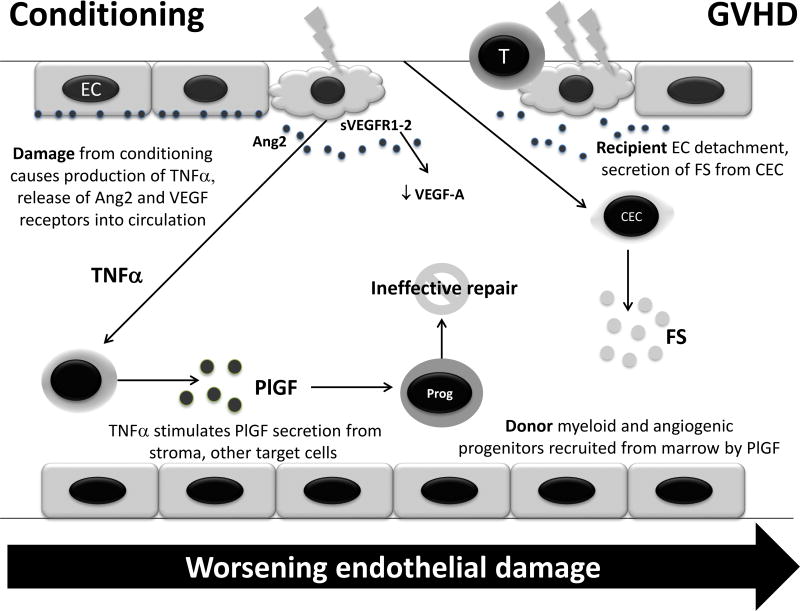
Figure 2.
Potential mechanism of alterations in levels of angiogenic factors after conditioning prior to HCT and during GVHD. Damage to endothelial cells (EC) can cause release of angiopoietin-2 (Ang2) and vascular endothelial growth factor receptors (VEGFR) 1–2, the latter of which possibly leads to sequestration of VEGF-A in circulation. Damage also increases tumor necrosis factor-alpha (TNF-α) production, leading to increased production of placental growth factor (PlGF) in target tissues. PlGF causes chemotaxis of donor myeloid and angiogenic progenitors (Prog) to repair the damage, which is not completely effective due to ongoing inflammation. This cascade is amplified in GVHD, where endothelial damage is sufficiently severe to cause circulation of endothelial cells (CEC), which release follistatin (FS) as an autocrine enhancer of proliferation. Thus, although these alterations are observed after transplant, the cascade is exaggerated in GVHD, which reflects a greater degree of endothelial damage.