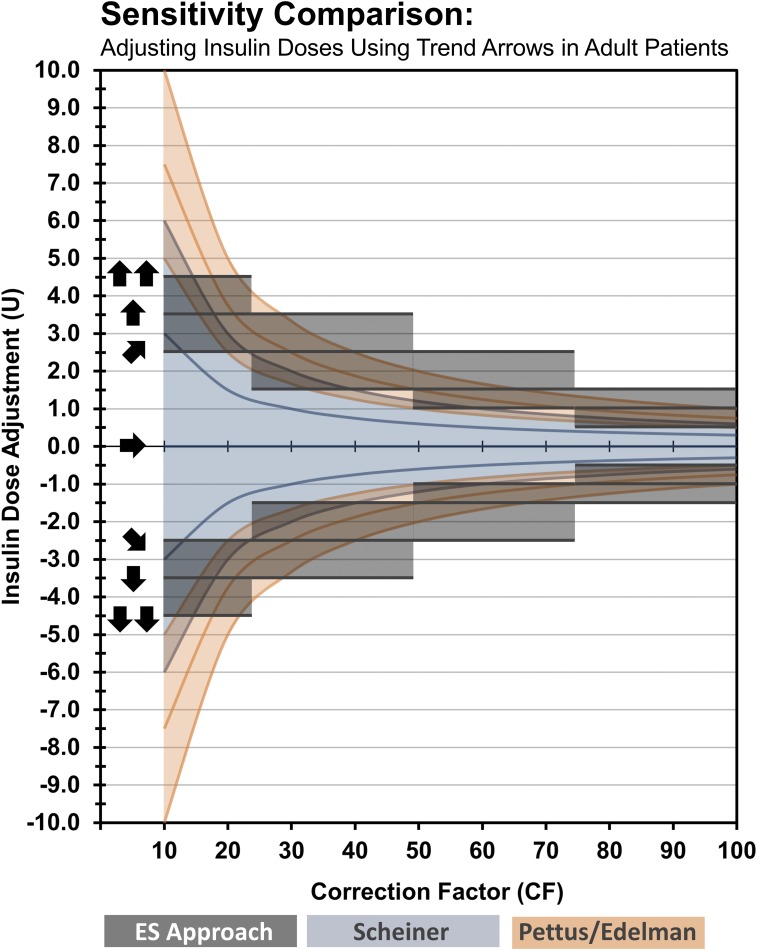
Figure 5.
Sensitivity comparison of methods to adjust insulin doses using trend arrows in adult patients. The figure is a visual comparison of insulin dose adjustments according to previous methods based on anticipated glucose (Scheiner and Pettus/Edelman) and our suggested approach based on insulin sensitivity ranges (Endocrine Society approach). The illustration shows that our approach aligns well with existing methods that indirectly use insulin sensitivity to adjust insulin doses while overcoming some of the limitations (e.g., a need for additional calculations and minimum increments possible for MDI-treated patients). When applied to lower CF ranges (e.g., <25), our approach is more conservative, whereas in the midrange (e.g., 50 to <75), it is more aggressive. However, one must consider that the conversions used in our approach are based on 30 minutes. When considering the anticipated glucose at 1 hour, our suggested dose adjustments become more conservative. For example, a single UP trend arrow indicates that glucose is rising 2 to 3 mg/dL/min. At 30 minutes, the anticipated glucose would be 60 to 90 mg/dL higher. However, the anticipated glucose could be as much as 120 to 180 mg/dL higher at 60 minutes if exposed to other perturbations. If an individual’s CF was 60, our approach would recommend adding 1.5 U of rapid-acting insulin to the premeal bolus. The additional 1.5 U of insulin would be expected to provide additional glucose lowering of 60 mg/dL over the 60 minutes. Given that the 60-minute anticipated glucose could potentially be much higher at 1-hour, our suggestion could be considered conservative. The expected glucose would be closer to target, postprandially, without overcorrecting and without increasing risk for hypoglycemia. As noted, these recommendations are starting points and should be readjusted as experience increases and responsiveness is observed and understood. Conversion: mg/dL × 0.0555 = mmol/L. CF, correction factor in mg/dL indicates glucose lowering per unit of rapid-acting insulin; U, units of rapid-acting insulin.