Abstract
Coronary artery fistula (CAF) is an uncommon anomaly that is usually congenital but can be acquired. Although most patients are asymptomatic, some may present with congestive heart failure, infective endocarditis, myocardial ischemia or rupture. In the past, surgical ligation was the only option in the management of CAF, but since 1983, transcatheter closure of CAF has been increasing as an alternative to surgery. We report a 3-year-old boy, presented in Queen Alia Heart Institute, who underwent successful transcatheter closure of a large fistula communicating the distal part of the right coronary artery to the right ventricle. Our case differs from other CAFs in that the fistula was communicating the right coronary artery itself to the right ventricle.
Keywords: Coronary artery fistula, Right ventricle, Vascular plug
Introduction
Coronary artery fistula (CAF) is a direct communication between a coronary artery and a cardiac chamber, great vessels as well as vascular structure [1]. It is a rare disease of coronary arteries, which can cause a significant hemodynamic problems depending on the size, exit chamber and its relationship to the native coronary artery. It occurs in around 0.002% of general population [2].
Around 50% of CAF patients are asymptomatic, picked up with an incidental heart murmur whereas others may present with acute myocardial ischemia, angina pectoris, and infective endocarditis [3].
In this case report, we present a percutaneous closure of right coronary artery fistula to the right ventricle in a 3-year-old male patient.
Case report
The patient was a 3-year-old boy, born at full term, one of identical twins following an uneventful pregnancy and cesarean delivery. He presented in the neonatal period with attack of tachypnea and feeding difficulties with normal O2 saturation. Cross sectional echocardiogram at the neonatal period showed right coronary artery (RCA) fistula to the right ventricle (RV). The patient was asymptomatic during the regular follow-up until age 3 years; he started complaining of effort intolerance with profuse sweating after minimal activity. Echocardiography (ECG) showed the same CAF with mild dilatation of the right heart. The patient was started on furosemide and planned for cardiac catheter.
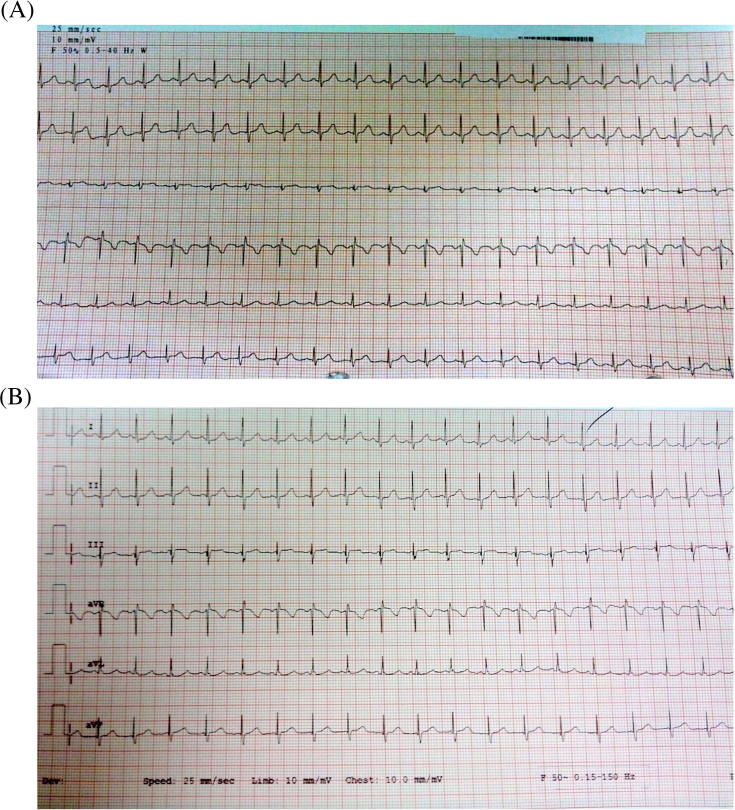
On clinical examination, the patient looked well, not in failure, with no visible impulse, and with soft S1 and S2 and continuous murmur grade 3/6, at the third intercostal space. ECG showed sinus tachycardia with no evidence of myocardial ischemia (Figure 1). Coronary arteries computed tomography angiogram showed RCA ectasia and RCA fistula to the RV.
Figure 1.
(A). Echocardiography before coronary artery fistula closure. (B) Echocardiography after coronary artery fistula closure, shows no changes in ST and T waves.
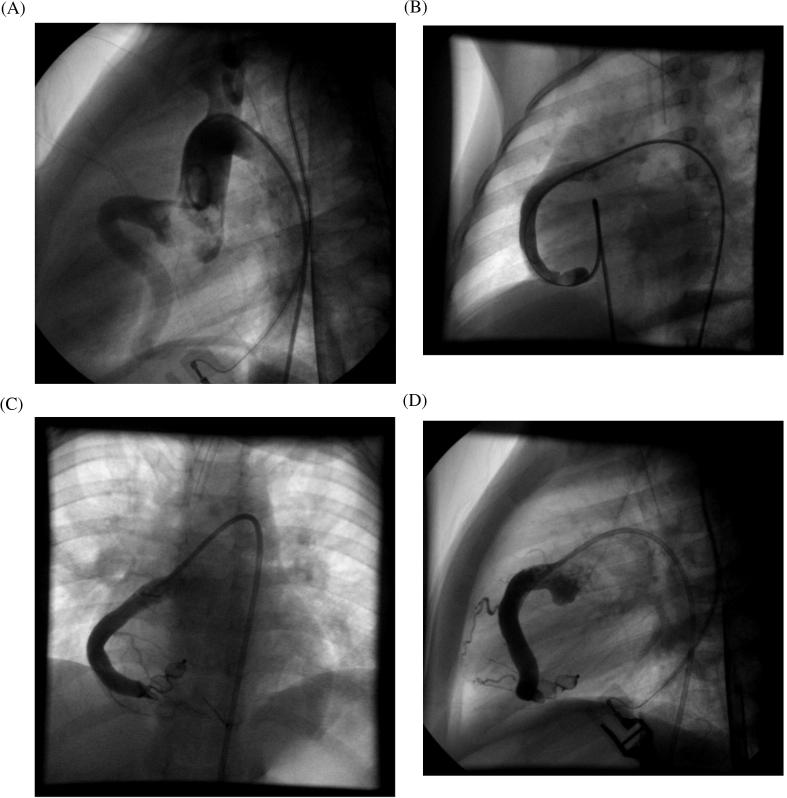
Under general anesthesia, cardiac catheterization was done using right femoral vein and artery. Firstly, hemodynamic data were collected, pressures were taken in the left ventricle, aortic root, and RV. The pulmonary to systemic shunt ratio was 2:1. Aortic root angiography showed a patent nondominant left coronary artery with normal branches and the RCA was dilated, gave rise to RCA branches but continued as fistula, which exited in the RV. The fistula was classified as distal type fistula from native RCA [4]. The anatomy and dimension of coronary arteries and fistula were determined using selective coronary angiograms. The diameter of the fistula’s waist at RV exit was 6.5 mm. Having created an arteriovenous circuit through the fistula to facilitate crossing, balloon occlusion was applied firstly to precisely identify all distal coronary branches (Figure 2) and secondly to get accurate details and dimensions of the fistula in order to decide on a landing zone and the appropriate type and size of device for occlusion, preserving all the native coronary branches to the myocardium. Based on the anatomy of the fistulae, we used the AMPLATZER vascular plug type II (AVP2-010) 10 mm diameter and 7 mm length, deployed by Guide 6F catheter. The device deployment was performed retrograde via the femoral artery placing the AVPII distally close to the exit point in the RV. An angiogram was done after device deployment and no immediate complications were noted (Figures 2C and 2D). The patient was extubated immediately postprocedure and started on heparin continuous infusion and warfarin. The patient was discharged home after 3 days with international normalized ratio 1.8 on warfarin and aspirin.
Figure 2.
(A) Aortic root angiogram with right coronary artery fistula. (B) Balloon occlusion test. (C) Angiogram after device deployment; anterior–posterior view. (D) Angiogram after device deployment; lateral view.
The patient was followed with daily ECG and international normalized ratio in the first 3 days postprocedure, then every 2 weeks for 1 month, then monthly. No ECG changes (Fig. 1), and no leaking through the device have been noted during follow up. The patient was on warfarin for 4 months then switched to Plavix and aspirin.
Discussion
CAF is a rare disease, accounting for 0.2–0.4% of congenital cardiac anomalies [5]. The major site of origin is from RCA in 55% of patients, 35% from the left coronary artery, and less commonly from the circumflex artery. Very rarely, CAFs can be bilateral. The major receiving chamber is the RV in 45%, followed by the right atrium in 25%, pulmonary artery 15%, and less commonly the coronary sinus 7%. Complications related to the CAF are present in 11% of patients younger than 20 years and in 35% of patients older than 20 years. Congestive heart failure is presented in 30.8% of children with CAF [6]. For this reason, elective closure of a significant CAF at a young age is recommended to prevent complication at time of presentation [7].
CAFs are thought to be formed as result from persistence of sinusoidal connection between the lumens of primitive tubular heart that supply myocardial blood flow in the early embryonic period [1].
A small fistula does not cause any hemodynamic compromise, while large fistulae can cause coronary artery steal phenomenon, which leads to ischemia; the latter can give rise to chest pain, arrhythmias, or mitral valve insufficiency [7]. The pathophysiologic mechanism of CAF is reduction in myocardial blood flow, which is related to the diastolic pressure gradient and runoff from the coronary vascular to the low pressure receiving cavity. In large fistulas, the intracoronary diastolic perfusion pressure becomes progressively diminished. As a compensation, the coronary artery enlarges leading to an increase in the risk of myocardial ischemia beyond the origin of fistula [5].
The management of CAF in children is still controversial, spontaneous closure has been reported in one patient secondary to thrombus [3], otherwise surgical closure was traditionally viewed as the main therapeutic method with good outcome, but around 76.9% of patients needed cardiopulmonary bypass [6]. Since 1983 transcatheter closure of CAF has widely been used with good results. Several reports have evaluated the efficacy and safety of early transcatheter closure of CAF using coils, umbrella, or AMPLATZER Duct occlusion devices. Compared with early surgical closure of CAF, transcatheter is simple and helpful in minimizing surgical complications such as bypass complication, postoperative care, wound management, and scar formation [2], [5], [7], [8], [9], [10].
Our case is different because the RCA was the fistula itself, which gave the branches of the RCA. We follow the same technique using right femoral vein and artery; the anatomy and dimension of coronary arteries and fistula were determined using selective coronary angiograms. A balloon occlusion test within the fistula was applied mainly to identify all distal coronary branches precisely. An arteriovenous loop was created to cross easily through the fistula. Using the AMPLATZER vascular plug type 2, which needs a small size delivery system deployment, the fistula was successfully closed and the device deployment was performed retrograde via the femoral artery. An angiogram was done after device deployment, and no immediate complication has been reported.
Medical follow-up with daily ECG in the first 3 days, then every 2 weeks, showed no ST-T wave changes and no leaking was notice on follow-up two-dimensional ECG.
Conclusion
The transcatheter closure of coronary fistula in children is a safe alternative to surgical closure. We reported a successful transcatheter closure of fistula communicating the distal part of the right coronary artery to the right ventricle in a 3 year old boy with no complications, and no scar as well as low cost in comparing to surgical closure.
Conflicts of interest
All authors declare no conflicts of interest.
Disclosure: Authors have nothing to disclose with regard to commercial support.
Footnotes
Peer review under responsibility of King Saud University.
References
- 1.Gupta M. Coronary Artery Fistula http://emedicine.medscape.com/article/895749-overview#showall: emedicine.medscape; 2015 [updated Jan 27, 2015]. Available from: http://emedicine.medscape.com/article/895749-overview#showall.
- 2.Gribaa R., Slim M., Ouali S., Neffati E., Boughzela E. Transcatheter closure of a congenital coronary artery to right ventricle fistula: a case report. J Med Case Rep. 2014;8:432. doi: 10.1186/1752-1947-8-432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Koneru J., Samuel A., Joshi M., Hamden A., Shamoon F.E., Bikkina M. Coronary anomaly and coronary artery fistula as cause of angina pectoris with literature review. Case Rep Vasc Med. 2011;2011:486187. doi: 10.1155/2011/486187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gowda S.T., Forbes T.J., Singh H., Kovach J.A., Prieto L., Latson L.A. Remodeling and thrombosis following closure of coronary artery fistula with review of management. Catheter Cardiovasc Interv. 2013;82:132–142. doi: 10.1002/ccd.24699. [DOI] [PubMed] [Google Scholar]
- 5.Noble S., Basmadjian A., Ibrahim R. Transcatheter closure of coronary artery fistulas. Rev Esp Cardiol. 2009;62:1316. doi: 10.1016/s1885-5857(09)73358-4. [DOI] [PubMed] [Google Scholar]
- 6.Yim D., Yong M.S., d’Udekem Y., Brizard C.P., Konstantinov I.E. Early surgical repair of the coronary artery fistulae in children: 30 years of experience. Ann Thorac Surg. 2015;100:188–194. doi: 10.1016/j.athoracsur.2015.02.044. [DOI] [PubMed] [Google Scholar]
- 7.Armsby L.R., Keane J.F., Sherwood M.C., Forbess J.M., Perry S.B., Lock J.E. Management of coronary artery fistulae: patient selection and results of transcatheter closure. J Am Coll Cardiol. 2002;39:1026–1032. doi: 10.1016/s0735-1097(02)01742-4. [DOI] [PubMed] [Google Scholar]
- 8.Zhu X.Y., Zhang D.Z., Han X.M., Cui C.S., Sheng X.T., Wang Q.G. Transcatheter closure of congenital coronary artery fistulae: immediate and long-term follow-up results. Clin Cardiol. 2009;32:506–512. doi: 10.1002/clc.20650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rammos S., Apostolopoulou S.C., Kiaffas M.G. Transcatheter closure of large-sized coronary artery fistula. Hosp Chron. 2008;3(1 Suppl):103–107. [Google Scholar]
- 10.Song-Hua L., Ren-Hua S., Yang L., Shao-Ping C., Rong-Liang X., Yong-Wen Q. Transcatheter interventional therapy of congenital coronary artery fistula. Heart. 2015;101:A35. [Google Scholar]