Abstract
Objectives
The aim of this study was to evaluate different anatomical variants of the anterior loop of the inferior alveolar nerve (IAN) via cone-beam computed tomography (CBCT).
Materials and Methods
CBCT images of 71 patients (36 males and 35 females) were evaluated. We used the classification described by Solar for IAN evaluation. In this classification, three different types of IAN loops were introduced prior to emerging from the mental foramen. We classified patients according to this system and introduced a new, fourth type.
Results
Type I was seen in 15 sites (10.6%), type II in 39 sites (27.5%), and type III in 50 sites (35.2%). We found a new type in 38 sites (26.8%) that constituted a fourth type.
Conclusion
We found that type III was the most common variant. In the fourth type, the IAN was not detectable because the main nerve was adjacent to the cortical plate and the incisive branch was thinner than the main branch and alongside it. In this type, more care is needed for surgeries including inferior alveolar and mental nerve transposition.
Keywords: Anterior, Mental loop, Cone-beam computed tomography, Iran
I. Introduction
In surgical procedures, attention to anatomical structures and their precise position is paramount1. The inferior alveolar nerve (IAN) canal is an important anatomical landmark in the mandible and contains the clinically important neurovascular bundle2,3,4,5. The mental foramen is superior to the mandibular canal and is apical to the premolars. The IAN divides into two branches before exiting the foramen. One branch exits into soft tissue via the mental foramen and is then named the mental nerve and provides lip and chin sensation. Another branch called the incisive branch goes forward in the bone to supply anterior teeth sensation6,7. In many cases, there is no distinct incisive canal because the nerves are organized in a network and are not detectable on radiographs8.
The mental foramen in the embryonic period is at the apical area of the canine and first deciduous molar6. During the development of the mandible until the eruption of deciduous molars, the mental foramen is displaced anteriorly but after eruption of the second deciduous molar it redirects posteriorly. This displacement is a possible cause for development of an anterior loop of the IAN before it emerges as the mental nerve6,7. The anterior loop of the IAN is an important anatomical variation that originates from the IAN. In its first portion, it dips downwards and is then displaced upward and posteriorly to exit the mental foramen9. Failure to note this mesial loop may cause complications like sensory disorders in the lower lip. Therefore, precise evaluation of its position before surgery is essential. Pre-surgical evaluation of three-dimensional (3D) cone-beam computed tomography (CBCT) images plays an important role in prevention of probable damage. Several cadaver studies using radiological images have classified different shapes of the anterior loops of the IAN. We used the classification described by Solar et al.10. In this classification, three different types have been introduced for the anterior loop. According to this classification, the anterior loop is not seen in type I. The anatomy is Y-shaped and incisive branch thickness is similar to the main branch. In type II, the anterior loop is absent but the anatomy is T-shaped. The incisive branch is perpendicular to the main branch and the mental branch enters the mental foramen in a perpendicular direction. In type III, the anterior loop is detectable and the anatomy is Y-shaped. The incisive branch is thicker than the main branch and the mental branch diverges from the IAN anterior to the mental foramen. The aim of this study was to evaluate different IAN loop anatomical variants in an Iranian population via CBCT.
II. Materials and Methods
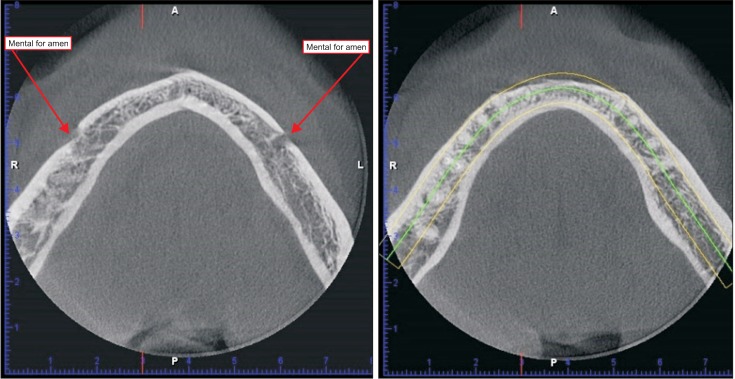
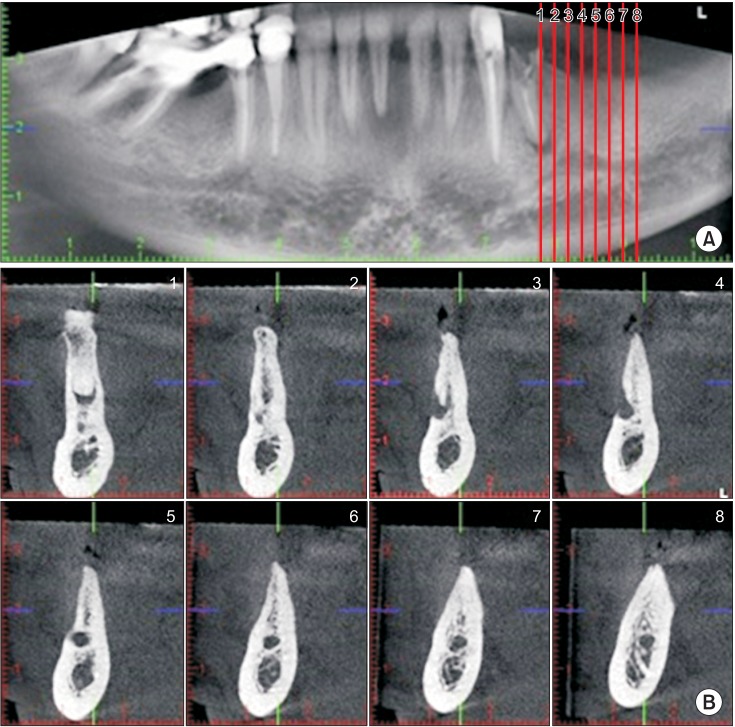
CBCT images of 71 patients (36 males and 35 females) from the radiology department archive of Mashhad Dental School were evaluated. The mean age of the patients was 43.54±9.72 years (range, 20–68 years). All images were taken by the same radiographic device (Planmeca Oy, Helsinki, Finland) and under the same exposure settings of 90 kVp, 10 mA, 12 seconds, and 18×18 cm field of view. All patients with history of trauma to the mandible, developmental anomalies, and pathological lesions were excluded. To ensure precise evaluation, all images were assessed by three postgraduate students who were trained to evaluate the IAN loop and its different types. All data were checked by an associate professor of oral and maxillofacial radiology. Both sides of all images were scanned with 0.2 mm3 voxel size and 2 mm interslice distances. Axial, sagittal, and coronal sections were obtained. All images were similarly evaluated to standardize the procedure. First, the axial section was generated in a way that both left and right mental foramina could be seen. Panoramic curves were then drawn from the right to the left mental foramen.(Fig. 1) Panoramic sections were used to generate the cross-sections.(Fig. 2, 3)
Fig. 1. Both left and right mental foramina on the axial section and panoramic curve drawn on the axial section.
Fig. 2. A. Panoramic section showing type I on both sides; the guide plans for cross sections are also seen. B. Cross-sectional images showing type I.
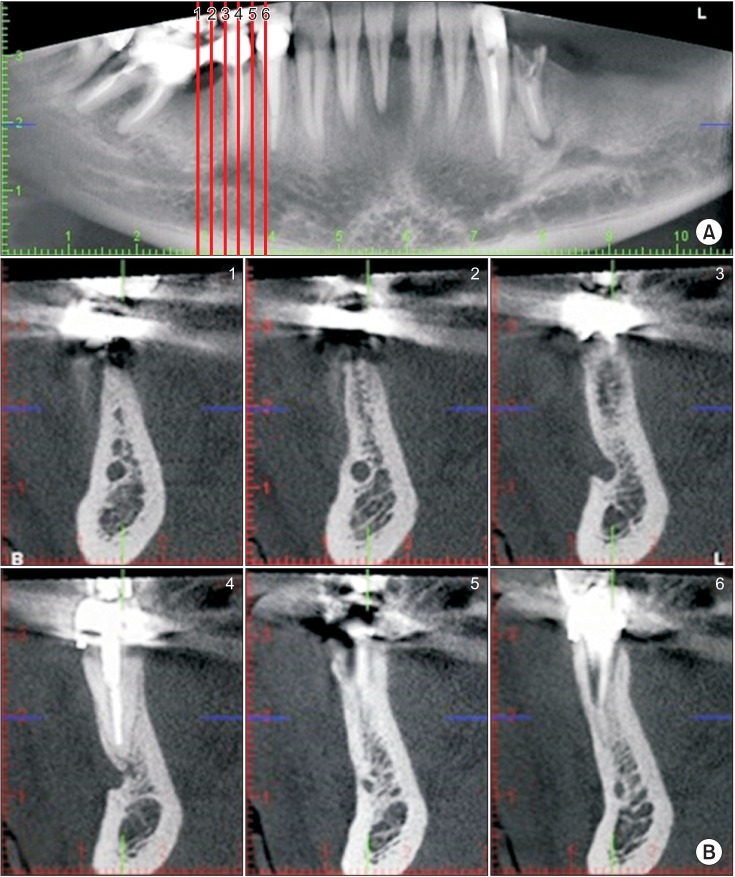
Fig. 3. A. Panoramic view of type IV. B. Cross-sectional images of type IV.
III. Results
In our study, CBCT images of the mandible obtained from 71 patients, 36 male patients (50.7%) and 35 female patients (49.3%), were evaluated bilaterally. Type I was seen at 15 sites (10.6%), type II at 39 sites (27.5%), and type III at 50 sites (35.2%). We identified a new type of the anterior loop at 38 sites (26.8%) that could not be classified into any of the defined types. We found that in some radiographs the shape of the mental nerve was different from type III. In this new type, the inferior alveolar canal is adjacent to the buccal cortical plate of the mandible. The IAN divided into two branches but the mental nerve was not detectable because the main branch was adjacent to the cortical plate in the mental foramen area. The anatomy of this type was neither Y nor T-shaped and the incisive branch was along the main branch and this branch was thinner than the main branch. Panoramic and cross-sectional images of type IV are shown in Fig. 3.
IV. Discussion
Many studies have shown the unreliability of plain radiographs for detection of anatomical structures11. Panoramic radiography is an appropriate imaging modality for observation of the mandibular canal. Vazquez et al.12 evaluated the efficiency of panoramic radiographs for treatment planning of implant surgery. These images effectively evaluated the bone height available for posterior mandibular implants and 3D imaging was not necessary12. However, panoramic radiography is not an efficient imaging modality for evaluation of nerve loop morphology because processing errors and incorrect patient position strongly affect image quality. In addition, the anterior loop is an intermedullary structure that is covered with thick cortical bone13. The absence of the anterior loop in panoramic radiographs does not mean that it does not exist in those cases14,15. 3D imaging is necessary for evaluation of the anterior IAN loop16,17. CBCT is an imaging method that has advantages including easy technique, precise images, decreased artifacts, lower costs, and decreased patient radiation dose compared to computed tomography (CT)18. However, decreased resolution and contrast in comparison to CT are disadvantages. The American Academy of Oral and Maxillofacial Radiology (AAOMR) suggested CBCT for evaluation of periodontal and orthodontic treatment and implant surgeries14,19,20,21,22. According to the results of our study, type I was seen in 10.6%, type II in 27.5%, and type III in 35.2% of patients. Most patients had anterior loops. The results of our study were similar to a study on a Turkish patient population23. They showed that type III was the most prevalent type (59.5%), and type I (8.6%) was the least prevalent type. Several studies (anatomical, radiographic, and combination of both) have evaluated the prevalence of an anterior loop and its morphological characteristics. The findings of these studies are summarized in Table 12,8,9,11,23,24,25,26.
Table 1. Results of anatomical and radiographic studies on the prevalence of the anterior mental loop and its morphological characteristics.
| Author | Year | Country | Evaluation tools | Sample size (n) | Prevalence of anterior mental loop |
|---|---|---|---|---|---|
| Rosenquist24 | 1996 | Cadaver | 58 | 15% | |
| Arzouman et al.9 | 1993 | Cadaver (anatomic and radiographic evaluation) | 25 | Anatomic (96%), radiographic (12%) | |
| Jacobs et al.2 | 2002 | Belgium | Panoramic | 545 | 11% |
| Kaya et al.25 | 2008 | Turkey | Panoramic, CBCT | 73 | Anatomic (28%), CBCT (34%) |
| Ngeow et al.8 | 2009 | Malaya | Panoramic | 33 | 40.2% |
| Benninger et al.26 | 2011 | USA | Cadaver | 15 | 26% |
| Kajan and Salari11 | 2012 | Iran | CBCT | 84 | 36.9% |
| Demir et al.23 | 2015 | Turkey | CBCT | 279 | 59.5% |
| Our study | Iran | CBCT | 91 | 48% |
(CBCT: cone-beam computed tomography)
In our study, this anatomical structure was visible in 50 sites (35.2%). But the prevalence of the anterior loop cannot provide enough information for surgeons because determination of the safety margin for interforaminal surgeries is a major issue. Despite many studies, a distinct distance from the mesial aspect of the mental foramen is still not recommended as a guideline. Different studies suggested a safety margin of 1-9 mm from the anterior margin of the mental foramen10,24,27,28,29,30,31,32,33,34. In a study by Wismeijer et al.13, a protocol with a 3 mm safety margin was considered for all patients, and sensory disorders due to damage to the anterior loop was seen in 7% of cases. A standard distance from the mental foramen as a safe margin still cannot be recommended. Due to fear from this complication, many clinicians place implants anterior to their ideal position to avert damage to the mental nerve and sensory disorders in the lower lip35. In our study, we found a new variant of the anterior loop in 26.8% of sites that could not be classified into any defined type. In this new variation, the nerve was not detectable because the main branch was adjacent to the cortical plate and the incisive branch was along the main branch and this branch was thinner than the main branch. The presence of this type is very important in nerve transpositioning. Superficial IAN positioning in this variant can more likely render damage to the nerve.
In our study, all radiographs available in the archive that matched inclusion criteria were evaluated. Future multicenter studies with a larger sample size can provide more accurate information regarding the prevalence of different mental nerve variants.
V. Conclusion
We found type III to be the most common variant. In the fourth type, the IAN was not detectable because the main nerve was adjacent to the cortical plate and the incisive branch was thinner than the main branch and alongside it. For this type, more care is needed in surgeries including inferior alveolar and mental nerve transposition.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Mraiwa N, Jacobs R, van Steenberghe D, Quirynen M. Clinical assessment and surgical implications of anatomic challenges in the anterior mandible. Clin Implant Dent Relat Res. 2003;5:219–225. doi: 10.1111/j.1708-8208.2003.tb00204.x. [DOI] [PubMed] [Google Scholar]
- 2.Jacobs R, Mraiwa N, vanSteenberghe D, Gijbels F, Quirynen M. Appearance, location, course, and morphology of the mandibular incisive canal: an assessment on spiral CT scan. Dentomaxillofac Radiol. 2002;31:322–327. doi: 10.1038/sj.dmfr.4600719. [DOI] [PubMed] [Google Scholar]
- 3.Agbaje JO, Sun Y, De Munter S, Schepers S, Vrielinck L, Lambrichts I, et al. CBCT-based predictability of attachment of the neurovascular bundle to the proximal segment of the mandible during sagittal split osteotomy. Int J Oral Maxillofac Surg. 2013;42:308–315. doi: 10.1016/j.ijom.2012.07.012. [DOI] [PubMed] [Google Scholar]
- 4.Alqerban A, Jacobs R, Souza PC, Willems G. In-vitro comparison of 2 cone-beam computed tomography systems and panoramic imaging for detecting simulated canine impaction-induced external root resorption in maxillary lateral incisors. Am J Orthod Dentofacial Orthop. 2009;136:764, 764.e1–764.e11. doi: 10.1016/j.ajodo.2009.03.036. discussion 764-5. [DOI] [PubMed] [Google Scholar]
- 5.White SC. Cone-beam imaging in dentistry. Health Phys. 2008;95:628–637. doi: 10.1097/01.HP.0000326340.81581.1a. [DOI] [PubMed] [Google Scholar]
- 6.Chávez-Lomeli ME, Mansilla Lory J, Pompa JA, Kjaer I. The human mandibular canal arises from three separate canals innervating different tooth groups. J Dent Res. 1996;75:1540–1544. doi: 10.1177/00220345960750080401. [DOI] [PubMed] [Google Scholar]
- 7.de Villiers H. The skull of the South African Negro: a biometrical and morphological study. Johannesburg: Wits University Press; 1970. [Google Scholar]
- 8.Ngeow WC, Dionysius DD, Ishak H, Nambiar P. A radiographic study on the visualization of the anterior loop in dentate subjects of different age groups. J Oral Sci. 2009;51:231–237. doi: 10.2334/josnusd.51.231. [DOI] [PubMed] [Google Scholar]
- 9.Arzouman MJ, Otis L, Kipnis V, Levine D. Observations of the anterior loop of the inferior alveolar canal. Int J Oral Maxillofac Implants. 1993;8:295–300. [PubMed] [Google Scholar]
- 10.Solar P, Ulm C, Frey G, Matejka M. A classification of the intraosseous paths of the mental nerve. Int J Oral Maxillofac Implants. 1994;9:339–344. [Google Scholar]
- 11.Kajan ZD, Salari A. Presence and course of the mandibular incisive canal and presence of the anterior loop in cone beam computed tomography images of an Iranian population. Oral Radiol. 2012;28:55–61. [Google Scholar]
- 12.Vazquez L, Saulacic N, Belser U, Bernard JP. Efficacy of panoramic radiographs in the preoperative planning of posterior mandibular implants: a prospective clinical study of 1527 consecutively treated patients. Clin Oral Implants Res. 2008;19:81–85. doi: 10.1111/j.1600-0501.2007.01402.x. [DOI] [PubMed] [Google Scholar]
- 13.Wismeijer D, van Waas MA, Vermeeren JI, Kalk W. Patients' perception of sensory disturbances of the mental nerve before and after implant surgery: a prospective study of 110 patients. Br J Oral Maxillofac Surg. 1997;35:254–259. doi: 10.1016/s0266-4356(97)90043-7. [DOI] [PubMed] [Google Scholar]
- 14.Kalender A, Orhan K, Aksoy U. Evaluation of the mental foramen and accessory mental foramen in Turkish patients using cone-beam computed tomography images reconstructed from a volumetric rendering program. Clin Anat. 2012;25:584–592. doi: 10.1002/ca.21277. [DOI] [PubMed] [Google Scholar]
- 15.Kuzmanovic DV, Payne AG, Kieser JA, Dias GJ. Anterior loop of the mental nerve: a morphological and radiographic study. Clin Oral Implants Res. 2003;14:464–471. doi: 10.1034/j.1600-0501.2003.00869.x. [DOI] [PubMed] [Google Scholar]
- 16.Chen JC, Lin LM, Geist JR, Chen JY, Chen CH, Chen YK. A retrospective comparison of the location and diameter of the inferior alveolar canal at the mental foramen and length of the anterior loop between American and Taiwanese cohorts using CBCT. Surg Radiol Anat. 2013;35:11–18. doi: 10.1007/s00276-012-0986-z. [DOI] [PubMed] [Google Scholar]
- 17.Parnia F, Moslehifard E, Hafezeqoran A, Mahboub F, Mojaver-Kahnamoui H. Characteristics of anatomical landmarks in the mandibular interforaminal region: a cone-beam computed tomography study. Med Oral Patol Oral Cir Bucal. 2012;17:e420–e425. doi: 10.4317/medoral.17520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Danforth RA, Dus I, Mah J. 3-D volume imaging for dentistry: a new dimension. J Calif Dent Assoc. 2003;31:817–823. [PubMed] [Google Scholar]
- 19.Haghanifar S, Rokouei M. Radiographic evaluation of the mental foramen in a selected Iranian population. Indian J Dent Res. 2009;20:150–152. doi: 10.4103/0970-9290.52886. [DOI] [PubMed] [Google Scholar]
- 20.Bushong SC. Radiologic science for technologists: physics, biology, and protection. 8th ed. New York: Elsevier; 2004. pp. 29–30. [Google Scholar]
- 21.Katakami K, Mishima A, Shiozaki K, Shimoda S, Hamada Y, Kobayashi K. Characteristics of accessory mental foramina observed on limited cone-beam computed tomography images. J Endod. 2008;34:1441–1445. doi: 10.1016/j.joen.2008.08.033. [DOI] [PubMed] [Google Scholar]
- 22.Koh KJ, Kim KA. Observation of the anterior loop and mental foramen of the mandibular canal using cone beam computed tomography. Korean J Oral Maxillofac Radiol. 2009;39:81–87. [Google Scholar]
- 23.Demir A, Izgi E, Pekiner FN. Anterior loop of the mental foramen in a Turkish subpopulation with dentate patients: a cone beam computed tomography study. J Marmara Univ Inst Health Sci. 2015;5:231–238. [Google Scholar]
- 24.Rosenquist B. Is there an anterior loop of the inferior alveolar nerve? Int J Periodontics Restorative Dent. 1996;16:40–45. [PubMed] [Google Scholar]
- 25.Kaya Y, Sencimen M, Sahin S, Okcu KM, Dogan N, Bahcecitapar M. Retrospective radiographic evaluation of the anterior loop of the mental nerve: comparison between panoramic radiography and spiral computerized tomography. Int J Oral Maxillofac Implants. 2008;23:919–925. [PubMed] [Google Scholar]
- 26.Benninger B, Miller D, Maharathi A, Carter W. Dental implant placement investigation: is the anterior loop of the mental nerve clinically relevant? J Oral Maxillofac Surg. 2011;69:182–185. doi: 10.1016/j.joms.2010.07.060. [DOI] [PubMed] [Google Scholar]
- 27.Mraiwa N, Jacobs R, Moerman P, Lambrichts I, van Steenberghe D, Quirynen M. Presence and course of the incisive canal in the human mandibular interforaminal region: two-dimensional imaging versus anatomical observations. Surg Radiol Anat. 2003;25:416–423. doi: 10.1007/s00276-003-0152-8. [DOI] [PubMed] [Google Scholar]
- 28.Bavitz JB, Harn SD, Hansen CA, Lang M. An anatomical study of mental neurovascular bundle-implant relationships. Int J Oral Maxillofac Implants. 1993;8:563–567. [PubMed] [Google Scholar]
- 29.Mardinger O, Chaushu G, Arensburg B, Taicher S, Kaffe I. Anterior loop of the mental canal: an anatomical-radiologic study. Implant Dent. 2000;9:120–125. doi: 10.1097/00008505-200009020-00003. [DOI] [PubMed] [Google Scholar]
- 30.Yu SK, Kim S, Kang SG, Kim JH, Lim KO, Hwang SI, et al. Morphological assessment of the anterior loop of the mandibular canal in Koreans. Anat Cell Biol. 2015;48:75–80. doi: 10.5115/acb.2015.48.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Uchida Y, Noguchi N, Goto M, Yamashita Y, Hanihara T, Takamori H, et al. Measurement of anterior loop length for the mandibular canal and diameter of the mandibular incisive canal to avoid nerve damage when installing endosseous implants in the interforaminal region: a second attempt introducing cone beam computed tomography. J Oral Maxillofac Surg. 2009;67:744–750. doi: 10.1016/j.joms.2008.05.352. [DOI] [PubMed] [Google Scholar]
- 32.Oguz O, Bozkir MG. Evaluation of location of mandibular and mental foramina in dry, young, adult human male, dentulous mandibles. West Indian Med J. 2002;51:14–16. [PubMed] [Google Scholar]
- 33.Rosa MB, Sotto-Maior BS, Machado Vde C, Francischone CE. Retrospective study of the anterior loop of the inferior alveolar nerve and the incisive canal using cone beam computed tomography. Int J Oral Maxillofac Implants. 2013;28:388–392. doi: 10.11607/jomi.2648. [DOI] [PubMed] [Google Scholar]
- 34.Apostolakis D, Brown JE. The dimensions of the mandibular incisive canal and its spatial relationship to various anatomical landmarks of the mandible: a study using cone beam computed tomography. Int J Oral Maxillofac Implants. 2013;28:117–124. doi: 10.11607/jomi.2372. [DOI] [PubMed] [Google Scholar]
- 35.Lee JK, Kim YG. An anatomical study on the mandibular medial surface by CBCT analysis for safer implant placement. J Korean Assoc Oral Maxillofac Surg. 2011;37:43–48. [Google Scholar]