Abstract
Background: Prior research indicates that hospice and palliative care delivered in outpatient settings are associated with reduced hospital readmissions for cancer patients. However, little is known about how inpatient palliative care affects readmissions in oncology.
Objective: To examine associations among inpatient palliative care consultation, hospice use (discharge), and 30-day readmissions among patients with solid tumor cancers.
Methods: We identified all live discharges from a large tertiary cancer hospital between 2010 and 2016. Palliative care consult data were abstracted from medical charts and linked to hospital encounter data. Propensity scores were used to match palliative care consult to usual care encounters. Modified Poisson regression models estimated adjusted relative risk (aRR) and 95% confidence intervals (CI) of 30-day readmissions and hospice discharge. We compared predicted probabilities of readmission for palliative care consultation with hospice discharge, without hospice discharge, and usual care.
Results: Of 8085 eligible encounters, 753 involved a palliative care consult. The likelihood of having a 30-day readmission did not differ between palliative care consult and usual care groups (p > 0.05). However, the palliative care consult group was more likely than usual care to have a hospice discharge (aRR = 4.09, 95% CI: 3.07–5.44). The predicted probability of 30-day readmission was lower when palliative care consultation was combined with hospice discharge compared to usual care or consultation with discharge to nonhospice postacute care (p < 0.001).
Conclusions: The effect of inpatient palliative care on readmissions in oncology is largely driven by hospice enrollment. Strategies that combine palliative care consultation with hospice discharge may decrease hospital readmissions and improve cancer care quality.
Keywords: : inpatient palliative care, oncology, 30-day readmissions, hospice
Introduction
Many cancer patients experience poor symptom control and aggressive treatment near the end of their lives, including hospitalizations and emergency department (ED) visits, with limited medical benefits.1–4 Unplanned 30-day hospital readmission rates as high as 27% have been reported in patients with cancer.5 Reducing unplanned 30-day readmissions is important to patients and healthcare organizations seeking to lower overall healthcare costs and avoid financial penalties under the federal Hospital Readmissions Reduction Program.6 Although cancer hospitals currently are excluded from this penalty, frequent hospital readmissions and ED visits remain important for oncology patients and are well-accepted indicators of poor quality care for cancer patients near the end of life.1,7
Prior research indicates hospice use is associated with reduced hospital readmissions among cancer patients,3,5 yet conversations about hospice often do not occur between cancer patients and their providers.8 As a result, cancer patients frequently do not enroll in hospice or are referred late in the disease trajectory.9 Palliative care has also been shown to decrease hospitalizations and ED visits among cancer patients when delivered in outpatient settings.10–13 In inpatient settings, palliative care reduces the intensity of hospital treatment, and thus reduces the cost of hospital care.14,15 However, less is known about how inpatient palliative care affects readmissions in oncology.
Therefore, using a propensity-matched cohort from a large tertiary cancer hospital, we examined associations among inpatient palliative care consultation, hospice use (discharge), and 30-day unplanned readmissions. We hypothesized that inpatient palliative care consultation would be associated with greater hospice discharge and reduced 30-day readmissions. To further understand the mechanism by which inpatient palliative care may reduce readmissions, we also explored whether inpatient palliative care consultation combined with hospice discharge was associated with reduced 30-day readmissions.
Methods
Sample
We conducted a retrospective cohort study of all patients who were admitted and/or discharged from the medical oncology or gynecologic oncology service lines at University of North Carolina (UNC) Hospitals (an 804-bed acute care facility and National Cancer Institute-designated Comprehensive Cancer Center) from January 1, 2010, to June 30, 2016. We included all live discharges with a solid tumor diagnosis documented during the hospital stay based on International Classification of Diseases (ICD) 9 and 10 codes (Supplementary Table S1; Supplementary Data are available online at www.liebertpub.com/jpm). If multiple palliative care consults occurred during an encounter, we only included the first one. We excluded 69 palliative care consults that were initiated in a service other than the admitting and/or discharge service (e.g., originated in medical intensive care, but the admitting and/or discharge service was medical oncology).
The unit of analysis was the discharge encounter for hospitalization. All eligible encounters included in the sample were considered to be an index admission. Encounters with a discharge status of missing, “left against medical advice,” or deceased were excluded as an index admission, but could be considered a readmission. A readmission could also serve as an index admission for subsequent discharge encounters.
UNC Hospital inpatient palliative care consultation service
The inpatient palliative care consult service at UNC Hospitals began in 2002. The team is interdisciplinary, composed of an attending palliative physician, two nurse practitioners, a social worker, and a chaplain. Palliative care clinicians provide expert pain and symptom management, supportive services for spiritual/psychosocial distress, goal setting, and decision making for inpatients at all stages of illness and their families. Consultation is available to patients by referral of the inpatient treating physician. The inpatient palliative care consult service at UNC Hospitals is a part of the UNC Health Care System, which includes a hospice program. In addition, several geographically proximate hospices have internal liaisons who visit UNC Hospitals. However, patients are referred to UNC Hospitals statewide; thus, the palliative care team makes referrals to hospices beyond those represented on-site.
Data sources
We obtained data on palliative care consults from the UNC Palliative Care Clinical Research database, which includes data abstracted from medical charts for all patients at UNC Hospital referred for palliative care consultation. This data source provided dates of service and referring oncology service. Using unique identifiers, we linked these data to hospital encounter data obtained from the Carolina Data Warehouse for Health (a central data repository containing clinical, research, and administrative data sourced from the institution electronic health record system). This data source provided admitting and discharge service and dates, discharge status, as well as clinical and demographic characteristics. The dataset was then augmented with information on patient cancer stage at diagnosis as a proximate indicator of disease extent during hospitalization obtained from the UNC Hospital Cancer Registry. The UNC Institutional Review Board reviewed and approved this study.
Measures
Outcomes
Our primary outcomes were hospice discharge (inpatient or home) and 30-day unplanned all-cause readmissions. We defined readmission as an inpatient episode, including ED visits resulting in an admission, within 30 days of discharge. Secondary outcomes included ED visits not resulting in an admission within 30 days of discharge and a composite outcome of inpatient readmissions and ED visits within 30 days of discharge. We calculated time to readmission as the number of days between the index admission discharge date and readmission date.
Longer travel distance is an obstacle for accessing hospital care.16 As such, because our data sources were unique to only one hospital system, readmissions for patients whose residence was further away might be missed. To minimize potential measurement error, we used Hospital Referral Region (HRR) as a proxy for travel distance and restricted the sample to encounters with resident zip codes in the Durham, Raleigh and Greensboro North Carolina HRRs. Admissions for chemotherapy or radiotherapy (identified using ICD codes V58.xx and Z51.xx), psychiatry, or rehabilitation services were not considered readmissions since these usually indicated a planned admission.
Independent variable
The independent variable was whether or not an encounter involved a palliative care consultation. Encounters that involved a palliative care consult were included in the “treatment” group; encounters that did not involve palliative care consult were included in the “usual care” group.
Covariate selection
We used propensity score matching (see below) to balance treatment and usual care groups on the following clinical and demographic covariates: race (white, black, other, and missing); sex; insurance status (private, Medicare, Medicaid, other public, uninsured, and missing); palliative care consultation in a prior hospital encounter; hospitalization in the prior 30 days; solid tumor cancer type (digestive, breast, bone/joint, soft tissue, skin, head/neck, urological, lung/thoracic, gynecological, other/ill defined, central nervous system, and missing); oncology service (medical oncology or gynecologic oncology); and admission year. Age was included as a continuous variable. Stage of disease at diagnosis was based on the American Joint Committee on Cancer staging criteria (0 or 1, 2 or 3, 4). If stage could not be ascertained, it was categorized as “missing.” We assessed comorbidity illness (0, 1, 2, or more comorbidities) using previously described coding algorithms.17 Comorbidity ICD codes were derived from the patient's problem list in the electronic health record system. The comorbidities in the electronic health record may be added any time patients receive care at the institution and are not associated with a specific encounter. We searched the problem list for evidence of comorbidities 30 days before and after the admission date to ensure all comorbidities present at the time of an encounter were captured.
Propensity score
To minimize the potential for selection bias, propensity scores were used to identify encounters that did not involve a palliative care consult, but were comparable to encounters that did involve a palliative care consult based on the aforementioned observed covariates.18 We used a modified Poisson regression model19 with palliative care consult as the outcome and observed covariates as predictors to calculate propensity scores. Length of stay (number of calendar days between admission date to discharge date) was included as an exposure variable in the model to account for different observation periods. Robust standard errors clustered at the patient level were used to account for autocorrelation across encounters, since some patients may have had multiple hospitalizations. Encounters that involved a palliative care consult were matched 1:1 to usual care encounters using the nearest neighbor with replacement method, which provided the smallest absolute standardized difference in covariates between the groups (i.e., <10%). Covariates with a standardized difference greater than 10% were additionally adjusted for in the postmatch analysis.
Statistical analysis
Using the propensity score matched sample, we estimated the adjusted relative risk (aRR) and 95% confidence intervals (CI) of hospice discharge, 30-day unplanned all-cause readmission, and secondary outcomes (i.e., ED visits and a composite outcome of inpatient readmissions and ED visits) using modified Poisson regression models. For the readmission analysis, we included days to death after discharge (number of calendar days between discharge date to death date) as the exposure to account for mortality during the 30-day readmission window. We used robust standard errors clustered at the patient level. We included hospice discharge as a covariate in the model when examining whether the combination of palliative care consultation with hospice discharge was associated with lower 30-day readmissions. Adjusted predicted probabilities of a 30-day readmission for an encounter were then calculated to contrast outcomes for the following clinical scenarios: usual care, palliative consultation combined with hospice discharge, and palliative care consultation with discharge to nonhospice postacute care (e.g., home with self-care or intermediate care facility). We conducted our analyses using Stata version 13.0 (College Station, TX). All statistical tests were two tailed with a critical alpha equal to 0.05.
Results
Sample
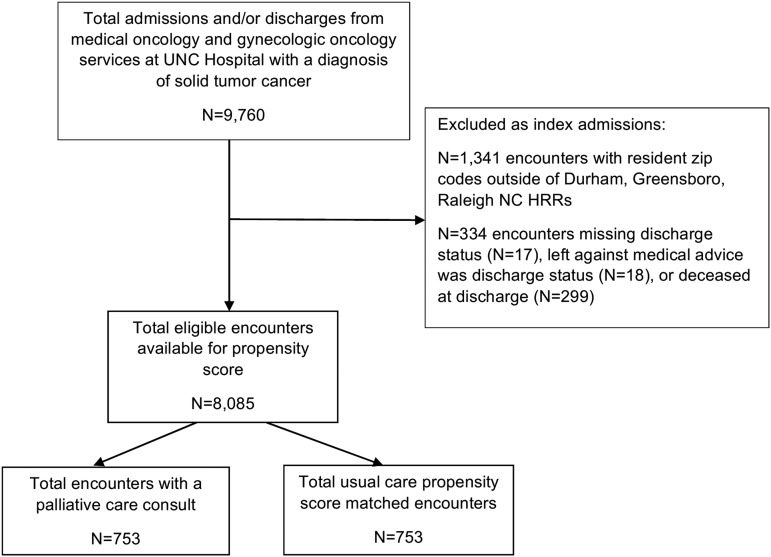
There were 9760 discharge encounters from the medical oncology or gynecological oncology inpatient services. Of these, 1341 had resident zip codes outside of the Durham, Raleigh, and Greensboro HRRs and 334 had a discharge status of missing, “left against medical advice,” or deceased. Of the 8085 eligible discharge encounters, 753 involved a palliative care consult (Fig. 1); 753 usual care propensity scored matched encounters were found (n = 1506), representing 1081 distinct patients across the treatment and usual care groups. On average, patients had 2.4 discharges from the oncology inpatient services during the study period.
FIG. 1.
Study sample flow diagram.
The demographic and clinical characteristics of the unmatched and matched samples are presented in Table 1. The sample was predominantly white, male, and insured by Medicare. The mean age was around 60. Most encounters originated from the medical oncology service. The unmatched sample indicated that compared to usual care, the palliative care consult group was more likely to be male, have a diagnosis of certain cancer types, have a palliative care consult in a prior hospital encounter, and be hospitalized in the prior 30 days. After matching, characteristics between the palliative care consult and usual care groups were similar (absolute standardized difference of <10%). However, the palliative care consult group remained significantly more likely than usual care to have a palliative care consult in a prior hospital encounter (15.6% vs. 9.8%) and hospitalization in the prior 30 days (30.2% vs. 24.2%). Therefore, we adjusted for these covariates in the postmatch analysis.
Table 1.
Description of Sample by Palliative Care Consult Status, Matched (N = 1506) and Unmatched (N = 8085)
| Unmatched | Matched | ||||
|---|---|---|---|---|---|
| Variables | Palliative care consulted (n = 753) | Usual care (n = 7332) | Absolute standardized difference (%) | Usual care (n = 753) | Absolute standardized difference (%) |
| Age, mean (SD) | 58.6 | 58.5 | 0.4 | 59.3 | 5.6 |
| Race (%) | |||||
| White | 60.3 | 62.2 | 3.9 | 58.2 | 4.3 |
| Black | 29.6 | 28.8 | 1.7 | 29.9 | 0.6 |
| Other | 8.0 | 7.5 | 1.7 | 9.3 | 5.0 |
| Missing | 2.1 | 1.5 | 4.5 | 2.6 | 4.0 |
| Sex: female (%) | 24.2 | 31.9 | 17.2 | 27.5 | 7.4 |
| Insurance (%) | |||||
| Medicare | 41.7 | 40.6 | 2.2 | 44.5 | 5.6 |
| Medicaid | 18.3 | 19.1 | 2.1 | 16.7 | 4.1 |
| Other public | 3.7 | 2.9 | 4.7 | 3.3 | 2.2 |
| Uninsured | 1.8 | 2.6 | 5.1 | 1.8 | 0.0 |
| Private | 30.3 | 31.0 | 1.7 | 29.3 | 2.0 |
| Missing | 4.1 | 3.8 | 1.7 | 4.4 | 1.4 |
| Cancer type (%) | |||||
| Digestive: yes | 46.5 | 32.4 | 29.0 | 47.9 | 3.0 |
| Breast: yes | 6.4 | 7.9 | 6.1 | 7.2 | 3.1 |
| Bone/joint: yes | 23.6 | 16.3 | 18.5 | 23.2 | 1.0 |
| Soft tissue: yes | 2.5 | 2.8 | 1.9 | 2.0 | 3.3 |
| Skin: yes | 5.6 | 2.5 | 15.6 | 4.5 | 5.4 |
| Head/neck: yes | 1.5 | 3.5 | 13.2 | 1.6 | 0.9 |
| Urological: yes | 5.8 | 5.4 | 2.1 | 5.7 | 0.6 |
| Lung/thoracic: yes | 31.3 | 25.7 | 12.4 | 28.9 | 5.3 |
| Gynecological: yes | 30.0 | 27.3 | 5.9 | 26.2 | 8.5 |
| Other/ill defined: yes | 23.7 | 15.4 | 21.2 | 22.8 | 2.4 |
| CNS: yes | 12.6 | 10.8 | 5.6 | 12.3 | 0.8 |
| Missing: yes | 5.4 | 8.8 | 13.0 | 4.0 | 5.7 |
| Cancer stage (%) | |||||
| 0 or 1 | 8.6 | 11.3 | 9.0 | 9.4 | 2.8 |
| 2 or 3 | 33.5 | 29.1 | 9.8 | 35.4 | 4.0 |
| 4 | 23.6 | 24.3 | 1.6 | 23.1 | 1.2 |
| Missing | 34.1 | 35.3 | 2.4 | 32.1 | 4.2 |
| Comorbidities: Charlson Index (%) | |||||
| 0 | 70.9 | 72.9 | 3.6 | 66.0 | 9.7 |
| 1 | 18.1 | 16.7 | 4.0 | 20.5 | 6.3 |
| ≥2 | 10.8 | 10.4 | 1.5 | 13.5 | 8.6 |
| Length of stay, mean days (SD) | 9.6 (8.9) | — | — | 10.5 (9.2) | |
| Days to death postdischarge, mean days (SD)a | 13.9 (8.5) | — | — | 14.0 (8.2) | — |
| PC consulted during a prior hospitalization: yes (%)b | 15.6 | 3.9 | 40.2 | 9.8 | 20.0 |
| Hospitalized in prior 30 days: yes (%)b | 30.2 | 22.5 | 17.6 | 24.2 | 13.9 |
| Service (%) | |||||
| Medical oncology | 53.5 | 60.8 | 14.8 | 56.6 | 6.2 |
| Gynecologic oncology | 46.4 | 39.2 | 14.8 | 43.4 | 6.2 |
| Year of encounter (%) | |||||
| 2010 | 10.8 | 16.3 | 16.1 | 10.6 | 0.6 |
| 2011 | 15.5 | 18.3 | 7.4 | 15.0 | 1.4 |
| 2012 | 13.6 | 15.9 | 6.5 | 14.6 | 2.6 |
| 2013 | 12.8 | 16.2 | 9.4 | 13.5 | 1.9 |
| 2014 | 15.4 | 13.4 | 5.7 | 16.1 | 1.9 |
| 2015 | 17.1 | 12.5 | 13.0 | 16.1 | 3.0 |
| 2016 | 14.6 | 7.4 | 23.3 | 14.1 | 1.7 |
Calculated for 349 encounters in the matched sample where a death date was recorded within 30 days of discharge date.
Covariates with standardized difference >10% were adjusted for in the postmatch analysis.
CNS, central nervous system, PC, palliative care; SD, standard deviation.
Associations among inpatient palliative care consultation, hospice discharge, and 30-day readmissions
Table 2 shows rates of hospice discharge and 30-day readmissions using the matched sample. Overall, inpatient readmission rates were high, with 21% and 25.5% of encounters resulting in a readmission within 30 days of discharge in the palliative care consult and usual care groups, respectively. However, the ED visit rates without admission within 30 days of discharge were only 3.9% and 5.7% for the palliative care consult and usual care groups, respectively.
Table 2.
Associations among Palliative Care Consultation, Hospice Discharge, and 30-Day Readmissions in Inpatient Oncology
| Outcome variables | Palliative care consulted (n = 753) | Usual care (n = 753) | Adjusted relative risk (95% CI) |
|---|---|---|---|
| Discharge to hospice, n (%) | 286 (38.0) | 69 (9.2) | 4.09 (3.07–5.44)* |
| Inpatient readmission 30 days after discharge, n (%) | 158 (21.0) | 192 (25.5) | 0.93 (0.76–1.13) |
| ED visit 30 days after discharge, n (%) | 29 (3.9) | 43 (5.7) | 0.76 (0.46–1.24) |
| Inpatient readmission or ED visit 30 days after discharge, n (%) | 187 (24.8) | 235 (31.2) | 0.89 (0.75–1.07) |
Regressions adjusted for palliative care consult in a prior hospital encounter and hospitalization in the prior 30 days.
p < 0.001.
CI, confidence interval; ED, emergency department.
In the adjusted analysis, the likelihood of having an inpatient readmission, ED visit, or composite outcome of an inpatient readmission and ED visit within 30 days of discharge did not significantly differ between the palliative care consult and usual care groups (p > 0.05). However, the palliative care consult group was significantly (p < 0.001) more likely than usual care to have a hospice discharge (38% vs. 9.2%; aRR = 4.09, 95% CI: 3.07–5.44) (Table 2).
The adjusted predicted probability of an inpatient readmission was significantly (p < 0.001) lower when palliative care consultation was combined with hospice discharge (5.8%), compared to usual care (25.3%) or palliative care consultation with discharge to nonhospice postacute care (29.4%). Likewise, the predicted probability of an inpatient readmission or ED visit was significantly (p < 0.001) lower when palliative care consultation was combined with hospice discharge (8.9%), compared to usual care (31%) or palliative care consultation with discharge to nonhospice locations (34%). Across all comparisons, we found no differences (p > 0.05) in the predicted probability of an ED visit (Table 3).
Table 3.
Adjusted Predicted Probabilities and 95% Confidence Intervals of 30-Day Readmission Outcomes in Inpatient Oncology
| Outcome variables | Palliative care consulted (with hospice discharge) (n = 753) | Palliative care consulted (without hospice discharge) (n = 753) | Usual care (with hospice discharge) (n = 753) | Usual care (without hospice discharge) (n = 753) |
|---|---|---|---|---|
| Inpatient readmission 30 days after discharge | 5.8% (0.03–0.09)* | 29.4% (0.25–0.33) | 5.1% (0.02–0.08) | 25.3% (0.22–0.29) |
| ED visit 30 days after discharge | 2.9% (0.01–0.05) | 4.6% (0.03–0.06) | 3.1% (0.00–0.06) | 5.5% (0.04–0.07) |
| Inpatient readmission or ED visit 30 days after discharge | 8.9% (0.05–0.126)* | 34.0% (0.30–0.38) | 8.5% (0.05–0.12) | 31.0% (0.27–0.35) |
Palliative care consultation combined with hospice discharge versus discharge to nonhospice postacute care and usual care. Regression adjusted for hospice discharge, palliative care consult in a prior hospital encounter, and hospitalization in the prior 30 days.
p < 0.001.
Discussion
This study examined associations among inpatient palliative care consultation, hospice use, and 30-day unplanned readmissions among patients with solid tumors admitted to oncology services. After propensity score matching, we found palliative care consult and usual care groups had similar likelihoods of 30-day readmissions, including any return to acute care, defined as inpatient readmission or ED visit. However, consistent with our hypothesis, the palliative care consult group was over four times more likely than usual care to have a hospice discharge. This finding is consistent with prior research indicating earlier and more frequent hospice use among cancer patients when specialty palliative care augments oncology care.20–24 When examined more closely, palliative care consultation combined with hospice discharge had a much lower probability of inpatient readmission or ED visit (combined), compared to usual care or palliative care consultation in the absence of hospice discharge. This was also true for inpatient readmissions. Our findings extend prior research demonstrating that the effect of inpatient palliative care consultation on readmissions is largely driven by hospice enrollment25–27; we provide important insights into the mechanism by which inpatient palliative care consultation may reduce 30-day readmissions in oncology. For example, using a propensity score matched sample, Tangeman et al. found a similar likelihood of 30-day readmissions among inpatient palliative care and usual care patients. However, only 1.1% of inpatient palliative care patients discharged to hospice experienced a readmission compared to 6.6% of usual care patients (p < 0.01).27 Likewise, among patients who received an inpatient palliative care consultation, Enguidanos et al. found that patients discharged home with self-care were 3.7 times more likely to be readmitted within 30 days of discharge compared to patients discharged with hospice or home-based palliative care (p < 0.05).25 Thus, our study adds to evidence supporting outpatient palliative care services, including hospice, as support for patients with serious illness to manage their persistent symptom distress and rapid changes in health. Additional research elucidating the relationship between inpatient palliative care consultation, continuity of care in the outpatient setting, and readmissions in oncology is needed.
The findings also speak to the importance of enhancing collaboration and care coordination between inpatient palliative care and hospice, or other outpatient palliative care specialty services. Cancer patients near the end of life are often faced with the decision to pursue comfort treatment and transition to hospice. Palliative care teams play an active role in patients' decision-making process about hospice enrollment, including dispelling myths that hospice hastens death or is appropriate only in the final days of life.28 As our findings suggest, inpatient palliative care consultations are key to initiating goals of care and advanced care planning discussions to bridge these difficult transitions from hospitalization to hospice for cancer patients. Future efforts are needed to develop effective partnerships between inpatient palliative care and hospice programs to ensure care continuity, such as involving hospice providers in the development and operation of inpatient palliative care services.29
There are several limitations to this study. First, it was conducted at a single academic medical center with an established inpatient palliative care consultation service. As such, this limits generalizability. Second, we only included readmissions to one hospital system, which may underestimate readmissions. We attempted to address this limitation by including resident zip codes and neighboring HRRs as a proxy for travel distance. Of note, we conducted the analysis on the full sample and the findings were similar. Third, although selection bias was minimized through propensity score matching, we cannot rule out the possibility of unobserved confounding. Instrumental variables could potentially address unobserved confounding, but we were unable to identify a valid instrumental variable for this sample. Fourth, we lacked data on the “active ingredients” of palliative care consultations (e.g., goals of care and treatment decision making, symptom management, or other elements important in the choice for hospice). Identifying components of palliative care consultation, and their delivery by specialty palliative care versus oncology providers, is an important area for future research.
Despite these limitations, this study makes an important contribution to understanding the role of inpatient palliative care consultation in mitigating use of low-benefit, high-cost treatments by increasing hospice use and reducing 30-day readmissions in oncology. To date, little is known about how hospitals can best achieve reductions in readmissions in oncology.3,30,31 However, studies focusing on associations between inpatient palliative care consultation and both hospice use and 30-day readmissions in oncology are limited.32 Using a large sample of hospitalizations across multiple cancer types, our study is the first to demonstrate that inpatient palliative care consultation can achieve a significant decrease in 30-day readmissions in oncology, mostly through combining consultation with hospice discharge. Considering prior research, which shows cancer inpatients underuse palliative care services,20,33,34 our findings have important implications for the need to develop strategies that promote palliative care consultation and earlier introduction of hospice in inpatient oncology.
Supplementary Material
Acknowledgment
Dr. DiMartino's work on this research was supported by grant funding from the National Cancer Institute Cancer Control Education Program (R25 CA057726). The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Award Number TL1TR001110. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Earle CC, Landrum MB, Souza JM, et al. : Aggressiveness of cancer care near the end of life: Is it a quality-of-care issue? J Clin Oncol 2008;26:3860–3866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morden NE, Chang CH, Jacobson JO, et al. : End-of-life care for Medicare beneficiaries with cancer is highly intensive overall and varies widely. Health Aff (Millwood) 2012;31:786–796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Manzano JG, Gadiraju S, Hiremath A, et al. : Unplanned 30-day readmissions in a General Internal Medicine Hospitalist Service at a Comprehensive Cancer Center. J Oncol Prac 2015;11:410–415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mayer DK, Travers D, Wyss A, et al. : Why do patients with cancer visit emergency departments? Results of a 2008 population study in North Carolina. J Clin Oncol 2011;29:2683–2688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brooks GA, Abrams TA, Meyerhardt JA, et al. : Identification of potentially avoidable hospitalizations in patients with GI cancer. J Clin Oncol 2014;32:496–503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hansen LO, Young RS, Hinami K, et al. : Interventions to reduce 30-day rehospitalization: A systematic review. Ann Intern Med 2011;155:520–528 [DOI] [PubMed] [Google Scholar]
- 7.National Quality Forum. National Quality Forum: NQF-Endorsed Standards. www.qualityforum.org/measures_list.aspx (last accessed March1, 2017)
- 8.Rocque GB, Cleary JF: Palliative care reduces morbidity and mortality in cancer. Nat Rev Clin Oncol 2013;10:80–89 [DOI] [PubMed] [Google Scholar]
- 9.Shin JA, Parkes A, El-Jawahri A, et al. : Retrospective evaluation of palliative care and hospice utilization in hospitalized patients with metastatic breast cancer. Palliat Med 2016;30:854–861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hui D, Kim SH, Roquemore J, et al. : Impact of timing and setting of palliative care referral on quality of end-of-life care in cancer patients. Cancer 2014;120:1743–1749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McNamara BA, Rosenwax LK, Murray K, et al. : Early admission to community-based palliative care reduces use of emergency departments in the ninety days before death. J Palliat Med 2013;16:774–779 [DOI] [PubMed] [Google Scholar]
- 12.Scibetta C, Kerr K, McGuire J, et al. : The costs of waiting: Implications of the timing of palliative care consultation among a cohort of decedents at a Comprehensive Cancer Center. J Palliat Med 2016;19:69–75 [DOI] [PubMed] [Google Scholar]
- 13.Temel JS, Greer JA, Muzikansky A, et al. : Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010;363:733–742 [DOI] [PubMed] [Google Scholar]
- 14.Hanson LC, Usher B, Spragens L, et al. : Clinical and economic impact of palliative care consultation. J Pain Symptom Manage 2008;35:340–346 [DOI] [PubMed] [Google Scholar]
- 15.May P, Garrido MM, Cassel JB, et al. : Prospective Cohort Study of Hospital Palliative Care Teams for inpatients with advanced cancer: Earlier consultation is associated with larger cost-saving effect. J Clin Oncol 2015;33:2745–2752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cohen MA, Lee HL: The determinants of spatial distribution of hospital utilization in a region. Med Care 1985;23:27–38 [DOI] [PubMed] [Google Scholar]
- 17.Quan H, Sundararajan V, Halfon P, et al. : Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005;43:1130–1139 [DOI] [PubMed] [Google Scholar]
- 18.Garrido MM, Kelley AS, Paris J, et al. : Methods for constructing and assessing propensity scores. Health Serv Res 2014;49:1701–1720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zou G: A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159:702–706 [DOI] [PubMed] [Google Scholar]
- 20.Reville B, Miller MN, Toner RW, et al. : End-of-life care for hospitalized patients with lung cancer: Utilization of a palliative care service. J Palliat Med 2010;13:1261–1266 [DOI] [PubMed] [Google Scholar]
- 21.Greer JA, Pirl WF, Jackson VA, et al. : Effect of early palliative care on chemotherapy use and end-of-life care in patients with metastatic non-small-cell lung cancer. J Clin Oncol 2012;30:394–400 [DOI] [PubMed] [Google Scholar]
- 22.Gonsalves WI, Tashi T, Krishnamurthy J, et al. : Effect of palliative care services on the aggressiveness of end-of-life care in the Veteran's Affairs cancer population. J Palliat Med 2011;14:1231–1235 [DOI] [PubMed] [Google Scholar]
- 23.Paris J, Morrison RS: Evaluating the effects of inpatient palliative care consultations on subsequent hospice use and place of death in patients with advanced GI cancers. J Oncol Pract 2014;10:174–177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Uppal S, Rice LW, Beniwal A, et al. : Trends in hospice discharge, documented inpatient palliative care services and inpatient mortality in ovarian carcinoma. Gynecol Oncol 2016;143:371–378 [DOI] [PubMed] [Google Scholar]
- 25.Enguidanos S, Vesper E, Lorenz K: 30-day readmissions among seriously ill older adults. J Palliat Med 2012;15:1356–1361 [DOI] [PubMed] [Google Scholar]
- 26.O'Connor NR, Moyer ME, Behta M, et al. : The Impact of Inpatient Palliative Care Consultations on 30-day hospital readmissions. J Palliat Med 2015;18:956–961 [DOI] [PubMed] [Google Scholar]
- 27.Tangeman JC, Rudra CB, Kerr CW, et al. : A hospice-hospital partnership: Reducing hospitalization costs and 30-day readmissions among seriously ill adults. J Palliat Med 2014;17:1005–1010 [DOI] [PubMed] [Google Scholar]
- 28.National Hospice and Palliative Care Organization: Common misconceptions regarding hospice. www.nhpco.org/sites/default/files/public/communications/Outreach/Common_misconceptions_about_hospice.pdf (last accessed March1, 2017)
- 29.Meier DE, Beresford L: Hospitals and hospices partner to extend the continuum of palliative care. J Palliat Med 2007;10:1231–1235 [DOI] [PubMed] [Google Scholar]
- 30.Granda-Cameron C, Behta M, Hovinga M, et al. : Risk factors associated with unplanned hospital readmissions in adults with cancer. Oncol Nurs Forum 2015;42:E257–E268 [DOI] [PubMed] [Google Scholar]
- 31.Montero AJ, Stevenson J, Guthrie AE, et al. : Reducing unplanned medical oncology readmissions by improving outpatient care transitions: A process improvement project at the Cleveland Clinic. J Oncol Pract 2016;12:e594–e602 [DOI] [PubMed] [Google Scholar]
- 32.Yang GM, Neo SH, Lim SZ, et al. : Effectiveness of Hospital Palliative Care Teams for cancer inpatients: A systematic review. J Palliat Med 2016;19:1156–1165 [DOI] [PubMed] [Google Scholar]
- 33.Fadul N, Elsayem A, Palmer JL, et al. : Predictors of access to palliative care services among patients who died at a Comprehensive Cancer Center. J Palliat Med 2007;10:1146–1152 [DOI] [PubMed] [Google Scholar]
- 34.Walling AM, Asch SM, Lorenz KA, et al. : The quality of supportive care among inpatients dying with advanced cancer. Support Care Cancer 2012;20:2189–2194 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.