Abstract
Background
China has a large population with cardiovascular disease (CVD) that requires extensive self-management. Mobile health (mHealth) apps may be a useful tool for CVD self-management. Little is currently known about the types and quality of health information provided in Chinese CVD mobile apps and whether app functions are conducive to promoting CVD self-management.
Objective
We undertook a systematic review to evaluate the types and quality of health information provided in Chinese CVD mobile apps and interactive app functions for promoting CVD self-management.
Methods
Mobile apps targeting end users in China with CVD conditions were selected in February 2017 through a multi-stage process. Three frameworks were used to evaluate the selected apps: (1) types of health information offered were assessed using our Health Information Wants framework, which encompasses 7 types of information; (2) quality of information provided in the apps was assessed using the 11 guidelines recommended by the National Library of Medicine of the National Institutes of Health; and (3) types of interactive app functions for CVD self-management were assessed using a 15-item framework adapted from the literature, including our own prior work.
Results
Of 578 apps identified, 82 were eligible for final review. Among these, information about self-care (67/82, 82%) and information specifically regarding CVD (63/82, 77%) were the most common types of information provided, while information about health care providers (22/82, 27%) and laboratory tests (5/82, 6%) were least common. The most common indicators of information quality were the revealing of apps’ providers (82/82, 100%) and purpose (82/82, 100%), while the least common quality indicators were the revealing of how apps’ information was selected (1/82, 1%) and app sponsorship (0/82, 0%). The most common interactive functions for CVD self-management were those that enabled user interaction with the app provider (57/82, 70%) and with health care providers (36/82, 44%), while the least common interactive functions were those that enabled lifestyle management (13/82, 16%) and psychological health management (6/82, 7%). None of the apps covered all 7 types of health information, all 11 indicators of information quality, or all 15 interactive functions for CVD self-management.
Conclusions
Chinese CVD apps are insufficient in providing comprehensive health information, high-quality information, and interactive functions to facilitate CVD self-management. End users should exercise caution when using existing apps. Health care professionals and app developers should collaborate to better understand end users’ preferences and follow evidence-based guidelines to develop mHealth apps conducive to CVD self-management.
Keywords: mobile health, mHealth, cardiovascular disease, CVD, patient preferences, information quality, self-management, mobile applications, mobile apps, China
Introduction
Cardiovascular disease (CVD) is a leading cause of morbidity and mortality in China, accounting for 45% of all deaths in rural areas and 42% in urban areas [1]. Currently, approximately 290 million people in China live with CVD [2]. Meanwhile, there is a severe shortage of doctors in China, where the doctor-patient ratio is 1.4 doctors per 1000 patients [3]. Mobile health (mHealth) apps therefore hold promise for delivering health information and services to Chinese patients, especially for chronic conditions like CVD, which require extensive self-management [4]. Self-management is key to person-centered care [5], but its support requires an understanding of individual preferences for different types of health information and decision-making autonomy [6]. The Health Information Wants (HIW) framework suggests 7 types of information that patients typically desire in health care contexts: (1) information about the specific health condition, (2) treatment, (3) laboratory tests, (4) self-care, (5) complementary and alternative medicine (CAM), (6) psychosocial aspects, and (7) health care providers (HCPs) [6-8]. Empirical research using the HIW framework has shown that diabetes-related mobile apps for Mainland Chinese users offer inadequate information [9]. However, little is currently known about whether Chinese CVD mobile apps might offer a broad range of high-quality information and functions that can facilitate effective CVD self-management.
The self-management of chronic conditions requires the ability “to manage the symptoms, treatment, physical and psychosocial consequences and life style changes inherent in living with a chronic condition” [10]. Self-management is inherent to person-centered care that promotes a “balanced consideration of the values, needs, expectations, preferences, capacities, and health and well-being of all the constituents and stakeholders of the health care system” [5]. Effective self-management and person-centered care require full accommodation of people’s needs and preferences for different types and amounts of information and other care services [11,12], a degree of autonomy in health-related decision-making [13,14], and support from their formal (eg, health care professionals) and informal caregivers (eg, family members) [15,16].
Although mHealth apps have the potential to promote effective self-management and person-centered care [17,18], existing apps tend to provide limited types of information [9], lack information quality assurance [19-21], and offer inadequate functionalities [22]. These limitations may have negative impacts on mHealth app users. Information quality is important to users of electronic health (eHealth) and mHealth products or services [23,24]. However, the quality of online health information is often unregulated and problematic [25], especially in the context of mHealth apps [23,24]. The situation is even worse in developing countries, including China [26-28]. One study, for example, has found that the quality of Chinese mHealth apps is poor, especially due to limited coverage of medication topics [29]. Another study found that Chinese mHealth apps tend to lack information accountability and have limited coverage of relevant topics [30]. Empirical evidence also suggests that concerns about privacy and information quality could hinder Chinese people’s mHealth app usage [31].
Nevertheless, mobile apps’ interactive functions have the potential to assist users in their health care activities and improve user satisfaction [32-34]. A randomized controlled trial undertaken in Sweden, for example, found that an interactive health app was more effective than a noninteractive tool for improving medication adherence, lifestyle changes, and quality of life [35]. However, little is currently known about the types of interactive functions in Chinese CVD apps and whether they might meet existing guidelines for promoting CVD self-management; even studies that have focused on Chinese CVD-related apps have not considered these characteristics [21,30].
In the present study, we assessed (1) the types of health information that Chinese CVD apps offer, (2) the quality of information available in the apps, and (3) the apps’ interactive functions for promoting CVD self-management.
Methods
We selected the mobile apps for this study in multiple steps. First, in February 2017, we conducted searches on the Chinese website for the iTunes App Store, using predetermined search terms consistent with New York State Department of Health definitions of CVD [36] and based on our research team’s knowledge of the terms that Chinese people typically use when describing CVD-related conditions (one of our research team members, a surgeon, specializes in CVD-related conditions and has practiced in China for over 20 years). The use of lay people’s search terms enabled us to obtain the types of apps that people in China would typically find in their own searches (see Textbox 1).
Chinese search terms used.
心脏病 (heart diseases)
心脑血管 (cardiovascular diseases)
中风 (stroke)
卒中 (stroke)
冠心病 (coronary artery disease)
高血压 (high blood pressure)
偏瘫 (paralysis)
The initial search yielded 578 results. After we removed duplicates, 464 apps remained. Next, we reviewed the titles and descriptions of the remaining apps in iTunes and included those that: (1) targeted Mainland China; (2) had full text in simplified Chinese characters (used in Mainland China); (3) targeted end users/patients/the general public; and (4) covered at least one CVD condition. Apps that did not meet all four of these criteria were excluded. A total of 98 apps remained in the review.
Finally, we downloaded (or attempted to download) each of the 98 apps to an iPhone for further examination. During this step, we found that 16 of the apps were not accessible or downloadable, so they too were excluded. The final sample consisted of 82 apps that could be downloaded and installed for further examination (see Figure 1).
Figure 1.
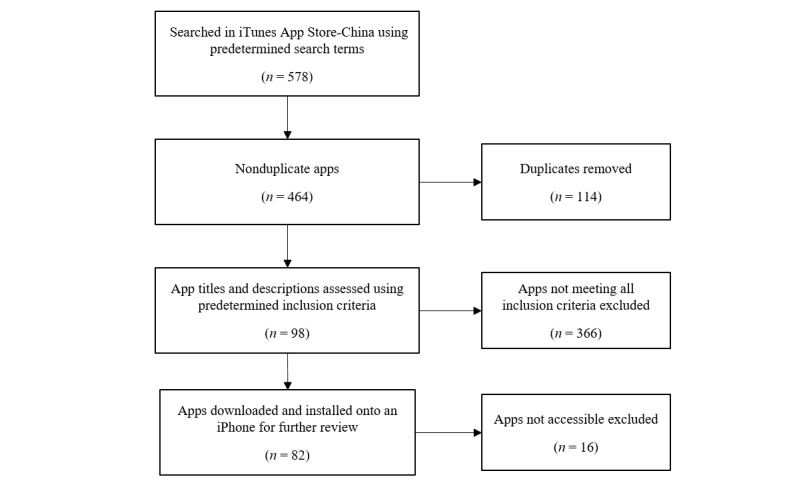
App selection process.
After downloading and installing the 82 apps onto an iPhone to simulate Chinese end users’ experiences, we used the HIW framework, the National Library of Medicine’s (NLM’s) guidelines, and our own self-management framework to systematically evaluate the apps’ (1) information types, (2) information quality, and (3) interactive functions for self-management, respectively. One researcher (a trained graduate research assistant) first coded five apps using these frameworks. The coding results were verified by another researcher (a faculty member experienced with this type of research). Differences between these two researchers were resolved through discussions. The research assistant then completed the coding for all apps in the final sample, with the faculty member randomly verifying 10% of the results; differences were again resolved through discussions. The research assistant then revised relevant coding based on the discussions.
The Health Information Wants Framework for Evaluating the Types of Information
We adapted the HIW framework [37] to assess the types of health information provided in the apps. As stated in the introduction, this framework covers 7 types of health information commonly wanted by patients in health care encounters; based on the descriptions for each type and subtype from our earlier studies [9,37], we adapted items to apply to CVD specifically, when necessary (eg, information about the type of diabetes was changed to information about the type of CVD). The presence of each type of health information was recorded as 1, and each absence was recorded as 0 (scoring range: 0-7). The higher the score, the more types of information identified in the apps.
The National Library of Medicine Framework for Evaluating Quality of Information
Based on the NLM guidelines [38], we developed operational definitions to determine the quality of the apps’ information. This framework includes 11 indicators of information quality; the presence of each indicator was recorded as 1, and each absence was recorded as 0 (scoring range: 0-11). The higher the score, the higher the app’s information quality (Table 1).
Table 1.
National Library of Medicine guidelines for information quality and our operational definitions.
| NLM guideline | Operational definitions |
| Providing information on who is in charge of the app | Provides information that could help users understand who is in charge of the app (eg, information about the app provider’s name). Such information is typically found via the About Us button in the app and/or on the app’s iTunes page. |
| Providing information about why the app is being provided | Provides information that could help users understand the app’s purpose, intended users, and functionalities. Such information is typically found on the app’s iTunes page and/or via the About Us button in the app (eg, indicating that the app is developed for CVDa patients, or to provide CVD-related information, or to provide one-on-one consultation with a CVD physician). |
| Providing the app provider’s physical address | Provides information about the physical address of app developer or administrator. |
| Providing information on the source of the app’s information | Provides information that could help users understand where the information used by the app came from (eg, an article or book with author names, or, for Web-based information, the website from which the information was retrieved). |
| Providing information on how the app’s content was selected | Provides a logical explanation for how the app’s information was selected (eg, information selected from peer-reviewed journals). |
| Having expert review of the information | Provides information to make clear that information presented in the app has been reviewed by qualified health care professionals. |
| Financial disclosure | Provides information on where the money to support an app comes from (eg, government agencies, nonprofit organizations, drug companies). This information could help users understand whether the app’s providers have financial motives that users should be aware of (eg, the sale of CVD drugs). |
| Content is up-to-date | The original NLMb guidelines did not specify what timeframe would be considered up-to-date; in our study, we operationalized this indicator as app content updated in the past 3 months. |
| Does not have advertisements | Whether or not an app contains advertisements. Note: if a drug or treatment option mentioned in an app was a part of scientific results (eg, if reported in a research article) then it was not considered an advertisement. |
| Does not use unbelievable or emotional claims | Whether or not an app makes claims that are too good to be true, or are based on emotions instead of scientific facts (eg, “Lose 30 pounds in 2 weeks!”). |
| Does not ask for personal information | Whether or not users must submit personal information (eg, name, phone number, email address) in order to use certain app functions. |
aCVD: cardiovascular disease.
bNLM: National Library of Medicine.
The Self-Management Framework for Evaluating Interactive App Functions
A major advantage of mobile apps is that they enable user input (eg, recording of physical activities) and interaction with others (eg, HCPs, families, and peers) that are key to effective self-management. Current app evaluation frameworks tend to focus on limited interactive functions. For instance, the Mobile Apps Review Scale [39] narrowly defines interactivity within the parameters of user input, feedback, and prompts, with no consideration of other important interactive functions (eg, virtual rewards, online-offline integration, family involvement). Hale et al [40] developed an evaluation framework to assess the congruency between apps’ intervention strategies and user needs. However, their framework was designed to assess apps’ topics (eg, healthy eating) and intervention strategies (eg, self-monitoring); it did not offer a systematic way to evaluate the scope of interactive app functions (the authors mention only briefly that self-monitoring, social support, modelling/vicarious learning, and stimulus control are highly interactive strategies that an app can adopt) [40].
Based on the literature on strategies for effective self-management of chronic conditions [4,6,7,9,10,41-43] as well as the aforementioned frameworks for evaluating mobile apps [39,40], we developed our 15-item Self-Management Framework for Evaluating Interactive App Functions (SFEIAF) to specifically assess interactive functions that are necessary for effective CVD self-management in CVD apps. We did not, however, include providing information as an app function in our SFEIAF, even though providing relevant information to ensure patient education is essential for effective self-management. This decision was based on two reasons: (1) the function of providing patient education information is already fully covered in our HIW framework, which focuses specifically on a broad range of health information; and (2) the typical approach to providing patient education information is top-down, such that information flows from the app developer to the user with no input from the user. In contrast, our SFEIAF emphasizes user input in information provision that is essential to effective self-management. The presence of each function in the SFEIAF was recorded as 1, and each absence was recorded as 0 (scoring range: 0-15). The higher the score, the more the interactive functions in an app (Table 2).
Table 2.
Interactive app functions in the Self-Management Framework for Evaluating Interactive App Functions and their operational definitions.
| Interactive app function | Our operational definition |
| Monitoring of physical or health indicators | Functions that allow users to record and monitor their health or physical indicators (eg, body mass index, blood pressure) |
| Exercise and physical activity management | Functions that enable users to record and monitor their exercise and physical activities (eg, interactive pedometers) |
| Lifestyle management | Functions that enable users to record and monitor aspects of their lifestyles relevant to the prevention of, or coping with, CVDa (eg, monitoring of alcohol drinking) |
| Medication management | Functions that enable users to manage their medication (eg, when to take what medicine as prescribed) |
| Interaction with health care providers | Functions that enable the user to interact with HCPsb (eg, consultation via the app) |
| Condition management or prevention | Functions (other than medication management) that enable user input or interaction to control or prevent CVD (eg, hypertension self-detector) |
| Psychological health management | Functions that enable users to understand or manage their psychological health (eg, self-evaluation of psychological health) |
| Peer interaction | Functions that enable users to interact with other users with similar health conditions (eg, in-app peer support groups) |
| Family involvement | Functions that enable users to include family in their CVD self-management |
| Virtual rewards/gamification | Functions that provide motivational or gamification functions to encourage user commitment to their CVD self-management (eg, virtual rewards to encourage medication adherence) |
| Personal health records management | Functions that enable user input of their health-related data (eg, electronic health profiles) |
| Individualized care management | Functions that enable tailoring of prompts based on user input (eg, care recommendations tailored to users’ specific health conditions) |
| Multiple platform care management | Functions that enable users to connect their CVD care concerns across multiple platforms (eg, short message reminders sent from the app to other apps or electronic services such as email) |
| Online-offline integration | Functions that enable users to connect and integrate their online and offline self-management activities (eg, connecting the app with a blood glucose device to manage one’s blood sugar level) |
| Interaction with the app provider | Functions that enable users to communicate with, and receive feedback from, the app provider. Depending on the questions that users ask, this type of interaction could involve technical support (eg, questions about how to use the app) or medical issues (eg, CVD-specific questions). |
aCVD: cardiovascular disease.
bHPCs: health care providers.
Results
Types of Information
Ten of the 82 (10/82, 12%) apps in our final sample received scores of zero, because they offered none of the 7 types of information in the HIW framework; 15 (15/82, 18%) received scores of 1-2 (ie, they offered 1 or 2 types of information); 27 (27/82, 33%) offered 3 or 4 types; and 30 (30/82, 37%) offered 5 or 6 types of information. No app offered all 7 types of information. Self-care was the most commonly offered type of information (67/82, 82%), followed by information about the specific health condition (63/82, 77%) and treatment (55/82, 67%); information about laboratory tests (5/82, 6%) was the least common (Table 3).
Table 3.
Types of health information covered by Chinese CVD apps.
| Type of health information | n (%) |
| Self-care | 67 (82) |
| Health-condition specific | 63 (77) |
| Treatment | 55 (67) |
| Complementary and alternative medicine | 34 (42) |
| Psychosocial aspects | 29 (35) |
| Health care providers | 22 (27) |
| Laboratory tests | 5 (6) |
Quality of Information
Nineteen (19/82, 23%) of the apps received scores of 2-3 (ie, they met 2 or 3 NLM guidelines for information quality). Sixty-two (62/82, 75%) met 4-6 guidelines, and only one app (1/82, 1%) met 8; no app met more than that. The most commonly-met NLM guidelines were those that addressed providing information about the apps’ developers (82/82, 100%) and purpose (82/82, 100%). The least commonly-met guideline was that which addressed disclosing the app’s source of financial support; none of the apps did this (Table 4).
Table 4.
National Library of Medicine’s information quality indicators covered by the apps.
| Information quality indicator | n (%) |
| Provided information on who is in charge of the app | 82 (100) |
| Provided information about why the app is being provided | 82 (100) |
| Does not use unrealizable, emotional, or sensational language | 67 (82) |
| Does not have advertisements | 46 (56) |
| App content is up-to-date | 35 (43) |
| Does not ask for personal information | 30 (37) |
| Provided information on the source of the app’s information | 5 (6) |
| Provided the app provider’s physical address | 3 (4) |
| Expert review of the information selected in the app | 3 (4) |
| Provided information on how the app’s content was selected | 1 (1) |
| Financial support disclosure | 0 (0) |
Interactive App Functions for Self-Management
Nine (9/82, 11%) apps scored zero on the interactive app functions for self-management (ie, they offered none of the 15 interactive functions for CVD self-management specified in the SFEIAF). Twenty-nine apps (29/82, 35%) scored 1-3, offering 1-3 functions; 21 (21/82, 26%) offered 4-6, 12 (12/82, 15%) offered 7-9; 7 (7/82, 9%) offered 10-12; and only 4 (4/82, 5%) offered 13 functions. No app offered more than 13 functions. The most commonly offered interactive function was interaction with the app provider (57/82, 70%), and the least commonly offered was psychological health management (6/82, 7%; Table 5).
Table 5.
Interactive app functions for self-management.
| Interactive app function | n (%) |
| Interaction with the app provider | 57 (70) |
| Interaction with health care providers | 36 (44) |
| Online-offline integration | 34 (42) |
| Multiple platform care management | 33 (40) |
| Monitoring of physical or health indicator | 28 (34) |
| Personal health records management | 28 (34) |
| Condition management or prevention | 27 (33) |
| Individualized care management | 26 (32) |
| Family involvementa | 20 (24) |
| Peer interaction | 19 (23) |
| Virtual rewards/gamification | 19 (23) |
| Medication management | 18 (22) |
| Exercise and physical activity management | 15 (18) |
| Lifestyle management | 13 (16) |
| Psychological health management | 6 (7) |
aFamily involvement included app features that enabled user-designated family members to access user information in the app and allowed app developers to directly send family members information (eg, general health education information related to users’ health conditions, reminders of important things for users to do, and emergency alerts).
Follow-Up Analysis Results
In September 2017, following reviewers’ feedback, we performed follow-up analyses on app purposes. The definitions and results are reported in Table 6. At this point, 13 of the 82 original apps were no longer available; thus, these analyses were based on a sample of 69 apps.
Table 6.
App purposes.
|
Category |
Definition |
n (%)a |
| Health education | App has a function that aims to provide information and resources that could inform people about CVDb conditions | 44 (64) |
| Self-management | App has a function that aims to help users’ own monitoring and management of their health | 36 (52) |
| CVD risk evaluation | App has a function that aims to provide a calculator for users to assess their odds of developing one or more CVD conditions | 13 (19) |
| Interaction with health care providers | App has a function that aims to facilitate user-health care provider communications, including making appointments and having face-to-face or virtual one-on-one medical consultations | 35 (51) |
| Interaction with peers | App has a function that aims to allow users to communicate and bond with other users with similar health conditions | 9 (13) |
| Family involvement | App has a function that aims to involve users’ family members in the care management process | 12 (17) |
| Selling products and services | App has a function that aims to sell products (eg, medications) and services (eg, housekeeping services) to users | 7 (10) |
aWe coded an app into multiple categories if it had multiple purposes, so the total percentage exceeds 100% (27 of the apps, or 39%, were coded as having a single purpose; the remaining 42 apps each had multiple purposes).
bCVD: cardiovascular disease.
In October 2017, we further examined the types of providers in charge of the apps in our final sample. Of the 69 apps that we had examined in the previous month, only 59 were still available. Of these, 48 (48/59, 81%) were developed by for-profit companies (46 by information technology/software companies; 2 by pharmaceutical companies), and 11 (11/59, 19%) were developed by individuals with no clear connection to any organization. No app in this sample was developed by government agencies or nonprofit organizations. We also analyzed the type of CVD on which the apps focused: 20 (20/59, 34%) of the apps focused on general heart health monitoring/management; 17 (17/59, 29%) on hypertension; 9 (9/59, 15%) on stroke; 6 (6/59, 10%) on diabetes; 6 (6/59, 10%) on coronary heart disease; and 1 (1/59, 2%) on heart failure.
Discussion
Self-management is key to person-centered care, which acknowledges the importance of respecting people’s health care preferences for types and amounts of health information and social interactions (eg, family involvement in care) in their own health or disease management [9-11,13]. Effective self-management requires the building of a safe and shared care environment that can meet people’s information wants, their desires to make their own decisions, and their desires for high-quality health care and social interactions [14-16,25].
mHealth apps have the potential to assist self-management of many health conditions [17,18]. However, to ensure that mobile apps can adequately meet the wide range of users’ information wants [9,12], needs for high-quality information and care access [19,20], and self-management decision-making, evidence-based insights are needed to bridge current knowledge gaps [14,16,22]. Such insights could guide research and practice in China. In the Chinese health app market, the number of technology and health app users is growing exponentially [44,45], yet the quality of Chinese mHealth apps appears to be inferior to that of those in developed countries [27-29], and research on the current development of Chinese CVD apps has so far been limited [29,30].
In this study, we have systematically assessed (1) the types of health information that Chinese CVD apps offer, (2) the quality of health information available in the apps, and (3) the apps’ interactive functions for promoting self-management. The results show that none of the reviewed apps offered all 7 types of information specified in the HIW framework, met all 11 NLM guidelines for information quality, or provided all 15 of the SFEIAF’s interactive functions for promoting CVD self-management. Given that CVD self-management requires a variety of information [46], a lack of comprehensive information may hinder CVD self-management. For example, of all apps that were reviewed, only 5 offered information about laboratory tests, yet such information is crucial for patients [47].
None of the apps revealed sources of financial support or sponsorship, and very few revealed information about the selection of the apps’ content, app providers’ physical addresses, or the sources of the apps’ content. Over 60% of the apps asked for users’ personal information without a clear indication of how such information would be stored or used. Privacy concerns might affect app usage [48], so Chinese health app developers should integrate privacy protection measures into their future app designs. Overall, Chinese CVD apps fail to provide sufficient information for users to evaluate apps’ information quality.
Nine of the CVD apps offered none of the 15 interactive functions for self-management. This finding is troublesome, because a major advantage of mHealth apps is their ability to facilitate user input in managing their own health care [49,50]. This finding for Chinese apps, along with similar findings reported in studies of English-language mHealth apps [51,52], suggests that the same challenge exists across national/cultural boundaries. No app in our study offered more than 13 interactive functions for CVD self-management. Furthermore, although psychological health is closely associated with CVD conditions [53], only 7% (6/82) of the apps offered interactive functions that might facilitate self-management of psychological health. Given that individuals with CVD conditions or concerns may have to deal with comorbid psychological stress or other mental discomfort [54,55], it is important that this feature is addressed in future app design as well.
Facilitating family involvement is important in chronic disease self-management [56], especially in Chinese society, where the patient’s family traditionally plays a major role [57]. In China, family involvement is often considered integral to, and indispensable for, individuals’ health care [58,59]. A lack of functionality for family involvement might disconnect app users’ online self-management from the offline family-centered management of their condition. However, only 24% of the apps in our study had functions that enabled family involvement. Future app development should strive to include functions for family involvement, and should investigate and compare the efficacy of different interactive functions for family involvement to provide more guidance for app development (some interactive functions might work better for some users and their families, whereas others might find other functions more useful).
Limitations and Future Directions
This was a cross-sectional study. Although this study is novel in that it provides, to our knowledge, the first systematic evaluation of Chinese CVD apps’ information types, information quality, and interactive functions, it does so for a snapshot of apps available when the search was performed. Future research could examine issues at multiple time points to reveal the evolution of app development. This study only examined apps developed for iOS users in Mainland China (due to limited resources, we focused only on iOS apps available in Apple’s App Store); thus, the findings should not be generalized without caution. However, the overall findings of this study do resemble those reported in a Western context and across mobile platforms [25], suggesting that such problems may be common across different cultural/national and mobile platform contexts. Future research can apply the frameworks used in this study to examine apps in other national contexts to provide more systematic comparisons across the globe. It would also be desirable to secure research funding for researchers to purchase other types of mobile devices (eg, Android) to study mobile apps running on platforms other than iOS (it is certainly not ideal to rely completely on personal devices for data collection, as we did in this study).
Conclusions
Chinese CVD apps currently provide a limited range of high-quality information and lack sufficient interactive functions conducive to effective CVD self-management. Although family involvement in health care is expected in Chinese society, functionality for family involvement has not been adequately integrated into Chinese CVD apps. This study’s findings call for the development of more evidence-based, user-centered mHealth apps, with further systematic examination and monitoring of the apps’ abilities to provide a broad range of high-quality information and more interactive app functions to facilitate self-management of CVD.
Acknowledgments
Editorial support with manuscript development was provided by the Cain Center for Nursing Research and the Center for Transdisciplinary Collaborative Research in Self-Management Science (P30, NR015335) at The University of Texas at Austin School of Nursing.
Abbreviations
- CAM
complementary and alternative medicine
- CVD
cardiovascular disease
- eHealth
electronic health
- HCP
health care provider
- HIW
Health Information Wants
- mHealth
mobile health
- NLM
National Library of Medicine
- SFEIAF
Self-Management Framework for Evaluating Interactive App Functions
Footnotes
Conflicts of Interest: None declared.
References
- 1.National Health and Family Planning Commission . China's Health And Family Planning Statistical Yearbook 2014. Beijing: Peking Union Medical College Press; 2014. [Google Scholar]
- 2.Weiwei C, Runlin G, Lisheng L, Manlu Z, Wen W, Yongjun W, Zhaosu W, Huijun L, Zhe Z, Lixin J, Shengshou H. Outline of the report on cardiovascular diseases in China, 2014. Eur Heart J Suppl. 2016 May;18(Suppl F):F2–F11. doi: 10.1093/eurheartj/suw030. http://europepmc.org/abstract/MED/28533724. [DOI] [PubMed] [Google Scholar]
- 3.The World Bank Physicians (per 1,000 people) 2012. [2017-07-13]. http://data.worldbank.org/indicator/sh.med.phys.zs .
- 4.Gandhi S, Chen S, Hong L, Sun K, Gong E, Li C, Yan LL, Schwalm J. Effect of mobile health interventions on the secondary prevention of cardiovascular disease: systematic review and meta-analysis. Can J Cardiol. 2017 Feb;33(2):219–231. doi: 10.1016/j.cjca.2016.08.017. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization People at the Centre of Health Care: Harmonizing Mind and Body, People and Systems. 2007. http://www.wpro.who.int/publications/docs/PEOPLEATTHECENTREOFHEALTHCARE_final_lowres.pdf .
- 6.Xie B. Older adults' health information wants in the Internet age: implications for patient-provider relationships. J Health Commun. 2009 Sep;14(6):510–24. doi: 10.1080/10810730903089614. [DOI] [PubMed] [Google Scholar]
- 7.Xie B, Wang M, Feldman R, Zhou L. Exploring older and younger adults' preferences for health information and participation in decision making using the Health Information Wants Questionnaire (HIWQ) Health Expect. 2014 Dec;17(6):795–808. doi: 10.1111/j.1369-7625.2012.00804.x. http://europepmc.org/abstract/MED/22783800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xie B, Wang M, Feldman R, Zhou L. Internet use frequency and patient-centered care: measuring patient preferences for participation using the health information wants questionnaire. J Med Internet Res. 2013;15(7):e132. doi: 10.2196/jmir.2615. http://www.jmir.org/2013/7/e132/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nie L, Xie B, Yang Y, Shan YM. Characteristics of Chinese m-Health applications for diabetes self-management. Telemed J E Health. 2016 Jul;22(7):614–9. doi: 10.1089/tmj.2015.0184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Self-management approaches for people with chronic conditions: a review. Patient Educ Couns. 2002;48(2):177–87. doi: 10.1016/s0738-3991(02)00032-0. [DOI] [PubMed] [Google Scholar]
- 11.Tao D, Or CK. Effects of self-management health information technology on glycaemic control for patients with diabetes: a meta-analysis of randomized controlled trials. J Telemed Telecare. 2013 Apr 5; doi: 10.1177/1357633X13479701. [DOI] [PubMed] [Google Scholar]
- 12.Or CK, Tao D. Does the use of consumer health information technology improve outcomes in the patient self-management of diabetes? A meta-analysis and narrative review of randomized controlled trials. Int J Med Inform. 2014 May;83(5):320–9. doi: 10.1016/j.ijmedinf.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 13.Matthews J, Hall AM, Hernon M, Murray A, Jackson B, Taylor I, Toner J, Guerin S, Lonsdale C, Hurley DA. A brief report on the development of a theoretically-grounded intervention to promote patient autonomy and self-management of physiotherapy patients: face validity and feasibility of implementation. BMC Health Serv Res. 2015 Jul 05;15:260. doi: 10.1186/s12913-015-0921-1. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-015-0921-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Raaijmakers LG, Martens MK, Hesselink AE, de Weerdt I, de Vries NK, Kremers SPJ. Mastery and perceived autonomy support are correlates of Dutch diabetes patients' self-management and quality of life. Patient Educ Couns. 2014 Oct;97(1):75–81. doi: 10.1016/j.pec.2014.06.016. [DOI] [PubMed] [Google Scholar]
- 15.Watson AC. Shared decision making and self-management support: tools for empowering individuals to manage their health. Prof Case Manag. 2015;20(2):103–5. doi: 10.1097/NCM.0000000000000085. [DOI] [PubMed] [Google Scholar]
- 16.Deek H, Noureddine S, Newton PJ, Inglis SC, MacDonald PS, Davidson PM. A family-focused intervention for heart failure self-care: conceptual underpinnings of a culturally appropriate intervention. J Adv Nurs. 2016 Feb;72(2):434–50. doi: 10.1111/jan.12768. [DOI] [PubMed] [Google Scholar]
- 17.Cui M, Wu X, Mao J, Wang X, Nie M. T2DM self-management via smartphone applications: a systematic review and meta-analysis. PLoS One. 2016;11(11):e0166718. doi: 10.1371/journal.pone.0166718. http://dx.plos.org/10.1371/journal.pone.0166718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Whitehead L, Seaton P. The effectiveness of self-management mobile phone and tablet apps in long-term condition management: a systematic review. J Med Internet Res. 2016;18(5):e97. doi: 10.2196/jmir.4883. http://www.jmir.org/2016/5/e97/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nicholas J, Larsen ME, Proudfoot J, Christensen H. Mobile apps for bipolar disorder: a systematic review of features and content quality. J Med Internet Res. 2015;17(8):e198. doi: 10.2196/jmir.4581. http://www.jmir.org/2015/8/e198/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McMillan B, Hickey E, Mitchell C, Patel M. The need for quality assurance of health apps. BMJ. 2015 Nov 04;351:h5915. doi: 10.1136/bmj.h5915. [DOI] [PubMed] [Google Scholar]
- 21.Xiao Q, Wang Y, Sun L, Lu S, Wu Y. Current status and quality assessment of cardiovascular diseases related smartphone apps in China. Stud Health Technol Inform. 2016;225:1030–1. [PubMed] [Google Scholar]
- 22.Bailey SC, Belter LT, Pandit AU, Carpenter DM, Carlos E, Wolf MS. The availability, functionality, and quality of mobile applications supporting medication self-management. J Am Med Inform Assoc. 2014;21(3):542–6. doi: 10.1136/amiajnl-2013-002232. http://jamia.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=24163156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bardus M, van Beurden SB, Smith JR, Abraham C. A review and content analysis of engagement, functionality, aesthetics, information quality, and change techniques in the most popular commercial apps for weight management. Int J Behav Nutr Phys Act. 2016;13(1):35. doi: 10.1186/s12966-016-0359-9. http://ijbnpa.biomedcentral.com/articles/10.1186/s12966-016-0359-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jeon E, Park H, Min YH, Kim H. Analysis of the information quality of Korean obesity-management smartphone applications. Healthc Inform Res. 2014 Jan;20(1):23–9. doi: 10.4258/hir.2014.20.1.23. http://www.e-hir.org/journal/viewJournal.html?year=2014&vol=020&num=01&page=23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang Y, Sun Y, Xie B. Quality of health information for consumers on the web: a systematic review of indicators, criteria, tools, and evaluation results. J Assn Inf Sci Tec. 2015 Apr 29;66(10):2071–2084. doi: 10.1002/asi.23311. doi: 10.1002/asi.23311. [DOI] [Google Scholar]
- 26.Bastawrous A, Armstrong MJ. Mobile health use in low- and high-income countries: an overview of the peer-reviewed literature. J R Soc Med. 2013 Apr;106(4):130–42. doi: 10.1177/0141076812472620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hsu J, Liu D, Yu YM, Zhao HT, Chen ZR, Li J, Chen W. The top Chinese mobile health apps: a systematic investigation. J Med Internet Res. 2016 Aug 29;18(8):e222. doi: 10.2196/jmir.5955. http://www.jmir.org/2016/8/e222/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li H, Zhang T, Chi H, Chen Y, Li Y, Wang J. Mobile health in China: current status and future development. Asian J Psychiatr. 2014 Aug;10:101–4. doi: 10.1016/j.ajp.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 29.Liu Y, Chang P, Li N, Lamb KV, Wang J, Huang X, Wang Y, Wu Y. Quality of Chinese CVD medication apps. Stud Health Technol Inform. 2016;225:1036–7. [PubMed] [Google Scholar]
- 30.Xiao Q, Lu S, Wang Y, Sun L, Wu Y. Current status of cardiovascular disease-related smartphone apps downloadable in China. Telemed J E Health. 2017 Mar;23(3):219–225. doi: 10.1089/tmj.2016.0083. [DOI] [PubMed] [Google Scholar]
- 31.Liu Y, Wang L, Chang P, Lamb KV, Cui Y, Wu Y. What features of smartphone medication applications are patients with chronic diseases and caregivers looking for? Stud Health Technol Inform. 2016;225:515–9. [PubMed] [Google Scholar]
- 32.Nightingale R, Hall A, Gelder C, Friedl S, Brennan E, Swallow V. Desirable components for a customized, home-based, digital care-management app for children and young people with long-term, chronic conditions: a qualitative exploration. J Med Internet Res. 2017 Jul 04;19(7):e235. doi: 10.2196/jmir.7760. http://www.jmir.org/2017/7/e235/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Munster-Segev M, Fuerst O, Kaplan SA, Cahn A. Incorporation of a stress reducing mobile app in the care of patients with type 2 diabetes: a prospective study. JMIR Mhealth Uhealth. 2017 May 29;5(5):e75. doi: 10.2196/mhealth.7408. http://mhealth.jmir.org/2017/5/e75/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Samra S, Wu A, Redleaf M. Interactive iPhone/iPad app for increased tympanic membrane familiarity. Ann Otol Rhinol Laryngol. 2016 Dec;125(12):997–1000. doi: 10.1177/0003489416669952. [DOI] [PubMed] [Google Scholar]
- 35.Johnston N, Bodegard J, Jerström S, Åkesson J, Brorsson H, Alfredsson J, Albertsson PA, Karlsson J, Varenhorst C. Effects of interactive patient smartphone support app on drug adherence and lifestyle changes in myocardial infarction patients: A randomized study. Am Heart J. 2016 Aug;178:85–94. doi: 10.1016/j.ahj.2016.05.005. https://linkinghub.elsevier.com/retrieve/pii/S0002-8703(16)30062-X. [DOI] [PubMed] [Google Scholar]
- 36.New York State Department of Health Types of Cardiovascular Disease. 2012. https://www.health.ny.gov/diseases/cardiovascular/heart_disease/types_of_cv.htm .
- 37.Xie B, Wang M, Feldman R. Preferences for health information and decision-making: development of the Health Information Wants (HIW) questionnaire. iConference; iConference; February 8-11, 2011; Seattle. New York: ACM; 2011. pp. 273–280. [DOI] [Google Scholar]
- 38.U.S. National Library of Medicine Evaluating Internet Health Information: A Tutorial from the National Library of Medicine. 2016. [2017-07-12]. https://medlineplus.gov/webeval/webeval.html .
- 39.Stoyanov SR, Hides L, Kavanagh DJ, Zelenko O, Tjondronegoro D, Mani M. Mobile app rating scale: a new tool for assessing the quality of health mobile apps. JMIR Mhealth Uhealth. 2015;3(1):e27. doi: 10.2196/mhealth.3422. http://mhealth.jmir.org/2015/1/e27/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hale K, Capra S, Bauer J. A framework to assist health professionals in recommending high-quality apps for supporting chronic disease self-management: illustrative assessment of type 2 diabetes apps. JMIR Mhealth Uhealth. 2015;3(3):e87. doi: 10.2196/mhealth.4532. http://mhealth.jmir.org/2015/3/e87/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Meunier S, Coulombe S, Beaulieu M, Côté J, Lespérance F, Chiasson J, Bherer L, Lambert J, Houle J. Longitudinal testing of the Information-Motivation-Behavioral Skills model of self-care among adults with type 2 diabetes. Patient Educ Couns. 2016 Nov;99(11):1830–1836. doi: 10.1016/j.pec.2016.06.011. [DOI] [PubMed] [Google Scholar]
- 42.Zeng B, Sun W, Gary RA, Li C, Liu T. Towards a conceptual model of diabetes self-management among Chinese immigrants in the United States. Int J Environ Res Public Health. 2014 Jun 27;11(7):6727–42. doi: 10.3390/ijerph110706727. http://www.mdpi.com/resolver?pii=ijerph110706727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chen S, Gong E, Kazi DS, Gates AB, Karaye KM, Girerd N, Bai R, AlHabib KF, Li C, Sun K, Hong L, Fu H, Peng W, Liu X, Chen L, Schwalm J, Yan LL. Development of a mobile phone-based intervention to improve adherence to secondary prevention of coronary heart disease in China. J Med Eng Technol. 2016;40(7-8):372–382. doi: 10.1080/03091902.2016.1213904. [DOI] [PubMed] [Google Scholar]
- 44.Zhang X, Yan X, Cao X, Sun Y, Chen H, She J. The role of perceived e-health literacy in users' continuance intention to use mobile healthcare applications: an exploratory empirical study in China. Inform Technol Devel. 2017:1–26. doi: 10.1080/02681102.2017.1283286. [DOI] [Google Scholar]
- 45.Sun L, Wang Y, Greene B, Xiao Q, Jiao C, Ji M, Wu Y. Facilitators and barriers to using physical activity smartphone apps among Chinese patients with chronic diseases. BMC Med Inform Decis Mak. 2017 Apr 19;17(1):44. doi: 10.1186/s12911-017-0446-0. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-017-0446-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rief JJ, Hamm ME, Zickmund SL, Nikolajski C, Lesky D, Hess R, Fischer GS, Weimer M, Clark S, Zieth C, Roberts MS. Using health information technology to foster engagement: patients' experiences with an active patient health record. Health Commun. 2017 Mar;32(3):310–319. doi: 10.1080/10410236.2016.1138378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dennison L, Morrison L, Conway G, Yardley L. Opportunities and challenges for smartphone applications in supporting health behavior change: qualitative study. J Med Internet Res. 2013;15(4):e86. doi: 10.2196/jmir.2583. http://www.jmir.org/2013/4/e86/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wu Y, Yao X, Vespasiani G, Nicolucci A, Dong Y, Kwong J, Li L, Sun X, Tian H, Li S. Mobile app-based interventions to support diabetes self-management: a systematic review of randomized controlled trials to identify functions associated with glycemic efficacy. JMIR Mhealth Uhealth. 2017 Mar 14;5(3):e35. doi: 10.2196/mhealth.6522. http://mhealth.jmir.org/2017/3/e35/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hood M, Wilson R, Corsica J, Bradley L, Chirinos D, Vivo A. What do we know about mobile applications for diabetes self-management? A review of reviews. J Behav Med. 2016 Dec;39(6):981–994. doi: 10.1007/s10865-016-9765-3. [DOI] [PubMed] [Google Scholar]
- 50.Lithgow K, Edwards A, Rabi D. Smartphone app use for diabetes management: evaluating patient perspectives. JMIR Diabetes. 2017 Jan 23;2(1):e2. doi: 10.2196/diabetes.6643. doi: 10.2196/diabetes.6643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Scheibe M, Reichelt J, Bellmann M, Kirch W. Acceptance factors of mobile apps for diabetes by patients aged 50 or older: a qualitative study. Med 2 0. 2015 Mar 02;4(1):e1. doi: 10.2196/med20.3912. http://www.medicine20.com/2015/1/e1/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Klainin-Yobas P, Ng SH, Stephen PD, Lau Y. Efficacy of psychosocial interventions on psychological outcomes among people with cardiovascular diseases: a systematic review and meta-analysis. Patient Educ Couns. 2016 Apr;99(4):512–21. doi: 10.1016/j.pec.2015.10.020. [DOI] [PubMed] [Google Scholar]
- 53.Kim C, Park N, Choi J, Shin D. Designing an Internet-based intervention tailored to psychological factors for CVD risk reduction: role of stress and anger. Stud Health Technol Inform. 2016;225:1001–2. [PubMed] [Google Scholar]
- 54.Kachur S, Menezes AR, De Schutter A, Milani RV, Lavie CJ. Significance of comorbid psychological stress and depression on outcomes after cardiac rehabilitation. Am J Med. 2016 Dec;129(12):1316–1321. doi: 10.1016/j.amjmed.2016.07.006. [DOI] [PubMed] [Google Scholar]
- 55.Latkin CA, Knowlton AR. Social network assessments and interventions for health behavior change: a critical review. Behav Med. 2015;41(3):90–7. doi: 10.1080/08964289.2015.1034645. http://europepmc.org/abstract/MED/26332926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Peng W, Yuan S, Holtz BE. Exploring the challenges and opportunities of health mobile apps for individuals with type 2 diabetes living in rural communities. Telemed J E Health. 2016 Sep;22(9):733–8. doi: 10.1089/tmj.2015.0180. [DOI] [PubMed] [Google Scholar]
- 57.Cao Y, Chen X, Fan R. Toward a Confucian family-oriented health care system for the future of China. J Med Philos. 2011 Oct;36(5):452–65. doi: 10.1093/jmp/jhr036. [DOI] [PubMed] [Google Scholar]
- 58.Hu HH, Li G, Arao T. The association of family social support, depression, anxiety and self-efficacy with specific hypertension self-care behaviours in Chinese local community. J Hum Hypertens. 2015 Mar;29(3):198–203. doi: 10.1038/jhh.2014.58. [DOI] [PubMed] [Google Scholar]
- 59.Li G, Hu H, Dong Z, Arao T. Development of the Chinese family support scale in a sample of Chinese patients with hypertension. PLoS One. 2013;8(12):e85682. doi: 10.1371/journal.pone.0085682. http://dx.plos.org/10.1371/journal.pone.0085682. [DOI] [PMC free article] [PubMed] [Google Scholar]


