reduction after cesarean section and hysterectomy improved the recovery of these patients.7,10 Based on the results of this study, ultrasound-guided posterior TAP block compared with the lateral TAP block was more effective in pain control after cesarean section, and created a longer analgesia with higher patient satisfaction; the mean values of pain score of posterior TAP block was lower in all intervals after surgery but only the 12-hour postoperative coughing NAS score was significantly lower in the posterior TAP block group (p<0.001) and the summation of excellent and very good satisfaction scores was 52.7% in the posterior vs 18.4% in the lateral TAP group, this result was shown the better effect of posterior TAP block in clinical situation. In terms of longer duration of analgesia our results were in line with the results of the meta-analysis by Abdallah et al.7 In addition, patients in the posterior TAP block group required lower dose of drugs during the 36 hours after the cesarean section. In a study by Rafi et al in 2001,11–13 the TAP block was conducted by anatomical landmark and triangle of petit resulting in a better analgesia in lower parts of the abdomen; however, using anatomical landmarks for this block method has a higher risk of complications such as nerve and organ damage.
Due to the use of ultrasound in blocks, truncal blocks can be simply performed with low frequency of side effects.13 One of the main causes of pain after laparoscopic surgery in gynecologic surgery seems to be visceral pain originating from the uterus and vagina. According to one theory, local anesthetic used in posterior TAP block approach enters paravertebral space and blocks sympathetic pathway resulting in relieved visceral pain.14 The pain relief and higher effect of this method compared to the other method reduces drug consumption and is consequently associated with less side effects.16
In a meta-analysis conducted by Abdallah et al,8 the length of analgesic effect in the posterior and lateral approaches of the transversus abdominal blocks in the surgery of the lower transverse abdominal sections were evaluated. Both posterior and lateral approaches were examined. The study included 12 papers with 641 patients. Four papers examined the posterior approach and 8 papers examined the lateral approach. The researchers found that the posterior approach was more effective in reducing postoperative pain at rest after surgery and in the dynamic state and provided longer analgesia than the lateral approach. In addition, it reduced morphine consumption 48 hours after the surgery. The results of the above analysis are consistent with the results of the present study. Numerous reasons are assumed for the difference:
First, injection in posterior areas probably results in the transversus abdominal block of lateral cutaneous branches of thoracolumbar nerve before branching or anastomosis and entering the TAP.17–20
Second, the posterior approach and not the lateral approach spreads the local anesthetic regionally and in a retrograde fashion in paravertebral space covering from T4 to L1 within 4 hours after injection and potentially blocks a few degrees along the thoracolumbar sympathetic system.21,22 Evidence suggests that due to the role of sympathetic nervous system in pain immediately after surgery, probably this is the reason for the posterior approach to achieve faster and longer analgesic effect.
Finally, the posterior injection probably causes the formation of a depot or focus for the local anesthetic in the neurofascial TAP plain. This warehouse of local anesthetic may probably justify the better effect of the posterior approach.23,24
Conclusion
The results of this study show that ultrasound-guided posterior block TAP in a multi-modal approach for pain control after cesarean section is more suitable than the lateral TAP block and creates a longer duration of analgesia and a higher patient satisfaction rate of the patients.
Footnotes
Author contributions
SHRF and PR participated in the study concept and design. MGA and PD performed analysis and interpretation of data. Drafting of the manuscript was conducted by PD and MRA. PR, PD and FI preformed the revision of the manuscript for important intellectual content, and statistical analysis. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Angle P, Halpern S, Leighton B, Szalai JP, Gnanendran K, Kronberg J. A randomized controlled trial examining the effect of naproxen on analgesia during the second day after cesarean delivery. Anesth Analg. 2002;95(3):741–745. doi: 10.1097/00000539-200209000-00038. [DOI] [PubMed] [Google Scholar]
- 2.Gilron I, Orr E, Tu D, O’Neill JP, Zamora J, Bell A. A placebo-controlled randomized clinical trial of perioperative administration of gabapentin, rofecoxib and their combination for spontaneous and movement-evoked pain after abdominal hysterectomy. Pain. 2005;113(1–2):191–200. doi: 10.1016/j.pain.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 3.Fassoulaki A, Stamatakis E, Petropoulos G, Siafaka I, Hassiakos D, Sarantopoulos C. Gabapentin attenuates late but not acute pain after abdominal hysterectomy. Eur J Anaesthesiol. 2006;23(2):136–141. doi: 10.1017/S0265021505002048. [DOI] [PubMed] [Google Scholar]
- 4.White PF. The changing role of non-opioid analgesic techniques in the management of postoperative pain. Anesth Analg. 2005;101(5 Suppl):S522. doi: 10.1213/01.ANE.0000177099.28914.A7. [DOI] [PubMed] [Google Scholar]
- 5.Cousins MJ, Lynch ME. The declaration montreal: access to pain management is a fundamental human right. Pain. 2011;152(12):2673–2674. doi: 10.1016/j.pain.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 6.McDonnell JG, O’Donnell B, Curley G, Heffernan A, Power C, Laffey JG. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: a prospective randomized controlled trial. Anesth Analg. 2007;104(1):193–197. doi: 10.1213/01.ane.0000250223.49963.0f. [DOI] [PubMed] [Google Scholar]
- 7.McDonnell JG, Curley G, Carney J, et al. The analgesic efficacy of transversus abdominis plane block after cesarean delivery: a randomized controlled trial. Anesth Analg. 2008;106(1):186–191. doi: 10.1213/01.ane.0000290294.64090.f3. [DOI] [PubMed] [Google Scholar]
- 8.Abdallah FW, Laffey JG, Halpern SH, Brull R. Duration of analgesic effectiveness after the posterior and lateral transversus abdominis plane block techniques for transverse lower abdominal incisions: a meta-analysis. Br J Anaesthes. 2013;111(5):721–735. doi: 10.1093/bja/aet214. [DOI] [PubMed] [Google Scholar]
- 9.Practice guidelines for perioperative blood transfusion and adjuvant therapies: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Blood Transfusion and Adjuvant Therapies. Anesthesiology. 2006;105(1):198–208. doi: 10.1097/00000542-200607000-00030. [DOI] [PubMed] [Google Scholar]
- 10.Carney J, McDonnell JG, Ochana A, Bhinder R, Laffey JG. The trans-versus abdominis plane block provides effective postoperative analgesia in patients undergoing total abdominal hysterectomy. Anesth Analg. 2008;107(6):2056–2060. doi: 10.1213/ane.0b013e3181871313. [DOI] [PubMed] [Google Scholar]
- 11.Rafi AN. Abdominal field block: a new approach via the lumbar triangle. Anaesthesia. 2001;56(10):1024–1026. doi: 10.1046/j.1365-2044.2001.02279-40.x. [DOI] [PubMed] [Google Scholar]
- 12.Hebbard P. TAP block nomenclature. Anaesthesia. 2015;70(1):112–113. doi: 10.1111/anae.12970. [DOI] [PubMed] [Google Scholar]
- 13.Long JB, Birmingham PK, De Oliveira GS, Jr, Schaldenbrand KM, Suresh S. Transversus abdominis plane block in children: a multicenter safety analysis of 1994 cases from the PRAN (Pediatric Regional Anesthesia Network) database. Anesth Analg. 2014;119(2):395–399. doi: 10.1213/ANE.0000000000000284. [DOI] [PubMed] [Google Scholar]
- 14.Veline C, Le Hetet H, Le Roux A, et al. Comparison between ultra-soundguided transversus abdominis plane and conventional ilioinguinal/iliohypogastric nerve blocks for daycase open inguinal hernia repair. Br J Anaesth. 2011;106(3):380–386. doi: 10.1093/bja/aeq363. [DOI] [PubMed] [Google Scholar]
- 15.Walter CJ, Maxwell-Armstrong C, Pinkney TD, et al. A randomised controlled trial of the efficacy of ultrasound-guided transversus abdominis plane (TAP) block in laparoscopic colorectal surgery. Surg Endosc. 2013;27(7):2366–2372. doi: 10.1007/s00464-013-2791-0. [DOI] [PubMed] [Google Scholar]
- 16.Yoshiyama S, Ueshima H, Sakai R, Otake H. A posterior TAP block provides more effective analgesia than a lateral TAP block in patients undergoing laparoscopic gynecologic surgery: a retrospective study. Anesthesiol Res Pract. 2016;2016:5. doi: 10.1155/2016/4598583. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 17.Jankovic ZB, du Feu FM, McConnell P. An anatomical study of the transversus abdominis plane block: location of the lumbar triangle of Petit and adjacent nerves. Anesth Analg. 2009;109(3):981–985. doi: 10.1213/ane.0b013e3181ae0989. [DOI] [PubMed] [Google Scholar]
- 18.Rozen WM, Tran TM, Ashton MW, Barrington MJ, Ivanusic JJ, Taylor GI. Refining the course of the thoracolumbar nerves: a new understanding of the innervation of the anterior abdominal wall. Clin Anat. 2008;21(4):325–333. doi: 10.1002/ca.20621. [DOI] [PubMed] [Google Scholar]
- 19.Hebbard PD. Transversalis fascia plane block, a novel ultrasoundguided abdominal wall nerve block. Can J Anaesth. 2009;56(8):618–620. doi: 10.1007/s12630-009-9110-1. [DOI] [PubMed] [Google Scholar]
- 20.Hebbard P, Barrington M, Vasey C. Ultrasound-guided continuous oblique subcostal transversus abdominis plane blockade: description of anatomy and clinical technique. Reg Anesth Pain Med. 2010;35(5):436–431. doi: 10.1097/aap.0b013e3181e66702. [DOI] [PubMed] [Google Scholar]
- 21.Carney J, Finnerty O, Rauf J, Bergin D, Laffey J, Mc Donnell J. Studies on the spread of local anaesthetic solution in transversus abdominis plane blocks. Anaesthesia. 2011;66(11):1023–1030. doi: 10.1111/j.1365-2044.2011.06855.x. [DOI] [PubMed] [Google Scholar]
- 22.Finnerty O, McDonnell JG. Transversus abdominis plane block. Curr Opin Anaesthesiol. 2012;25(5):610–614. doi: 10.1097/ACO.0b013e328357b165. [DOI] [PubMed] [Google Scholar]
- 23.Latzke D, Marhofer P, Kettner SC, et al. Pharmacokinetics of the local anesthetic ropivacaine after transversus abdominis plane block in healthy volunteers. Eur J Clin Pharmacol. 2012;68(4):419–425. doi: 10.1007/s00228-011-1139-8. [DOI] [PubMed] [Google Scholar]
- 24.Griffiths JD, Barron FA, Grant S, Bjorksten AR, Hebbard P, Royse CF. Plasma ropivacaine concentrations after ultrasound-guided transversus abdominis plane block. Br J Anaesth. 2010;105(6):853–856. doi: 10.1093/bja/aeq255. [DOI] [PubMed] [Google Scholar]


