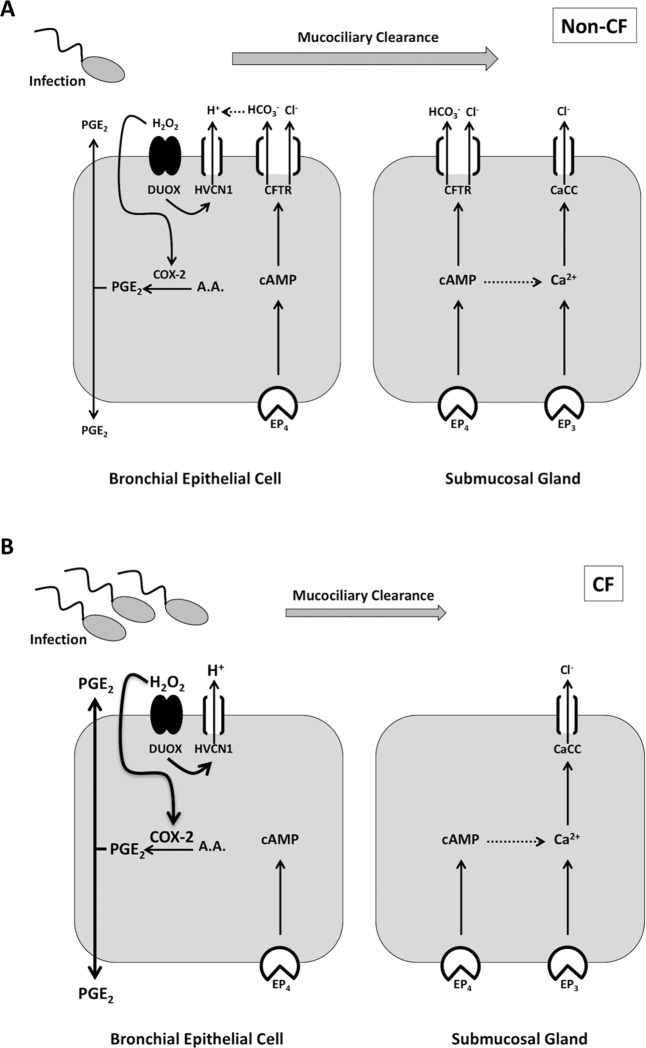
Fig 8. Simplified working model of PGE2-stimulated Cl- and HCO3- secretion and mucociliary clearance in non-CF and CF airway.
A. In the airway, microbial infections cause an increase in PGE2 through release from infiltrating inflammatory cells (not pictured) and production by airway epithelia via COX-2 activation. H2O2 produced by DUOX activates COX-2 and HVCN1 channels provide the H+ shunt from H2O2 production. PGE2 exits the cell and activates PGE2 (EP) receptors. In the current study we did not examine specific EP receptor involvement, however, we propose that EP4 is the predominant mediator of serosal PGE2 stimulation in bronchial epithelial cells. Submucosal gland cells may also utilize the EP3 receptor, or Ca2+-activated Cl- channels (CaCC) may get activated via EP4-mediated cAMP-Ca2+ crosstalk. In bronchial epithelial cells, PGE2 stimulates Cl- and HCO3- secretion via CFTR, whereas in submucosal glands, both CFTR and CaCC are activated. Cl- and HCO3- secretion will then influence airway pH, mucus properties, hydration, and ultimately, mucociliary clearance. B. In CF airway, lack of CFTR-dependent Cl- and HCO3- secretion in bronchial epithelial cells, coupled with no HCO3- secretion and decreased Cl- secretion from submucosal glands, leads to an acidic airway pH, thick-adherent mucus, and decreased mucociliary clearance. This results in increased microbial infection and rampant inflammation, in part by increased PGE2 production.