Fig. 2.
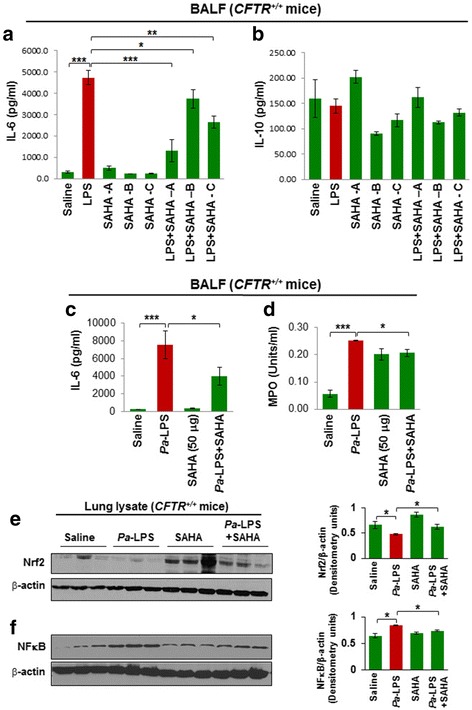
SAHA protects against Pseudomonas aeruginosa-LPS (Pa-LPS) - induced inflammatory lung disease. a, b The Cftr+/+ mice were intra-tracheally (i.t.) instilled with Pa-LPS (20 μg/mouse, n = 3), followed by SAHA treatment (100 μg/mouse in 100 μl total volume of PBS) for one (SAHA-A), two (SAHA-B) or three (SAHA-C) days, in order to standardize the correct dose and duration of SAHA treatment. The bronchoalveolar lavage fluid (BALF) was collected each day and analyzed for IL-6 and IL-10 cytokine levels by ELISA. Data shows that treatment with SAHA significantly (p < 0.05) controls Pa-LPS induced IL-6 levels at day 1, although the rescue was not very significant at day 2 or 3, implying that repeated SAHA administration might have some side effects. Moreover, even though no significant change was detected in IL-10 levels in BALF isolated from Pa-LPS treated mice compared to controls, we did observe a slight decrease, which was partially restored by SAHA treatment (Day 1), indicating that further standardization of SAHA dose is needed. c, d Based on the above preliminary data, we treated Cftr+/+ mice with i.t. SAHA (50 μg/mouse in 100 μl total volume of PBS, n = 3), for 12 h, post Pa-LPS (20 μg/mouse) challenge for another 24 h, to test the therapeutic efficacy of a lower SAHA dose. The BALF was harvested and analyzed for IL-6 (inflammation) levels and neutrophil (myeloperoxidase, MPO) activity. The data shows that even a lower dose (50 μg/mouse) of SAHA significantly controls Pa-LPS induced inflammation (IL-6) and neutrophil activity (MPO), suggesting it’s potential in controlling Pa-LPS induced pulmonary inflammation or lung disease. e, f Next, the lung tissues harvested from the above experiment (C) were used for immunoblotting. The data shows that SAHA treatment controls Pa-LPS induced inflammatory-oxidative stress by regulating Nrf2 and NFκB protein expression (p < 0.05)
