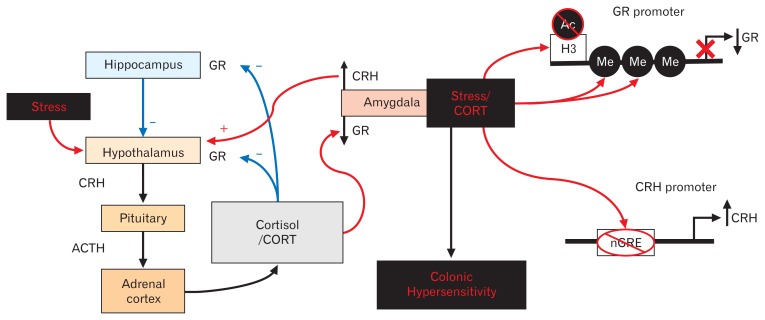
Figure 2.
Amygdala-mediated mechanisms for stress-induced colonic hypersensitivity. The body’s neuroendocrine stress response (hypothalamic-pituitary-adrenal [HPA] axis) is initiated at the hypothalamus and causes the synthesis and release of corticotropin-releasing hormone (CRH) onto the anterior pituitary. Upon binding of CRH to its type 1 receptor, the pituitary gland secretes adrenocorticotropic hormone (ACTH) into the peripheral blood circulation leading to production of cortisol in humans or corticosterone (CORT) in rodents. Following release into the circulation, CORT binds to the glucocorticoid receptor (GR) to initiate negative feedback of the HPA axis at the level of the hypothalamus and the hippocampus. In contrast, CORT binding to GR at the amygdala leads to facilitation of HPA axis, thus promoting persistent stress activation.50,52–55 In this review, we discuss our recent data showing that stress activation or implantation of a CORT micropellet at the amygdala produces persistent colonic hypersensitivity to balloon distension along with decreased GR expression and increased CRH expression.56–60 Our findings have also revealed that a decrease in GR expression could be due to increased methylation (Me) of the GR promoter along with decreased acetylation (Ac) of histone 3 (H3) at the GR promoter.61,62 The persistent decrease in GR expression decreases the binding of GR to a negative GR response (nGRE) element in the CRH promoter, thus removing GR-induced repression of CRH expression. The loss of the repression of the CRH promoter induced a persistent increase in CRH expression, and inhibiting the increase in CRH expression reversed the stress-induced colonic hypersensitivity.62