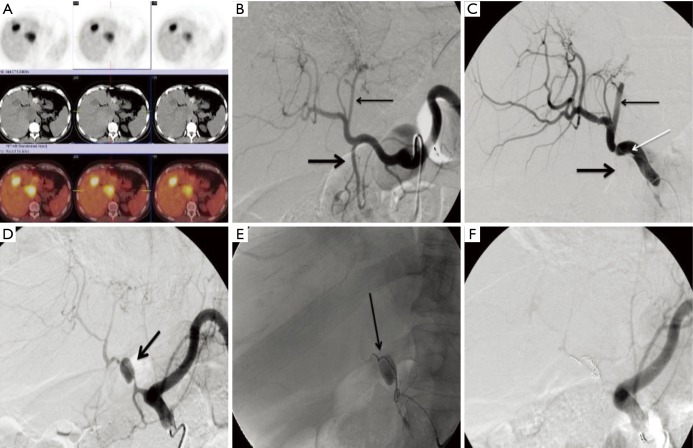
Figure 2.
Vascular injury related to biologic agents in colorectal cancer. This 70-year-old male had metastatic colorectal cancer that had progressed on first- and second-line therapies and was being treated with bevacizumab monotherapy at the time of treatment. His positron emission tomography/computed tomography scan demonstrated multiple hypermetabolic foci in the left and caudate lobes (A). Angiography was performed with the patient on bevacizumab. Celiac angiography was performed prior to and after advancing a catheter in the common hepatic artery (B, C). Following catheterization dissection flap (white arrow, C) extended from the common hepatic artery and the left lateral segment branches were occluded (thin arrow, B, C) along with the gastroduodenal artery (thick arrow, B, C). The patient was placed on clopidrogel in an attempt to avoid thrombosis of the hepatic artery and returned for another attempt to treat four weeks later. At that time (D), there was a large pseudoaneurysm (arrow, D) and the downstream arteries were attenuated, likely secondary to the underlying vascular injury. The pseudoaneurysm was embolized with coils (arrow, E) with resulting occlusion of the common hepatic artery (F). Several interventional radiologists were surveyed regarding the length of time from the last dose of bevacizumab that was considered safe to perform angiography. The consensus was 4 weeks from the date of the most recent dose with restarting 1–2 days after arteriography.