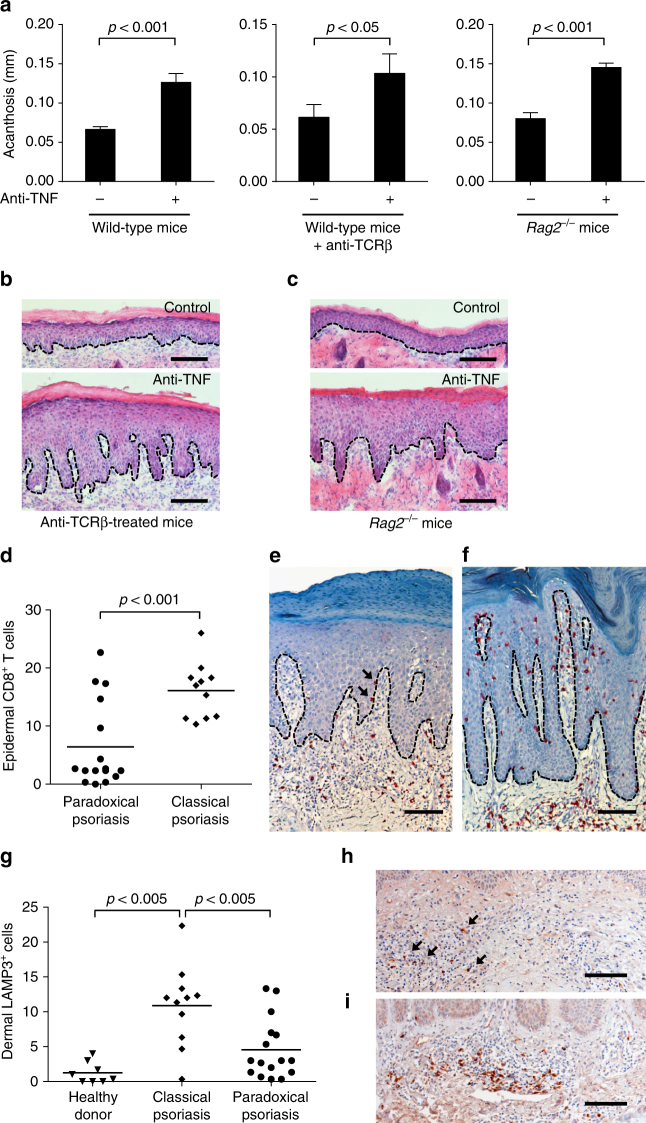
Fig. 6.
T-cell-independent induction of paradoxical psoriasis. a Quantification of acanthosis 7 days after mechanical injury of wild-type mice, wild-type mice treated with anti-TCRβ antibody, and Rag2 −/− mice, all of which were treated with or without anti-TNF antibody. b Representative HE staining of skin 7 days after mechanical injury of mice treated with anti-TCRβ antibody alone or anti-TCRβ and anti-TNF antibodies combined. c Representative HE staining of skin 7 days after mechanical injury of Rag2 −/− mice treated with or without anti-TNF antibody. d Number of epidermal CD8+ T cells per high-power field in skin lesions of patients with classical psoriasis and paradoxical psoriasis. e, f Representative CD8 staining of paradoxical psoriasis (e) and classical psoriasis (f). g Number of dermal LAMP3+ cells per high-power field in skin of healthy donors as well as in skin lesions of patients with classical psoriasis and paradoxical psoriasis. h, i Representative LAMP3-staining of paradoxical psoriasis (h) and classical psoriasis (i). Experiment depicted (in a–c) is representative for two independent experiments. Bar charts in a show mean values plus SEM of five mice each group. Dashed line in b, c, e, f, h, and i represents border between epidermis above and dermis below. Arrows point at intraepidermal CD8+ T cells in paradoxical psoriasis (e) or dermal LAMP3+ cells (h), respectively. All statistical analyses were performed with unpaired Student’s t-test. Anti-TCRβ = anti-T-cell receptor beta chain antibody