Abstract
Background & objectives:
Cannabis is a widely used illicit drug and its use is often associated with co-occurring psychiatric disorders. This systematic review was aimed to provide information on the published Indian studies on co-occurring cannabis use disorders and psychiatric disorders.
Methods:
An electronic search of available Indian literature using relevant search terms was carried out in May 2015 and 52 articles in English language published from India were included in the current review.
Results:
Studies on cannabis and associated psychotic disorders (n=16) chiefly described acute episodes with predominant positive symptoms, following cannabis use. Some studies (n=6) observed an overall increased prevalence of all psychiatric disorders and symptoms owing to cannabis use, while others (n=14) elaborated on high rates of substance use in those with psychiatric disorders. The effect of cannabis use on cognitive function was the focus of some of the Indian studies (n=7). All these studies barring one had all male subjects, and a single study described the service delivery model for those with dual diagnosis disorders in India. Most of the research used cross-sectional observational design and focussed on treatment-seeking population.
Interpretation & conclusions:
A review of Indian literature on cannabis use and its association with psychiatric disorders indicates a high co-prevalence of psychotic disorders, especially in vulnerable individuals as well as high rates of co-occurrence of other psychiatric comorbidities. However, there is limited focus on exploring the aetiological association between cannabis use and psychiatric disorders; understanding the neurobiology of this association and management-related issues.
Keywords: Cannabis, comorbidity, dual diagnosis, dual disorders, psychosis, schizophrenia, substance use disorders
Cannabis is the most frequently used illicit psychoactive substance worldwide. In 2012, 125 to 227 million people were estimated to have used cannabis1. The National Survey on Extent, Pattern and Trends of Drug Use in India also found it to be the most common illicit substance of use in the country2.
Cannabis use has been associated with a high incidence of psychiatric disorders3,4. Cannabis use has been found to have a strong association with psychotic illness including schizophrenia5. This co-occurrence, which could also present as dual disorder or dual diagnosis, has important clinical implications as it is often associated with diagnostic challenges, poor treatment outcome, severe illness course and high service utilization. Hence, it is important to study co-occurring cannabis use disorders and psychiatric disorders. The objective of the current review was to highlight salient features of the relevant Indian literature, to discuss the findings of these studies and to highlight the strengths and limitations of the existing work.
Material & Methods
Search strategy: Electronic databases of PubMed and IndMed were searched for relevant publications. The search was carried out in May 2015 and included publications till the month of May 2015. The PubMed, Boolean search was carried out using the combination of ‘diagnosis, dual (psychiatry)’ AND ‘India’. All publications listed using the search term ‘diagnosis, dual (psychiatry)’ were screened for Indian studies on co-occurring cannabis use disorders and psychiatric disorders. IndMed search was carried out using different search terms including ‘alcohol’, ‘cannabis’, ‘opioids’, ‘inhalants’, ‘sedatives’, ‘hallucinogens’, ‘stimulants’, ‘cocaine’, ‘amphetamine type stimulants’, ‘buprenorphine’, ‘pentazocine’, ‘dextropropoxyphene’, ‘heroin’, ‘opium’, ‘afeem’, ‘smack’, ‘morphine’, ‘bhang’, ‘charas’, ‘ganja’, ‘hashish’, ‘benzodiazepines’, ‘zolpidem’, ‘toluene’, ‘LSD’, ‘ketamine’, ‘caffeine’, ‘nicotine’ and ‘tobacco’. Electronic archives of Indian journals on psychiatry and psychology were also searched for relevant studies. Additional published material was identified from the bibliography of the studies screened and evaluated.
Study selection: Only English-language peer-reviewed studies from India conducted among human subjects were included. All published Indian researches on co-occurring substance use disorders and psychiatric disorders, irrespective of the type of substance and psychiatric disorder, were explored. The search was not restricted by the publication type, and various publication types such as original research articles, review articles, case reports, case series and trials (including randomized as well as open-label trials) were explored for the purpose of the current review. Studies that did not include cannabis use disorders were excluded. Further, experimental research not conducted at an Indian centre and animal studies were also excluded.
Data extraction and analysis: Information was extracted using a structured proforma from the studies that met the above-mentioned inclusion and exclusion criteria. Data were extracted pertaining to comorbid cannabis use disorders and psychiatric disorders. Two authors, using pre-defined criteria, extracted the information.
Results
Fifteen studies were found following search using Boolean search terms ‘diagnosis, dual (psychiatry)’ AND ‘India’, of which 10 were found relevant and included in the review. PubMed search with ‘diagnosis, dual (psychiatry)’ yielded 2957 studies, nine were relevant and included in the review. A search of IndMed archives led to 33 relevant studies. Twenty-eight studies on co-occurring cannabis use disorder and psychiatric disorders were included in the current review (Table I). Further, 24 studies on various psychoactive substances (including cannabis) and psychiatric disorders were included in the current review (Table II).
Table I.
Studies that have explored co-occurring cannabis use disorders and psychiatric disorders in Indian setting (arranged in ascending order of year of publication)
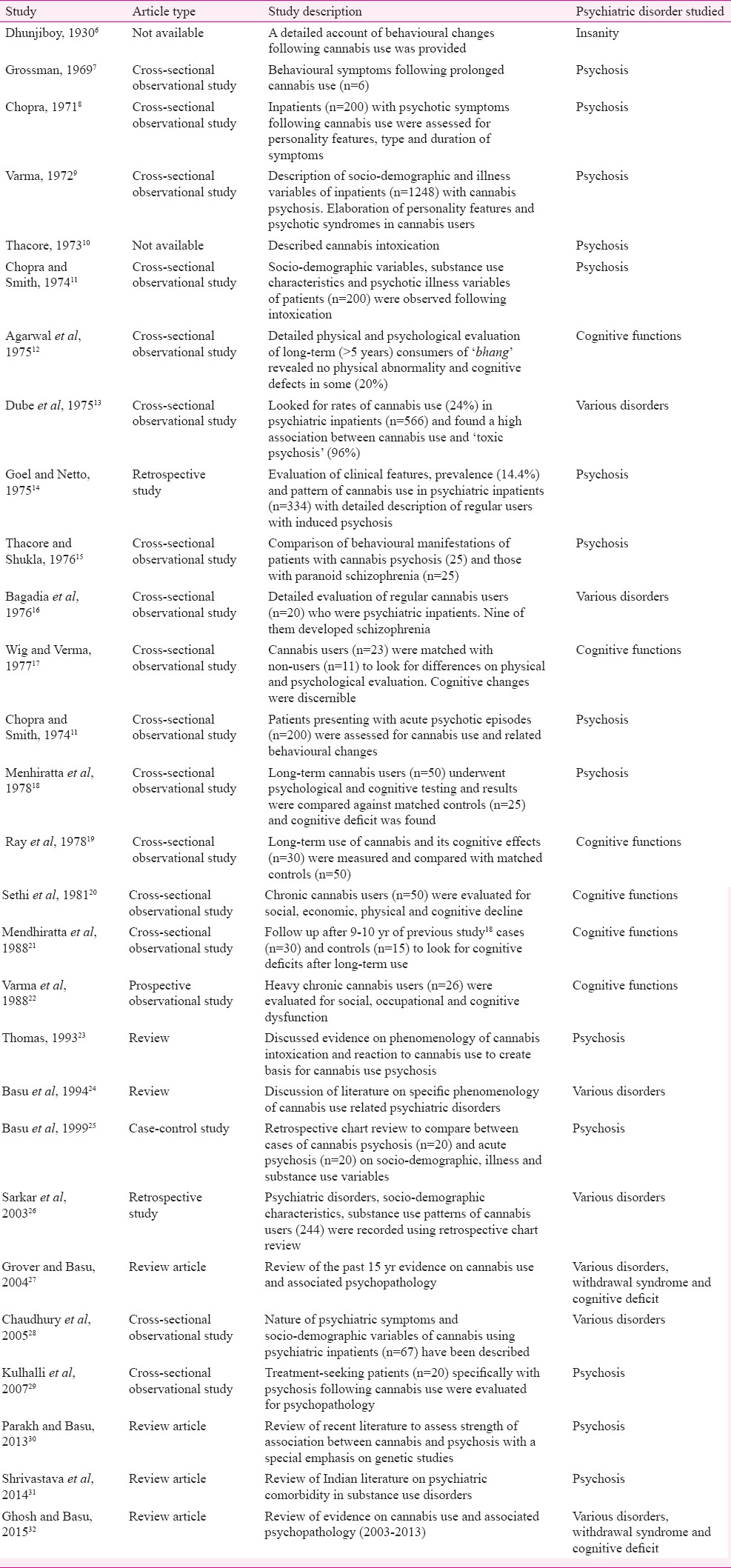
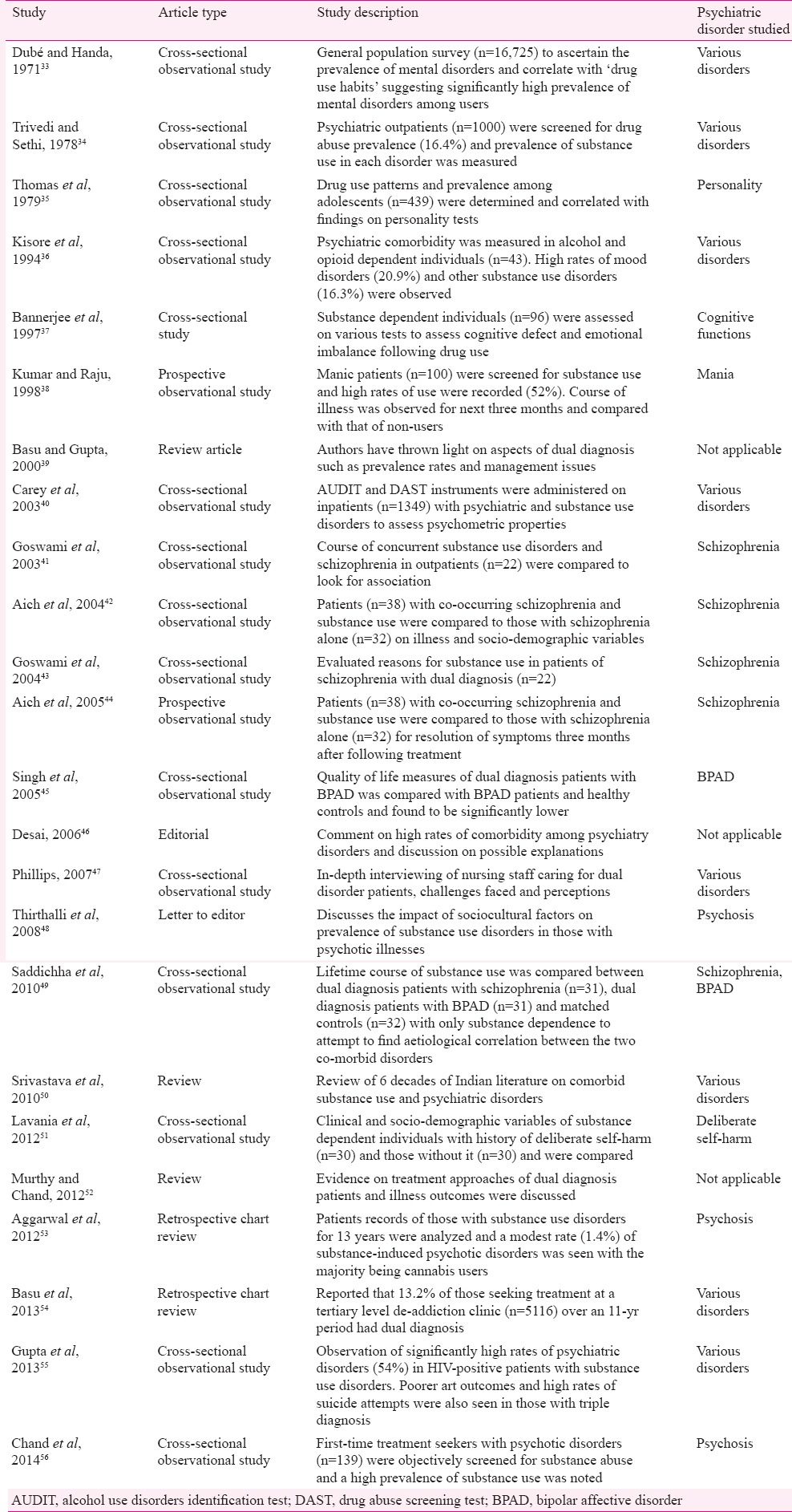
Table II.
Studies that have explored co-occurring various substance (including cannabis) use disorders and psychiatric disorders in Indian setting (arranged in ascending order of year of publication)
Types of studies: Thirty one studies included in the current review were cross-sectional observational studies7,8,9,10,11,12,13,14,15,17,18,19,20,21,28,33,34,35,36,37,38,40,41,42,43,45,47,49,51,55,56. Other study types included reviews (nine publications)23,24,27,30,31,32,39,50,52, prospective observational studies (three publications)22,29,44, retrospective chart reviews (three publications)26,53,54, case-control study (one publication)25, letter to editor (one publication)48, case series (one publication)10 and editorial (one publication)46.
Study population: Most studies were conducted among male subjects and included treatment-seeking individuals. Two studies reported findings from general population33,48. One study reported on family members and treatment centre staff47.
Psychoactive substances studied: Cannabis was the exclusive psychoactive substance studied in 27 Indian studies on dual disorders6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32. Twenty three studies reported findings on more than one psychoactive substances including cannabis33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,51,52,53,54,55,56.
Psychiatric disorders studied: Psychoses were studied in 27 publications6,7,8,9,10,11,14,15,16,17,18,19,20,21,22,23,25,29,30,31,41,42,43,44,49,53,56. Other psychiatric disorders studied included bipolar affective disorder (BPAD) (three publications)38,45,49. Cognitive functions were explored in eight publications12,17,18,19,20,21,22,37. More than one psychiatric disorder was explored in 14 publications27,32,33,34,38,39,40,45,48,49,52,54,56,57.
Time trends in publications on co-occurring cannabis use disorders and psychiatric disorders: The first published journal article on co-occurring cannabis use disorder and psychiatric disorders dated back to the 1930s. During the four decades from the 1960s to 1990s, the largest proportion of publications on dual disorders focussed exclusively on cannabis. However, the contribution of publication that focussed on cannabis use reduced during the 2000s and 2010s (Figure).
Figure.
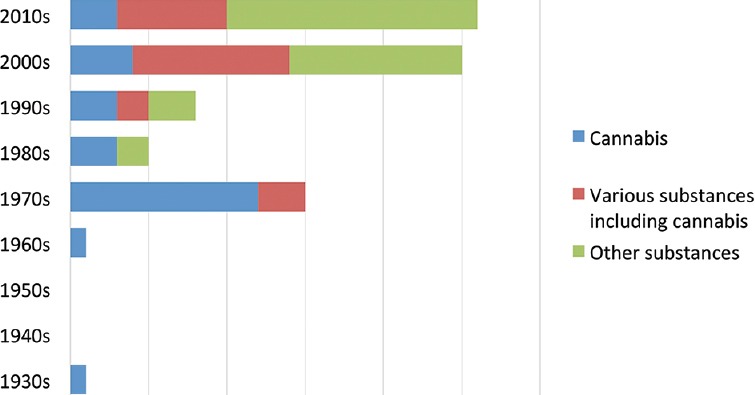
Time trends of publications on co-occurring cannabis use disorder and psychiatric disorders from India.
Cannabis use disorders and psychotic disorders: Sixteen studies described comorbid cannabis use disorders and psychoses6,9,10,11,14,15,16,23,24,25,29,30,31,42,44,53. Dhunjiboy6 described ‘Indian hemp insanity’ as an adverse reaction to cannabis use. Varma9 described socio-demographic attributes 1248 inpatients receiving treatment for psychotic disorder associated with long-term use of cannabis. Thacore10 described four long-term bhang users who developed schizophrenia-like psychosis associated with thought and perceptual disturbances in the absence of a state of confusion. Chopra and Smith11 described the clinical and demographic findings of 200 Indian patients who presented with symptoms, suggestive of psychosis due to use of cannabis Five per cent individuals were found to have presented with a pre-existing psychiatric illness, while 58 per cent were found to have covert psychopathology or a previous history of psychiatric disorders.
Goel and Netto14 reported that regular cannabis users presented with hyperactivity, mood changes, delusions and hallucinations. Thacore and Shukla15 reported similar presentations. Bagadia et al16 explored the causes for vulnerability to psychiatric disorders in daily cannabis users (n=20). Thomas23 reported the phenomenology of cannabis use disorders to be vague and of fleeting nature of symptoms. Basu et al24 classified the psychological effects of cannabis into three separate syndromes viz. intoxication syndrome, cannabis psychosis syndrome and amotivational syndrome. Basu et al25 did a retrospective case control review of 22 patients with cannabis psychosis and 20 control patients of acute psychotic episode to find an association.
Aich et al42 reported a prevalence rate of 54.3 per cent. Sixty per cent of them were using cannabis along with tobacco while 42 and 5 per cent were using alcohol and opioids, respectively. On a longitudinal examination of the same sample, it was seen that the substance-using group presented with predominantly positive symptoms (63.2%) in comparison and also had a faster rate of remission of these symptoms upon treatment. The non-substance-using group showed significantly more negative symptoms44. Similarly, Kulhalli et al29 examined 20 inpatient cases of psychosis following cannabis use during a weeklong period of abstinence. On further assessment, seven patients were diagnosed with schizophrenia, 12 were diagnosed with BPAD mania with psychotic symptoms while one had psychotic symptoms not amounting to a diagnosis. The subjects showed increased psychomotor activity, multiple delusions and hallucinations along with unusual thought content. Shrivastava et al31 and Grover and Basu27 discussed the theories of an association between cannabis use and schizophrenia such as self-medication hypothesis, vulnerability hypothesis, acute psychotic effect of cannabis use and occurrence of common socio-demographic and genetic factors in those affected by cannabis use and psychosis.
Cannabis use disorders and various psychiatric disorders: Five studies7,13,26,28,32 assessed the comorbid cannabis use disorders and various psychiatric disorders. Grossman7 described psychiatric symptoms in six individuals who were regular users of cannabis. Dube et al13, Sarkar et al26 and Chaudhury et al28 reported a rate of 24-52 per cent of cannabis misuse in psychiatric hospital admissions. Sarkar et al26 found that the common psychiatric comorbidities with cannabis use were other substance use disorders (34%), cannabis psychosis (21%), schizophrenia (14%), mania with psychosis (12%), and unspecified psychosis (7%). Ghosh and Basu32 reported a high strength of association between cannabis use and psychiatric disorders, chiefly schizophrenia.
Cannabis use disorders and cognitive function: Seven studies12,17,18,19,20,21,22 assessed cognitive functioning of cannabis users. Agarwal et al12 & Wig and Varma17 reported cognitive disturbances such as poor attention span and memory deficits in bhang users. Mendhiratta et al18 reported delayed reaction time, poor concentration and poor time estimation in long-term (>10 years) cannabis users. Marked deterioration in cognitive functioning continued to persist in a follow up study21. Similar findings were reported by Ray et al19 in frequent cannabis users.
Conversely, Sethi et al20 and Varma et al22 found no significant cognitive deficit, physical health, social functioning or work performance in long-term daily cannabis users. Bannerjee et al37 compared the cognitive functioning of opioid users, cannabis users and matched controls and reported most deficit in opioid users.
Studies on various substance use disorders (including cannabis use disorders) and psychiatric disorders: Fourteen studies on dual disorders were included33,34,37,38,39,40,41,43,45,48,49,52,54,57. Dubé & Handa33 showed a five per cent prevalence rate of dual diagnosis in a community survey (n=16,725). Trivedi & Sethi34 reported 16.4 per cent prevalence of substance misuse in psychiatric outpatients (n=1000). Kumar and Raju38 reported cannabis abuse in 26.7 per cent individuals with mania. Carey et al40 reported lower prevalence of cannabis use in people with mental illness in India as compared to other countries. Thirthalli et al48 also highlighted low prevalence of cannabis dependence in patients of schizophrenia (n=258) in a rural Indian community. Reviews on issues related to the management of dual diagnosis disorders recommended that psychosocial interventions should be implemented along with pharmacotherapy and that the integrated treatment approach is superior39,52.
Goswami et al41 mapped the course of schizophrenia onto the course of substance use in a retrospective study design. Goswami et al43 contrasted the psychopathology of patients with schizophrenia who used psychoactive substances [alcohol (n=22), cannabis and opioids (n=22)] with patients of schizophrenia who did not use these substances. Alcohol was found to be used more commonly as a self-medicating agent than opioids and cannabis. In general, patients with dual diagnosis reported lesser emotional distress and mitigation of certain symptoms as one of the purposes of using substance.
Singh et al45 reported the findings on quality of life and associated parameters in patients with dual diagnosis of BPAD and substance dependence. However, the findings of the cannabis users have been presented clubbed together with opioid users and prescription drug users that comprised 37.5 per cent of the study group. Saddichha et al49 did a comparative analysis of patients with dual diagnosis and ‘pure’ substance use disorders. All patients with schizophrenia and 80 per cent of patients with BPADs were diagnosed with cannabis dependence while 28 per cent of the participants with ‘pure’ substance use disorders had cannabis dependence.
The additive effect of substance use as well the occupational distress faced by female commercial sex workers seeking psychiatric treatment has been studied by Pandiyan et al57. Most common substances used were alcohol (100%), tobacco (74%), opioids (14%), cocaine (6%) and cannabis (6%).
Retrospective studies by Aggarwal et al53 and Basu et al54 on substance-induced psychotic disorders implicated cannabis as one of the chief causative agents for psychosis. Chand et al56 noted a 20 per cent prevalence of substance dependence among treatment naive first episode psychosis patients.
Studies on service delivery for individuals with co-occurring cannabis use disorders and psychiatric disorders: In a qualitative study of care providers of dual diagnosis patients Phillips47 reported that depressive and anxiety disorders commonly co-occurred in patients with alcohol use, while schizophrenia was usually observed in cannabis-dependent individuals.
Discussion
There is limited published literature on co-occurring cannabis use disorders and psychiatric disorders from India50,58,59. Most studies have used cross-sectional observational design and there are only a few studies that have followed up study subjects prospectively, while some have done a retrospective chart review. The existing literature on co-occurring cannabis use disorders and psychiatric disorders has explored only limited domains. This is despite cannabis being one of the most commonly used substances among those with psychiatric disorder. An update on the progress on exploring the detrimental and sometimes beneficial effects of cannabis use on various psychiatric disorders suggests that we still have a long road of exploration ahead of us60.
Most of the studies on comorbid cannabis use disorders and psychiatric disorders have focussed on psychoses. Reviews on the subject uphold the phenomenology described in the reviewed literature following long-term and short-term cannabis use61. The information gathered indicates an association of psychiatric comorbidity and cognitive decline in individuals with cannabis use disorders. A collective analysis on the data generated on behavioural changes associated with cannabis use suggests similar findings62. Studies in recent years among patients with co-occurring schizophrenia and substance use disorders have supported the ‘vulnerability hypothesis model’ to explain the association between cannabis use and schizophrenia. Research reiterates that cannabis use could interact with pre-existing genetic and environmental factors to lead to symptoms of schizophrenia63. It is to be mentioned here that antipsychotic potential of cannabidiol is being explored while support for vulnerability of cannabis users to develop psychosis gathers ground64.
Cognitive effect of cannabis is a commonly explored area in Indian studies. The studies have commonly chosen chronic users of cannabis and compared the deficits between weaker and stronger preparation users to substantiate their findings. The reports suggested a decline in performance among those with long-term cannabis use. The predominant cognitive deficit observed in these studies was poor attention and concentration along with memory impairment. The preponderance of developing cognitive defects and psychotic disturbances in younger and more frequent users of cannabis is a finding of recent research as well65.
Overall, the literature review points towards a high frequency of psychiatric symptoms in those with substance use disorders with a specific preponderance of cannabis-associated comorbidity of both psychotic and affective disorders with a higher strength of association with psychotic syndromes. A systematic review of worldwide literature echoes these findings66. Another longitudinal study on patients with mood disorders found a lack of association between course of the illness and cannabis use67.
In conclusion, several Indian studies have described the adverse effects of cannabis use, and the review of research suggests a high prevalence of psychiatric disorders among those with cannabis use disorders. The psychiatric comorbidity usually found in cannabis users was schizophrenia and other psychotic disorders. Research suggests that cannabis use alters the age of onset, course and presentation of psychotic illness in vulnerable individuals. Further high-quality research on cannabis use-associated psychosis is desired to understand impact of one on the other. Findings suggest that cannabis use has an association with other mental disorders indicating a modest strength of association with mood and anxiety spectrum disorders. Cognitive deficits are frequently reported among chronic and heavy cannabis users. Exploration of neurobiological aspects of dual disorders of cannabis use and psychiatric disorders has been inconclusive and Indian literature on this aspect is scarce.
Footnotes
Conflicts of Interest: None.
References
- 1.New York: United Nations Publication; 2014. United Nations Office on Drugs and Crime. World Drug Report 2014. [Google Scholar]
- 2.Ray R, editor. The Extent, Pattern and Trends of Drug Abuse in India - National Survey: New Delhi. Ministry of Social Justice and Empowerment, Government of India and United Nations Office on Drugs and Crime. 2004 [Google Scholar]
- 3.Leweke FM, Koethe D. Cannabis and psychiatric disorders: It is not only addiction. Addict Biol. 2008;13:264–75. doi: 10.1111/j.1369-1600.2008.00106.x. [DOI] [PubMed] [Google Scholar]
- 4.Johns A. Psychiatric effects of cannabis. Br J Psychiatry. 2001;178:116–22. doi: 10.1192/bjp.178.2.116. [DOI] [PubMed] [Google Scholar]
- 5.Hall W, Degenhardt L. Cannabis use and the risk of developing a psychotic disorder. World Psychiatry. 2008;7:68–71. doi: 10.1002/j.2051-5545.2008.tb00158.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dhunjiboy J. A brief resume of the types of insanity commonly met with in India with a full description of “Indian hemp insanity” peculiar to the country. J Ment Sci. 1930;75:254. [Google Scholar]
- 7.Grossman W. Adverse reactions associated with Cannabis products in India. Ann Intern Med. 1969;70:529–33. doi: 10.7326/0003-4819-70-3-529. [DOI] [PubMed] [Google Scholar]
- 8.Chopra GS. Marijuana and adverse psychotic reactions. Evaluation of different factors involved. Bull Narc. 1971;23:15–22. [PubMed] [Google Scholar]
- 9.Varma L. Cannabis psychosis. Indian J Psychiatry. 1972;14:241. [Google Scholar]
- 10.Thacore VR. Bhang psychosis. Br J Psychiatry. 1973;123:225–9. doi: 10.1192/bjp.123.2.225. [DOI] [PubMed] [Google Scholar]
- 11.Chopra GS, Smith JW. Psychotic reactions following cannabis use in East Indians. Arch Gen Psychiatry. 1974;30:24–7. doi: 10.1001/archpsyc.1974.01760070014002. [DOI] [PubMed] [Google Scholar]
- 12.Agarwal A, Sethi B, Gupta S. Physical and cognitive effects of chronic Bhang (Cannabis) intake. Indian J Psychiatry. 1975;17:1. [Google Scholar]
- 13.Dube KC, Jain SC, Basu AK, Kumar N. Patterns of the drug habit in hospitalized psychiatric patients. Bull Narc. 1975;27:1–10. [PubMed] [Google Scholar]
- 14.Goel D, Netto D. Cannabis: The habit and psychosis. Indian J Psychiatry. 1975;17:238–43. [Google Scholar]
- 15.Thacore VR, Shukla SR. Cannabis psychosis and paranoid schizophrenia. Arch Gen Psychiatry. 1976;33:383–6. doi: 10.1001/archpsyc.1976.01770030081012. [DOI] [PubMed] [Google Scholar]
- 16.Bagadia V, Copalani J, Pradhan P, Shah L. Habitual use of Cannabis indica in psychiatric patients. Indian J Psychiatry. 1976;18:141–6. [Google Scholar]
- 17.Wig NN, Varma VK. Patterns of long-term heavy cannabis use in north India and its effects on cognitive functions: A preliminary report. Drug Alcohol Depend. 1977;2:211–9. doi: 10.1016/0376-8716(77)90028-x. [DOI] [PubMed] [Google Scholar]
- 18.Menhiratta SS, Wig NN, Verma SK. Some psychological correlates of long-term heavy cannabis users. Br J Psychiatry. 1978;132:482–6. doi: 10.1192/bjp.132.5.482. [DOI] [PubMed] [Google Scholar]
- 19.Ray R, Prabhu GG, Mohan D, Nath LM, Neki JS. The association between chronic cannabis use and cognitive functions. Drug Alcohol Depend. 1978;3:365–8. doi: 10.1016/0376-8716(78)90006-6. [DOI] [PubMed] [Google Scholar]
- 20.Sethi BB, Trivedi JK, Singh H. Long term effects of cannabis. Indian J Psychiatry. 1981;23:224–9. [PMC free article] [PubMed] [Google Scholar]
- 21.Mendhiratta SS, Varma VK, Dang R, Malhotra AK, Das K, Nehra R. Cannabis and cognitive functions: A re-evaluation study. Br J Addict. 1988;83:749–53. doi: 10.1111/j.1360-0443.1988.tb00506.x. [DOI] [PubMed] [Google Scholar]
- 22.Varma VK, Malhotra AK, Dang R, Das K, Nehra R. Cannabis and cognitive functions: A prospective study. Drug Alcohol Depend. 1988;21:147–52. doi: 10.1016/0376-8716(88)90061-0. [DOI] [PubMed] [Google Scholar]
- 23.Thomas H. Psychiatric symptoms in cannabis users. Br J Psychiatry. 1993;163:141–9. doi: 10.1192/bjp.163.2.141. [DOI] [PubMed] [Google Scholar]
- 24.Basu D, Malhotra A, Varma VK. Cannabis related psychiatric syndromes: A selective review. Indian J Psychiatry. 1994;36:121–8. [PMC free article] [PubMed] [Google Scholar]
- 25.Basu D, Malhotra A, Bhagat A, Varma VK. Cannabis psychosis and acute schizophrenia. A case-control study from India. Eur Addict Res. 1999;5:71–3. doi: 10.1159/000018968. [DOI] [PubMed] [Google Scholar]
- 26.Sarkar J, Murthy P, Singh SP. Psychiatric morbidity of cannabis abuse. Indian J Psychiatry. 2003;45:182–8. [PMC free article] [PubMed] [Google Scholar]
- 27.Grover S, Basu D. Cannabis and psychopathology: Update 2004. Indian J Psychiatry. 2004;46:299–309. [PMC free article] [PubMed] [Google Scholar]
- 28.Chaudhury S, Sudarsanan S, Salujha SK, Srivastava K. Cannabis use in psychiatrie patients. Med J Armed Forces India. 2005;61:117–20. doi: 10.1016/S0377-1237(05)80004-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kulhalli V, Isaac M, Murthy P. Cannabis-related psychosis: Presentation and effect of abstinence. Indian J Psychiatry. 2007;49:256–61. doi: 10.4103/0019-5545.37665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Parakh P, Basu D. Cannabis and psychosis: Have we found the missing links? Asian J Psychiatr. 2013;6:281–7. doi: 10.1016/j.ajp.2013.03.012. [DOI] [PubMed] [Google Scholar]
- 31.Shrivastava A, Johnston M, Terpstra K, Bureau Y. Cannabis and psychosis: Neurobiology. Indian J Psychiatry. 2014;56:8–16. doi: 10.4103/0019-5545.124708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ghosh A, Basu D. Cannabis and psychopathology: The meandering journey of the last decade. Indian J Psychiatry. 2015;57:140–9. doi: 10.4103/0019-5545.158134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dubé KC, Handa SK. Drug use in health and mental illness in an Indian population. Br J Psychiatry. 1971;118:345–6. doi: 10.1192/bjp.118.544.345. [DOI] [PubMed] [Google Scholar]
- 34.Trivedi J, Sethi B. Drug abuse in psychiatric patients. Indian J Psychiatry. 1978;21:345–8. [Google Scholar]
- 35.Thomas MG, Mohan D, Sahasi G, Prabhu GG. Personality and attitude correlates of drug abuse amongst students of a high school in Delhi: A replicated study. Indian J Med Res. 1979;69:990–5. [PubMed] [Google Scholar]
- 36.Kisore P, Lal N, Trivedi JK, Dalal PK, Aga VM. A study of comorbidity in psychoactive substance dependence patients. Indian J Psychiatry. 1994;36:133–7. [PMC free article] [PubMed] [Google Scholar]
- 37.Bannerjee S, Mukhopadhyay A, Shukla V. Cognitive deterioration of male drug addicts. J Indian Acad Appl Psychol. 1997;23:13–8. [Google Scholar]
- 38.Kumar PN, Raju SS. Impact of substance abuse comorbidity on psychopathology and pattern of remission in mania. Indian J Psychiatry. 1998;40:357–63. [PMC free article] [PubMed] [Google Scholar]
- 39.Basu D, Gupta N. Management of “dual diagnosis” patients: Consensus, controversies and considerations. Indian J Psychiatry. 2000;42:34–47. [PMC free article] [PubMed] [Google Scholar]
- 40.Carey KB, Carey MP, Chandra PS. Psychometric evaluation of the alcohol use disorders identification test and short drug abuse screening test with psychiatric patients in India. J Clin Psychiatry. 2003;64:767–74. doi: 10.4088/jcp.v64n0705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Goswami S, Singh G, Mattoo SK, Basu D. Courses of substance use and schizophrenia in the dual-diagnosis patients: Is there a relationship? Indian J Med Sci. 2003;57:338–46. [PubMed] [Google Scholar]
- 42.Aich TK, Sinha VK, Khess CR, Singh S. Demographic and clinical correlates of substance abuse comorbidity in schizophrenia. Indian J Psychiatry. 2004;46:135–9. [PMC free article] [PubMed] [Google Scholar]
- 43.Goswami S, Mattoo SK, Basu D, Singh G. Substance-abusing schizophrenics: Do they self-medicate? Am J Addict. 2004;13:139–50. doi: 10.1080/10550490490435795. [DOI] [PubMed] [Google Scholar]
- 44.Aich T, Sinha V, Khess C, Singh S. Substance abuse co-morbidity in schizophrenia: An inpatient study of course and outcome. Indian J Psychiatry. 2005;47:33–8. [Google Scholar]
- 45.Singh J, Mattoo SK, Sharan P, Basu D. Quality of life and its correlates in patients with dual diagnosis of bipolar affective disorder and substance dependence. Bipolar Disord. 2005;7:187–91. doi: 10.1111/j.1399-5618.2004.00173.x. [DOI] [PubMed] [Google Scholar]
- 46.Desai NG. Comorbidity in psychiatry: Way forward or a conundrum? Indian J Psychiatry. 2006;48:75–7. doi: 10.4103/0019-5545.31593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Phillips PA. Dual diagnosis: An exploratory qualitative study of staff perceptions of substance misuse among the mentally ill in Northern India. Issues Ment Health Nurs. 2007;28:1309–22. doi: 10.1080/01612840701686468. [DOI] [PubMed] [Google Scholar]
- 48.Thirthalli J, Venkatesh BK, Gangadhar BN. Psychoses and illicit drug use: Need for cross-cultural studies. Acta Psychiatr Scand. 2008;118:86. doi: 10.1111/j.1600-0447.2008.01209.x. [DOI] [PubMed] [Google Scholar]
- 49.Saddichha S, Sur S, Sinha BN, Khess CR. How is substance use linked to psychosis. A study of the course and patterns of substance dependence in psychosis? Subst Abus. 2010;31:58–67. doi: 10.1080/08897070903442699. [DOI] [PubMed] [Google Scholar]
- 50.Srivastava A, Sreejayan K, Joseph AM, Sharma PS. Indian research on comorbidities. Indian J Psychiatry. 2010;52(Suppl 1):S246–9. doi: 10.4103/0019-5545.69240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lavania S, Ram D, Praharaj SK, Khan AH, Pattojoshi A. Deliberate self-harm in nondepressed substance-dependent patients. J Addict Med. 2012;6:247–52. doi: 10.1097/ADM.0b013e31826508c0. [DOI] [PubMed] [Google Scholar]
- 52.Murthy P, Chand P. Treatment of dual diagnosis disorders. Curr Opin Psychiatry. 2012;25:194–200. doi: 10.1097/YCO.0b013e328351a3e0. [DOI] [PubMed] [Google Scholar]
- 53.Aggarwal M, Banerjee A, Singh SM, Mattoo SK, Basu D. Substance-induced psychotic disorders: 13-year data from a de-addiction centre and their clinical implications. Asian J Psychiatr. 2012;5:220–4. doi: 10.1016/j.ajp.2011.11.008. [DOI] [PubMed] [Google Scholar]
- 54.Basu D, Sarkar S, Mattoo S. Psychiatric comorbidity in patients with substance use disorders attending an addiction treatment center in India over 11 years: Case for a specialized ‘dual diagnosis clinic’. J Dual Diagn. 2013;9:23–9. [Google Scholar]
- 55.Gupta M, Kumar K, Garg PD. Dual diagnosis vs triple diagnosis in HIV: A comparative study to evaluate the differences in psychopathology and suicidal risk in HIV positive male subjects. Asian J Psychiatr. 2013;6:515–20. doi: 10.1016/j.ajp.2013.06.012. [DOI] [PubMed] [Google Scholar]
- 56.Chand P, Thirthalli J, Murthy P. Substance use disorders among treatment naive first-episode psychosis patients. Compr Psychiatry. 2014;55:165–9. doi: 10.1016/j.comppsych.2013.07.075. [DOI] [PubMed] [Google Scholar]
- 57.Pandiyan K, Chandrasekhar H, Madhusudhan S. Psychological morbidity among female commercial sex workers with alcohol and drug abuse. Indian J Psychiatry. 2012;54:349–51. doi: 10.4103/0019-5545.104822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Murthy P, Manjunatha N, Subodh BN, Chand PK, Benegal V. Substance use and addiction research in India. Indian J Psychiatry. 2010;52(Suppl 1):S189–99. doi: 10.4103/0019-5545.69232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kumar V, Kumar P, Bhatia M, Jhanjee A. Substance abuse and comorbidity. Delhi Psychiatry J. 2010;13:36–42. [Google Scholar]
- 60.Haney M, Evins AE. Does cannabis cause, exacerbate or ameliorate psychiatric disorders? An oversimplified debate discussed. Neuropsychopharmacology. 2016;41:393–401. doi: 10.1038/npp.2015.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wilkinson ST, Radhakrishnan R, D’Souza DC. Impact of cannabis use on the development of psychotic disorders. Curr Addict Rep. 2014;1:115–28. doi: 10.1007/s40429-014-0018-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Repp K, Raich A. Washington: Department of Health and Human Services; 2014. Marijuana and Health: A Comprehensive Review of 20 Years of Research. [Google Scholar]
- 63.Green IW, Glausier JR. Different paths to core pathology: The equifinal model of the Schizophrenia syndrome. Schizophr Bull. 2016;42:542–9. doi: 10.1093/schbul/sbv136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Manseau MW, Goff DC. Cannabinoids and schizophrenia: Risks and therapeutic potential. Neurotherapeutics. 2015;12:816–24. doi: 10.1007/s13311-015-0382-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Albertella L, Le Pelley ME, Copeland J. Cannabis use, schizotypy, and negative priming. Psychiatry Res. 2015;228:404–10. doi: 10.1016/j.psychres.2015.05.074. [DOI] [PubMed] [Google Scholar]
- 66.Moore TH, Zammit S, Lingford-Hughes A, Barnes TR, Jones PB, Burke M, et al. Cannabis use and risk of psychotic or affective mental health outcomes: A systematic review. Lancet. 2007;370:319–28. doi: 10.1016/S0140-6736(07)61162-3. [DOI] [PubMed] [Google Scholar]
- 67.Feingold D, Weiser M, Rehm J, Lev-Ran S. The association between cannabis use and mood disorders: A longitudinal study. J Affect Disord. 2015;172:211–8. doi: 10.1016/j.jad.2014.10.006. [DOI] [PubMed] [Google Scholar]


