Abstract
Objective
Hypersensitivity to carbon dioxide (CO2)-enriched air may be a promising risk marker for anxiety disorders. Among adult and adolescent samples, heterogeneity in distress response to the CO2 challenge task indexes three underlying classes of individuals, which distinguish between sustained and acute threat response as markers for internalizing disorders, broadly, and anxiety disorders, specifically. The present study examines latent classes in children’s response to the CO2 challenge task to clarify the association of CO2 hypersensitivity with anxiety and internalizing symptomatology in childhood.
Method
Healthy children from a community twin sample (N = 538; 9–13 years) rated anxious distress every 2 minutes while breathing air enriched to 7.5% CO2 for 8 minutes. Latent growth mixture modeling evaluated potential classes of individuals with characteristic trajectories of distress during the task to clarify the association with internalizing disorder symptoms and related traits (e.g., anxiety sensitivity, irritability).
Results
While all participants reported increased distress during the task, inter-individual heterogeneity in distress indexed three underlying classes: a consistently low class (“low”), a consistently high class (“high”), and participants who demonstrated markedly increased acute distress (“acute”). Compared to the low class, the high class reported greater internalizing psychopathology, whereas membership in the acute class was associated with experiencing a panic-like event during the task.
Conclusion
As in older individuals, three distinct trajectories emerged to capture inter-individual heterogeneity in children’s distress during the CO2 challenge task. These classes were distinguished by clinical validators that reinforce the association of CO2 hypersensitivity and internalizing disorder phenotypes in children.
Keywords: carbon dioxide hypersensitivity, children, anxiety, anxiety disorders, latent growth mixture modeling
INTRODUCTION
Carbon dioxide (CO2) hypersensitivity, anxiety in response to CO2-enriched air, relates to risk for anxiety psychopathology.1,2 Among adults, CO2 hypersensitivity is related to anxiety psychopathology, especially panic disorder,3–5 panic attacks,6 and anxiety-related traits (e.g., anxiety sensitivity).7 Additionally, in adults CO2 hypersensitivity is associated with family history of an anxiety disorder,8,9 which implicates genetic liability. However, CO2 hypersensitivity is also associated with social anxiety disorder,10 generalized anxiety disorder (GAD),11 and posttraumatic stress disorder,12 which suggests further research to clarify the manifestation and clinical meaning of CO2 hypersensitivity.
Comparatively less research examines children. Extant studies suggest CO2 hypersensitivity in children with selected current anxiety disorders,13–15 particularly separation anxiety disorder,3,16 and those at elevated familial risk for anxiety disorders.17 The prevalence and phenomenology of anxiety changes over the course of development, especially after puberty.18,19 Evidence of multi- and equifinality in adult anxiety disorders20 demonstrates a need to evaluate correlates of adult anxiety disorders in child samples. All prior research on CO2 hypersensitivity in children was conducted in case-control samples and did not examine clinical correlates beyond child or parent diagnosis.14,15 To understand the role of CO2 hypersensitivity to models of risk prediction, it is critical to examine the manifestations of CO2 hypersensitivity in an unselected cohort of typically developing children assessed for a broad range of internalizing psychopathology.21 Clarifying the clinical implications of childhood CO2 hypersensitivity may also inform the prediction, assessment, and treatment of pediatric anxiety, which affects a large number of children and adolescents18 and often persists and broadens in adulthood.19
Breathing CO2-enriched air consistently produces trajectories of elevated distress with considerable inter-individual variability among both clinical and community samples.2 While various measures have been applied to index CO2 responses, self-reported distress relates most strongly to clinical outcomes. However, specificity of association to anxiety disorders may be obscured by methodological limitations and variability in characterization of CO2 hypersensitivity in prior studies. For example, peak anxiety does not discriminate between sustained anxiety and acute response to the task, whereas rate of increase risks conflating participants with sustained elevated anxiety and those who are consistently low. Additionally, whereas reporting a panic-like experience during the task indexes a particularly relevant construct, it may be highly specific to panic-related syndromes and fail to capture the role of CO2 hypersensitivity in other anxiety and internalizing disorders.22
Our group has previously demonstrated that the latent growth mixture model (LGMM) summarizes heterogeneity in the baseline, peak, and trajectory of the participant’s distress during the CO2 challenge task. This approach disaggregates sustained and acute distress in response to threat and, in prior work, identified three distinct classes of individuals: a consistently highly distressed class (“high”), a consistently mildly distressed class (“low”), and a class comprised of individuals who initially report low distress but who become acutely and markedly distressed when breathing CO2-enriched air (“acute”). Research in two older samples (i.e., university students23 and a community sample of adolescents22) demonstrates the utility of this approach while showing that other response measures (e.g., respiratory rate) add little to the understanding of clinical outcomes.23
The Present Study
The present study addresses three questions regarding CO2 hypersensitivity in children. First, is the pattern of temporal responding during the task in children similar to that seen in adolescents and adults? Second, how does CO2 hypersensitivity relate to clinical anxiety-related correlates in children? Third, do relationships extend beyond anxiety to a broader set of internalizing phenotypes?
We hypothesized that we would recover the expected three-class solution to clarify the manifestation of CO2 hypersensitivity among children. Based on prior research, we further hypothesized that, compared to the low class, the high and acute classes would report greater severity of anxiety symptoms and associated traits. Additionally, to demonstrate divergent validity of the model, it was hypothesized that class membership would not be associated with extraversion or behavioral activation. Finally, to evaluate the specificity of CO2 hypersensitivity to anxiety and related phenomena, exploratory analyses examined depression symptoms and irritability in relation to class membership.
METHOD
Participants
This study was conducted as part of the Virginia Commonwealth University (VCU) Juvenile Anxiety Study24: a genetic epidemiological study of internalizing disorders and related negative valence system processes in children. Participants were 398 pairs of twin children aged 9 to 13 recruited from the Mid-Atlantic Twin Registry.25 The sample was limited to Caucasians to provide sufficient power for genetic analyses by reducing genetic variance due to ancestral diversity. Twenty-two (4.1%) participants were removed who consistently rated 0 distress but discontinued the task early due to distress. Task response modeling was conducted on data from the remaining 516 participants; 505 (97.9%) completed self-report questionnaires on paper or via REDCap hosted at VCU26 and were included in analyses of the association of class membership with clinical correlates. This research was conducted at and approved by the institutional review boards of VCU and the National Institute of Mental Health (NIMH) Intramural Research Program (IRP). Participants’ parent or legal guardian provided informed consent, and participants provided informed assent before participating.
A study psychiatrist or psychologist completed the structured Kiddie Schedule for Affective Disorders and Schizophrenia assessment27 via parent interview. The sample was generally representative of children in this age group for internalizing disorders as indicated by lifetime prevalence rates consistent with prior epidemiological studies: any depressive disorder (2.2%)28; any anxiety disorder (27.4%).29
Measures
Clinical Symptomatology
Symptoms of pediatric anxiety disorders (panic disorder, generalized anxiety disorder, separation anxiety disorder, and social anxiety disorder) were assessed by the Screen for Child Anxiety Related Disorders – child version (SCARED). Strong psychometric reliability and validity have been demonstrated in child samples,30 including within the present sample.24 The severity of depressive symptoms was assessed by the Short Mood and Feelings Questionnaire (SMFQ), which assesses 13 symptoms,31 also with sound psychometrics,31,32 including within the present sample.24
Clinically-Relevant Traits
Anxiety sensitivity was assessed by the Child Anxiety Sensitivity Index (CASI).33 Irritability over the past 6 months was assessed by the Affective Reactivity Index (ARI).34 Extraversion and neuroticism were assessed by respective scales of the Junior Eysenck Personality Questionnaire-Revised. Behavioral activation and inhibition were assessed by the Behavioral Activation System/Behavioral Inhibition System (BIS/BAS) scales.35 These measures have all demonstrated strong psychometrics in prior child samples and in the present study.24
Task-Specific Assessment
Anxious distress during the CO2 challenge task was assessed at 2-minute intervals for the 18-minute duration of the task. Participants indicated their distress on a subjective units of distress scale (SUDS)36 from 0 (none) to 8 (extreme). Additionally, tolerance of distress during the CO2 challenge task was indexed by whether participants terminated participation in the task prematurely. Validity of premature termination from the CO2 task as a marker of distress tolerance has been previously established.22,37
Participant experiences of 13 clinical panic symptoms during the CO2 challenge task were assessed by self-report on the Diagnostic Symptom Questionnaire (DSQ)38 at 4 points during the procedure: prior to putting on the facemask, prior to initiation of CO2-enriched air, 5 minutes after initiation of CO2-enriched air, and at the end of the task before removing the facemask. A participant was determined to have experienced a panic-like state if, at any assessment, they reported the cognitive experience of panic and at least 4 of 13 symptoms at a 4 or 5 out of 5 intensity.
Procedure
The CO2 challenge task followed the procedure previously described by Roberson-Nay et al.23 While concentrations of CO2 vary across CO2 tasks, lower concentrations are more frequently used with child and adolescent samples (4–8%)14 and allow for a more fine-grained measure of the more gradual resulting response.2 Participants were informed that the task would last 18 minutes during which time they would breathe ambient room air that would be enriched to 7.5% CO2 and then revert to unenriched ambient room air. To minimize potential expectancy effects, participants were not told when CO2 enrichment would begin. Participants were reminded that they could terminate the task if it became too uncomfortable.
During the task, participants breathed through a silicone face mask (Hans Rudolph, Inc.), which covered their nose and mouth. This was connected, via gas impermeable tubing, to a multi-liter bag (Hans Rudolph, Inc.), which contained air enriched to 7.5% CO2. During the 5-minute baseline period, participants breathed ambient room air through the mask. After 5 minutes, a research assistant administered the DSQ items (see above) and then turned a three-way stopcock valve (Hans Rudolph, Inc.) to initiate the flow of CO2-enriched air. A research assistant was present in the room for the duration of the task. Participants breathed CO2-enriched air for 8 minutes, after which time the research assistant turned the valve again to revert the participant back to breathing ambient room air. Participants rated pre-task distress prior to putting on the face mask.
Data Analysis
LGMM evaluated whether inter-individual heterogeneity in response may be due to distinct classes of participant trajectories of distress over the course of the task.39 Unlike those that include only peak distress or slope of response, this approach analyzes the latent growth curve for each participant to characterize the temporal unfolding of individual responses. The time point prior to fitting the mask was used as a baseline on which to compare the resulting classes. The first two recordings following initiation of the task were averaged to obtain a pre-CO2 baseline. The final time point (i.e. minute 18) was removed due to suspected multicollinearity with the previous time points. Age was included as a covariate in the models to examine age-related changes in CO2 hypersensitivity. Similar class proportions and trajectories for each class remain when this covariate is excluded.
LGMMs were estimated for 1, 2, 3, 4, and 5 classes to identify the optimal number. The present study followed Eaves et al.’s approach to estimating latent class models (e.g., LGMMs) with clustered data.40 Participants were considered as individuals and nesting within families is accounted for in subsequent analyses based on class membership. Models were compared on entropy, Baysian Information Criterion (BIC), sample size-adjusted BIC (SABIC), and the Lo-Mendell Rubin Test (LMR-LRT), which compares a given model to a nested model 1 fewer classes. As recommended, the LMR-LRT provided the primary indicator of whether an additional class significantly improved model fit.41 Models were then further evaluated based on BIC and SABIC. LGMMs were run in Mplus version 7.42
Each clinical correlate and two traditional indicators of CO2 hypersensitivity, experience of a panic-like event and premature discontinuation, was regressed on class membership to demonstrate predictive validity of CO2 hypersensitivity.43 Additionally, experience of a panic-like event and participant sex were added as covariates to evaluate whether latent class was associated with clinical correlates beyond panic-like experiences during the task and potential sex differences in clinical correlates. Empirical results are presented, and interpretation of results considered multiple comparisons, particularly between classes. However, multiple clinical covariates (e.g., neuroticism, GAD symptoms, and depression symptoms) are correlated and represent overlapping measures to test specific hypotheses with greater validity.44 To our knowledge, existing adjustments for multiple comparisons of highly correlated measures are not amenable to nonindependent data.45 Instead, multiple comparisons were considered in interpreting results. Regressions were computed using mixed effects (i.e., multilevel) linear and logistic regression for continuous and dichotomous correlates, respectively, to account for participant non-independence. Therefore, confidence intervals are provided but standardized estimates of regression paths are not interpretable. Regression analyses and plotting were completed using R version 3.2.346 with lme4,47 pbkrtest,48 psych,49 and ggplot2.50
RESULTS
LGMM of Distress During CO2 Challenge
Table 1 lists the fit indices for the 1, 2, 3, 4, and 5 class LGMMs. The LMR and VLMR tests indicated that the 3-class model provided the best fit. Moreover, BIC and SABIC indicate improved fit of the 3-class model over the 2-class model while entropy remained high (0.785), which suggests that participants are classified into distinct classes.43
Table 1.
Fit and Parameters for Latent Growth Mixture Models
| # of classes | # of parameters | BIC | SABIC | −2LL | VLMR -2LL Difference | VLMR p-value | LMR -2LL Difference | LMR p-value | Entropy |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 18 | 9172.78 | 9115.64 | −4530.26 | -- | -- | -- | -- | -- |
| 2 | 23 | 9150.85 | 9077.85 | −4503.71 | 53.11 | .0002 | 51.46 | .0003 | 0.742 |
| 3 | 28 | 9124.60 | 9035.72 | −4474.99 | 59.09 | .0003 | 57.25 | .0003 | 0.785 |
| 4 | 33 | 9114.44 | 9009.70 | −4454.32 | 41.34 | .044 | 40.05 | .048 | 0.823 |
| 5 | 38 | 9044.11 | 8923.49 | −4403.56 | 42.15 | .438 | 40.84 | .447 | 0.924 |
Note. Boldface data reflect the best-fitting model based on fit criteria described earlier in the article. −2LL = −2 log likelihood; BIC = Bayesian Information Criteria; LMR = Lo-Mendell-Rubin Adjusted Likelihood Ratio Test; SABIC = Sample-Size Adjusted BIC; VLMR = Vuong-Lo-Mendell-Rubin Likelihood Ratio Test.
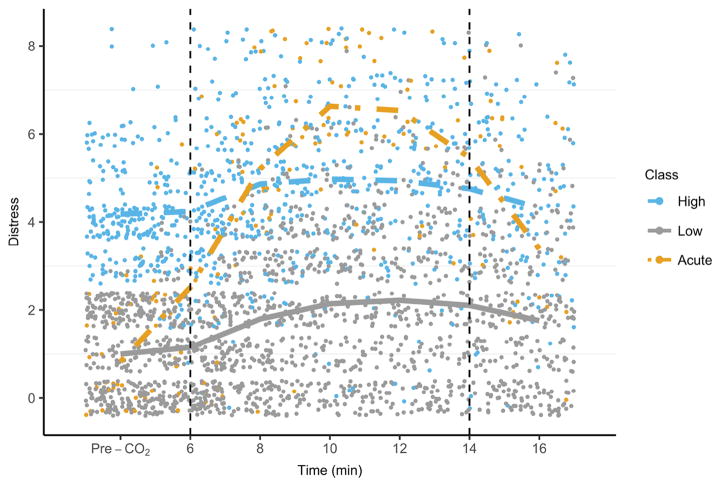
Participants in all three classes evidenced increased distress when breathing CO2-enriched air, which decreased when breathing ambient room air (see Figure 1). Across classes, older age was associated with a greater increase in distress when breathing CO2-enriched air (B=0.09, p=.001, βacute=0.19, βhigh=0.18, βlow=0.21), and subsequent decrease when breathing ambient room air (B=−0.02, p=.001, βacute=−0.23, βhigh=−0.22, βlow=−0.25). The predominant class (i.e. low) included 298 children (59% of the sample); these participants manifested a low intercept and modest increase in distress (see Table 2). The second largest group (i.e., high) included 176 children (34.9% of the sample) with a similar, modest increase in distress despite an overall higher level of distress. Finally, the third group (i.e. acute) included 31 children (6.1% of the sample) who reported initially low levels of distress but responded to the task with a sharp increase. Like other classes, participants in this acute class reported that increased distress abated by the end of the task (see Figure 1). Mean participant age did not differ among the low (M=11.32, SD=1.59), acute (M=10.90, SD=1.51), and high classes (M=11.26, SD=1.42). Similarly, the proportion of female participants did not differ among the low (n = 167; 58.4%), acute (n = 14; 46.7%), and high classes (n = 87; 51.2%), χ2 (2) = 3.17, p = .20. Finally, the proportion of individual monozygotic twins did not differ among the low (n = 97, 37.9%), acute (n = 8, 30.8%), and high classes (n = 60, 38.2%), χ2 (2) = 0.55, p = .76.
Figure 1.
Distress over time by class
Table 2.
Descriptive Statistics and Comparison for Latent Classes and Dimensional Correlates
|
|
||||||
|---|---|---|---|---|---|---|
| Low Class | Acute Class | High Class | Acute vs. Low | High vs. Low | Acute vs. High | |
|
| ||||||
| Variable | Mean (SD) | Mean (SD) | Mean (SD) | B (95% CI) | B (95% CI) | B (95% CI) |
| Panic symptoms | 4.76 (3.62) | 5.88 (3.92) | 5.87 (3.59) | 0.67 (−0.63, 1.98) | 0.82 (0.17, 1.46) * | −0.14 (−1.46, 1.18) |
| GAD symptoms | 5.26 (3.38) | 6.61 (3.50) | 7.11 (3.93) | 0.51 (−0.80, 1.82) | 1.50 (0.85, 2.15) + | −1.00 (−2.32, 0.33) |
| Separation anxiety | 4.68 (3.26) | 5.64 (3.73) | 5.90 (3.48) | 0.97 (−0.22, 2.16) | 0.98 (0.40, 1.57) *** | −0.01 (−1.22, 1.19) |
| Social anxiety | 5.87 (3.16) | 5.61 (2.68) | 6.51 (3.29) | −0.55 (−1.75, 0.64) | 0.47 (−0.12, 1.07) | −1.02 (−2.23, 0.19) |
| Fearfulness | 0.63 (0.32) | 0.67 (0.34) | 0.79 (0.32) | 0 (−0.12, 0.12) | 0.14 (0.08, 0.20) + | −0.14 (−0.26, −0.02) * |
| Extraversion | 17.59 (4.20) | 17.25 (3.73) | 17.12 (4.23) | 0.14 (−1.42, 1.69) | −0.16 (−0.93, 0.60) | 0.30 (−1.28, 1.88) |
| Neuroticism | 7.77 (4.55) | 8.96 (4.04) | 10.07 (4.82) | 0.83 (−0.89, 2.55) | 2.14 (1.30, 2.99) + | −1.31 (−3.06, 0.43) |
| Behavioral activation | 19.22 (5.98) | 19.74 (5.96) | 19.99 (5.70) | −0.21 (−2.50, 2.09) | 0.68 (−0.45, 1.82) | −0.89 (−3.23, 1.45) |
| Behavioral inhibition | 8.52 (3.96) | 8.51 (3.62) | 10.30 (4.02) | −0.84 (−2.31, 0.63) | 1.66 (0.94, 2.37) + | −2.49 (−3.97, −1.01) *** |
| Anxiety sensitivity | 9.57 (5.47) | 10.66 (5.15) | 12.27 (6.24) | −0.40 (−2.44, 1.66) | 2.27 (1.27, 3.28) + | −2.67 (−4.73, −0.60) ** |
| Irritability | 2.50 (2.45) | 4.03 (3.06) | 3.57 (2.80) | 1.35 (0.38, 2.31) ** | 0.90 (0.42, 1.38) *** | 0.45 (−0.53, 1.43) |
| Depression | 4.79 (3.89) | 5.90 (4.08) | 6.06 (4.09) | 0.89 (−0.53, 2.31) | 1.17 (0.46, 1.87) ** | −0.27 (−1.72, 1.17) |
Note. Estimates were derived from a model that adjusted for the experience of a panic-like event; results are unchanged without this adjustment. GAD = generalized anxiety disorder.
p ≤ .05,
p ≤ .01,
p ≤ .001,
p ≤ .0001.
Association of Latent Classes With Clinical Correlates
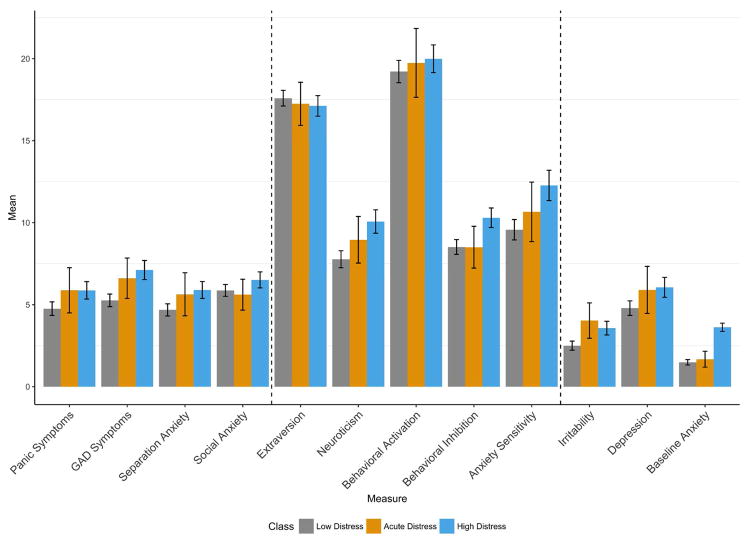
Compared to the low class, participants in the high class reported elevated neuroticism, behavioral inhibition, anxiety sensitivity, fearfulness, irritability, and symptoms of panic, generalized anxiety, separation anxiety, and depression (see Table 2, Figure 2, and Figure S1, available online). Also, compared to participants in the low class, those in the high class reported elevated pre-task distress and were more likely to experience a panic-like state during the task and to terminate the task prematurely (see Table 3). Although the small size of the acute class limits statistical power, comparisons against the low class suggest that the acute class may be a risk factor for internalizing psychopathology, specifically phasic responses such as irritability (see Table 2 and Figure 2). Additionally, as hypothesized, participants in the acute class experienced a panic-like state during the task at a much higher rate than participants in the low class (OR=16.25), while the acute and low classes did not differ regarding pre-task distress or task dropout rate.
Figure 2.
Bar graph of class means for clinical correlates. Note: GAD = generalized anxiety disorder.
Table 3.
Descriptive Statistics and Comparison for Latent Classes and Behavioral Correlates
|
|
||||||
|---|---|---|---|---|---|---|
| Low Class | Acute Class | High Class | Acute vs. Low | High vs. Low | Acute vs. High | |
|
| ||||||
| Variable | Mean (SD) | Mean (SD) | Mean (SD) | B (95% CI) | B (95% CI) | B (95% CI) |
| Baseline distressa | 1.49 (1.45) | 1.68 (1.38) | 3.62 (1.71) | 0.06 (−0.53, 0.64) | 2.04 (1.75, 2.33) + | −1.98 (−2.58, −1.39) + |
|
|
||||||
| n (%) | n (%) | n (%) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
|
|
||||||
| Panic-like experience during taskb | 8 (2.69) | 7 (22.58) | 18 (10.34) | 16.25 (4.07, 101.50) *** | 4.54 (1.78, 14.27) ** | 3.58 (1.01, 16.33) |
| Early terminationa | 109 (36.70) | 17 (54.84) | 94 (53.71) | 1.91 (0.59, 6.00) | 2.49 (1.40, 4.57) ** | 0.77 (0.23, 2.44) |
Note. Percentages correspond to participants positive within each class.
Estimates were derived from a model that adjusted for participant sex and the experience of a panic-like event; results are unchanged without this adjustment.
Estimates were derived from a model that adjusted for participant sex; results are unchanged without this adjustment.
p ≤ .05,
p ≤ .01,
p ≤ .001,
p ≤ .0001.
The experience of a panic-like event was associated with recent elevated symptoms of panic, GAD, separation anxiety, and depression, as well as elevated neuroticism, anxiety sensitivity, behavioral activation, behavioral inhibition, fearfulness, irritability, and baseline distress despite no association with terminating the task early (see Table S1, available online). Similarly, female participants reported higher symptoms of panic, GAD, separation anxiety, and social anxiety, as well as higher neuroticism, anxiety sensitivity, behavioral inhibition, and fearfulness despite no association with risk of experiencing a panic-like event or terminating the task early (see Table S2, available online). Results regarding the association of latent classes with clinical correlates were unchanged following adjustment for participant sex and whether the participant experienced a panic-like event. Additionally, most results regarding the association of latent classes with clinical correlates (see Table 2) are significant below the most restrictive Bonferroni-corrected alpha for 45 comparisons (i.e., α ≥ 0.0011), which is overly restrictive due to conceptual and empirical overlap between clinical correlates (e.g., GAD and depression symptoms).44
DISCUSSION
We addressed three questions regarding CO2 hypersensitivity in children. First, are temporal response patterns similar to those seen in adolescents and adults? Second, how does CO2 hypersensitivity relate to clinical anxiety measures in children, particularly panic and separation anxiety, as has been seen previously? Third, do these relationships extend beyond anxiety to a broader set of pediatric internalizing phenotypes, such as related traits (e.g., anxiety sensitivity, irritability) and depression symptomatology? We will review the results of these investigations in turn.
Inter-individual heterogeneity in children’s distress trajectories during the 7.5% CO2 challenge task resulted from a mixture of three distinct classes of participants (Figure 1). As expected, overall distress increased for participants in all three classes. However, one class remained consistently low in distress and another consistently high. Both exhibited only a modest mean increase while breathing the CO2 mixture. The third class started at the same baseline as the low class but displayed an acute increase in distress to a peak approximately as high as the high class. This 3-class pattern of response is consistent with two prior investigations of CO2 hypersensitivity in young adult and adolescent samples.22,23 However, the proportions of class membership differed substantially between this younger sample and prior studies in adolescents and young adults. In prior studies, the low class was the largest (74%), the acute class intermediate (14–20%), and the high class smallest (6–10%). Remarkably, in this younger sample, almost 35% of participants were in the high class while only 6% of participants were in the acute class.
These findings are consistent with shifts in the prevalence of specific anxiety disorders from childhood to adolescence.19 Hence, the CO2 challenge task might provide unique sensitivity to detecting such developmental changes. Participants in the prior studies had already passed through puberty, the time during which internalizing risk increases sharply, which might contribute to membership in the acute class. Consistent with this proposition and with previous studies, we found that older participant age was associated with greater distress response within each class, though age was not associated with greater likelihood of membership in the acute class per se.
We next examined the relationship between these classes and individual differences in a wide variety of symptoms of anxiety and depression as well as dimensional traits that may serve as internalizing risk markers. Several overall patterns emerge (Table 2, Figure 2, and Figure S1, available online), which are similar to prior investigations in adolescent22 and young adult samples.23 First, elevated symptoms of panic, separation anxiety, generalized anxiety, depression, and irritability are seen in the high class compared to the low class. These depict a set of broad clinical correlates that are marked by responsivity to stress for children who report consistently elevated anxiety. In contrast, social anxiety symptoms, which are more stable, chronic, and less relevant to this physiological challenge task, are not elevated in any group of task respondents. This is consistent with reports from prior studies of children14 and adults.51
Second, compared to the low class, participants in the high class were also elevated on anxious traits such as fearfulness, anxiety sensitivity, behavioral inhibition, and neuroticism. This further demonstrates the broad clinical implications for consistently elevated distress as compared against acute reactivity to physiological challenge or consistently low distress. Third, despite limited power, participants in the acute class were around sixteen times more likely to experience a panic-like event than the low class and around three times more likely than the high class. This suggests that the acute response mirrors a specific, panico-typic response to the task, and, along with evidence of elevated irritability,52 further indicates that the acute class represents a particularly reactive subset of participants who show elevated phasic symptoms (e.g., irritability). This is consistent with one prior investigation of adolescent participants22 that demonstrated elevated transient stress symptoms among participants in the acute class, compared to the low class, despite similar levels of anxiety and depressive symptoms. Additionally, membership in the high class was associated with increased rate of prematurely discontinuing the task, a proposed measure of distress tolerance.37 Finally, divergent validity for LGMM of the CO2 challenge task is evident in the lack of association of class membership with positive valence traits of extraversion or behavioral activation.
Whereas prior research has suggested elevated CO2 sensitivity among anxiety disorders other than panic,14–16 it remains unclear whether CO2 hypersensitivity predicts internalizing disorders, broadly, or anxiety, specifically. Disorder specificity is critical to understanding the developmental course of CO2 hypersensitivity as a risk factor for psychopathology, especially given evidence of multifinality in the development of psychopathology.20 Our findings suggest that, among children, CO2 hypersensitivity disaggregates sustained and acute threat. Whereas sustained threat may be a non-specific biomarker for internalizing symptomatology, acute threat may be specific to panic-related experiences and acute, phasic responses to stress.
The present study should be considered in light of several limitations. Primarily, the VCU-JAS was conducted to examine genetic correlates of negative valence phenotypes.24 To minimize genetic heterogeneity, the sample was restricted to Caucasian twin pairs. Future research is needed to generalize these results to individuals from other ancestral backgrounds, though we know of no evidence suggesting different manifestations or correlates of CO2 hypersensitivity.
Secondly, the present study was conducted with a genetic epidemiological sample of children. As such, participants were not selected based on existing psychopathology, though lifetime prevalence estimates for any depressive or anxiety disorder are similar to those in an age-matched general population sample. Compared to a clinically ascertained sample, a community sample such as VCU-JAS typically has lower severity of internalizing symptoms, making generalization to patient samples uncertain.
Lastly, the present study is an initial investigation of the manifestation, specificity, and internalizing correlates of CO2 hypersensitivity among children. As such, it was conducted on a single occasion, similar to prior research on CO2 hypersensitivity.15,23 However, a developmental perspective on child and adolescent psychopathology would benefit from a longitudinal examination of CO2 hypersensitivity to further identify its role as a prospective risk factor for future illness.
These results have several potential clinical implications. Future longitudinal research might identify distinct roles of chronically elevated and acutely reactive distress as risk factors for the development of internalizing and anxiety disorders, respectively. For example, the distinction between chronically elevated and acutely reactive anxiety may clarify the association of panic attacks with other areas of psychiatric and medical interest (e.g., suicidality).53,54 Finally, if CO2 hypersensitivity is a risk factor for the development of anxiety and internalizing disorders, future genetically informed research of CO2 hypersensitivity may clarify the etiology of pediatric internalizing disorders, especially anxiety, and inform the development of novel treatments for pediatric psychopathology.
In conclusion, the present study extends prior research examining the manifestation of CO2 hypersensitivity in children and demonstrates that child participants could be characterized based on three response groups: overall low, acute, or high distress. Moreover, in comparison to the low class, membership in the high or acute response classes was associated with elevated symptoms of several anxiety disorders and depression while the high class demonstrated additional association with internalizing dimensional traits. These results help clarify the manifestation of CO2 hypersensitivity among children, particularly as it is like that in adolescent and adult participants; they also demonstrate associations of CO2 hypersensitivity with anxiety and depressive disorders that are broadly consistent with research in older individuals.
Supplementary Material
Acknowledgments
Funding: This study was supported by the National Institute of Mental Health (R01MH098055 to J.M.H., NIMH-IRP-ziamh002781 to D.S.P., and T32MH020030 to L.M.R. and C.S.) and by UL1TR000058 from the NCRR.
The authors wish to thank the mid-Atlantic Twin Registry and the families who participated in this study.
Footnotes
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The material contained in this article has not been published elsewhere nor is it under consideration elsewhere. One prior paper, which described the study, is cited in the text; there are no previous publications based on the data regarding the carbon dioxide challenge task.
Supplemental material cited in this article is available online.
Preliminary research findings were presented as an abstract at the annual meeting of the Anxiety and Depression Association of America (ADAA) in San Francisco, CA, April 6–9, 2017.
Disclosures:
Drs. Rappaport, Sheerin, Towbin, Leibenluft, Pine, Brotman, Roberson-Nay, Hettema, and Ms. Carney report no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dr. Lance M. Rappaport, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond.
Dr. Christina Sheerin, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond.
Ms. Dever M. Carney, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond.
Dr. Kenneth E. Towbin, National Institute of Mental Health, Bethesda, MD.
Dr. Ellen Leibenluft, National Institute of Mental Health, Bethesda, MD.
Dr. Daniel S. Pine, National Institute of Mental Health, Bethesda, MD.
Dr. Melissa A. Brotman, National Institute of Mental Health, Bethesda, MD.
Dr. Roxann Roberson-Nay, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond.
Dr. John M. Hettema, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond.
References
- 1.Vickers K, Jafarpour S, Mofidi A, Rafat B, Woznica A. The 35% carbon dioxide test in stress and panic research: overview of effects and integration on findings. Clin Psychol Rev. 2012;32:153–164. doi: 10.1016/j.cpr.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 2.Zvolensky MJ, Eifert GH. A review of psychological factors/processes affecting anxious responding during voluntary hyperventilation and inhalations of carbon dioxide-enriched air. Clin Psychol Rev. 2001;21:375–400. doi: 10.1016/s0272-7358(99)00053-7. [DOI] [PubMed] [Google Scholar]
- 3.Battaglia M, Pesenti-Gritti P, Medland SE, Ogliari A, Tambs K, Spatola CA. A genetically informed study of the association between childhood separation anxiety, sensitivity to CO2, panic disorder, and the effect of childhood parental loss. Arch Gen Psychiatry. 2009;66:64–71. doi: 10.1001/archgenpsychiatry.2008.513. [DOI] [PubMed] [Google Scholar]
- 4.Battaglia M, Pesenti-Gritti P, Spatola CA, Ogliari A, Tambs K. A twin study of the common vulnerability between heightened sensitivity to hypercapnia and panic disorder. Am J Med Genet B Neuropsychiatr Genet. 2008;147b:586–593. doi: 10.1002/ajmg.b.30647. [DOI] [PubMed] [Google Scholar]
- 5.Rassovsky Y, Kushner MG. Carbon dioxide in the study of panic disorder: issues of definition, methodology, and outcome. J Anxiety Disord. 2003;17:1–32. doi: 10.1016/s0887-6185(02)00181-0. [DOI] [PubMed] [Google Scholar]
- 6.Schmidt NB, Maner JK, Zvolensky MJ. Reactivity to challenge with carbon dioxide as a prospective predictor of panic attacks. Psychiatry Res. 2007;151:173–176. doi: 10.1016/j.psychres.2006.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Telch MJ, Harrington PJ, Smits JAJ, Powers MB. Unexpected arousal, anxiety sensitivity, and their interaction on CO2-induced panic: Further evidence for the context-sensitivity vulnerability model. J Anxiety Disord. 2011;25:645–653. doi: 10.1016/j.janxdis.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 8.Coryell W, Fyer A, Pine DS, Martinez JM, Arndt S. Aberrant respiratory sensitivity to CO2 as a trait of familial panic disorder. Biol Psychiatry. 2001;49:582–587. doi: 10.1016/s0006-3223(00)01089-1. [DOI] [PubMed] [Google Scholar]
- 9.van Beek N, Griez E. Reactivity to a 35% CO2 challenge in healthy first-degree relatives of patients with panic disorder. Biol Psychiatry. 2000;47:830–835. doi: 10.1016/s0006-3223(99)00265-6. [DOI] [PubMed] [Google Scholar]
- 10.Gorman JM, Papp LA, Martinez JM, et al. High-dose carbon dioxide challenge test in anxiety disorder patients. Biol Psychiatry. 1990;28:743–757. doi: 10.1016/0006-3223(90)90510-9. [DOI] [PubMed] [Google Scholar]
- 11.Verberg K, Griez E, Meijer J, Pols H. Discrimination between panic disorder and generalized anxiety disorder by 35% carbon dioxide challenge. Am J Psychiatry. 1995;152:1081–1083. doi: 10.1176/ajp.152.7.1081. [DOI] [PubMed] [Google Scholar]
- 12.Muhtz C, Yassouridis A, Daneshi J, Braun M, Kellner M. Acute panicogenic, anxiogenic and dissociative effects of carbon dioxide inhalation in patients with post-traumatic stress disorder (PTSD) J Psychiatr Res. 2011;45:989–993. doi: 10.1016/j.jpsychires.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 13.Coplan JD, Moreau D, Chaput F, et al. Salivary cortisol concentrations before and after carbon-dioxide inhalations in children. Biol Psychiatry. 2002;51:326–333. doi: 10.1016/s0006-3223(01)01250-1. [DOI] [PubMed] [Google Scholar]
- 14.Pine DS, Klein RG, Coplan JD, et al. Differential carbon dioxide sensitivity in childhood anxiety disorders and nonill comparison group. Arch Gen Psychiatry. 2000;57:960–967. doi: 10.1001/archpsyc.57.10.960. [DOI] [PubMed] [Google Scholar]
- 15.Pine DS, Klein RG, Roberson-Nay R, et al. Response to 5% carbon dioxide in children and adolescents: relationship to panic disorder in parents and anxiety disorders in subjects. Arch Gen Psychiatry. 2005;62(1):73–80. doi: 10.1001/archpsyc.62.1.73. [DOI] [PubMed] [Google Scholar]
- 16.Roberson-Nay R, Klein DF, Klein RG, et al. Carbon dioxide hypersensitivity in separation-anxious offspring of parents with panic disorder. Biol Psychiatry. 2010;67:1171–1177. doi: 10.1016/j.biopsych.2009.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Perna G, Ieva A, Caldirola D, Bertani A, Bellodi L. Respiration in children at risk for panic disorder. Arch Gen Psychiatry. 2002;59:185–186. doi: 10.1001/archpsyc.59.2.185. [DOI] [PubMed] [Google Scholar]
- 18.Merikangas KR, He J, Burstein M, et al. Lifetime Prevalence of Mental Disorders in U.S. Adolescents: Results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pine DS, Fox NA. Childhood antecedents and risk for adult mental disorders. Annu Rev Psychol. 2015;66:459–485. doi: 10.1146/annurev-psych-010814-015038. [DOI] [PubMed] [Google Scholar]
- 20.Nelemans SA, Hale WW, Branje SJ, et al. Heterogeneity in development of adolescent anxiety disorder symptoms in an 8-year longitudinal community study. Dev Psychopathol. 2014;26:181–202. doi: 10.1017/S0954579413000503. [DOI] [PubMed] [Google Scholar]
- 21.Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V. Psychiatr Clin North Am. 2009;32:483–524. doi: 10.1016/j.psc.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rappaport LM, Sheerin C, Savage JE, Hettema JM, Roberson-Nay R. Clinical correlates of latent classes of CO2 hypersensitivity over time in adolescents and young adults. Behav Res Ther. 2017;93:95–103. doi: 10.1016/j.brat.2017.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roberson-Nay R, Beadel JR, Gorlin EI, Latendresse SJ, Teachman BA. Examining the latent class structure of CO2 hypersensitivity using time course trajectories of panic response systems. J Behav Ther Exp Psychiatry. 2015;47:68–76. doi: 10.1016/j.jbtep.2014.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carney DM, Moroney E, Machlin L, et al. The twin study of negative valence emotional constructs. Twin Res Hum Genet. 2016;19:456–464. doi: 10.1017/thg.2016.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lilley EC, Silberg JL. The mid-Atlantic twin registry, revisited. Twin Res Hum Genet. 2013;16:424–428. doi: 10.1017/thg.2012.125. [DOI] [PubMed] [Google Scholar]
- 26.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kaufman J, Birmaher B, Brent D, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 28.Fergusson DM, Horwood J, Lynskey MT. Prevalence and comorbidity of DSM-III-R diagnoses in a birth cohort of 15 year olds. J Am Acad Child Adolesc Psychiatry. 1993;32:1127–1134. doi: 10.1097/00004583-199311000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Costello EJ, Egger HL, Angold A. The developmental epidemiology of anxiety disorders: Phenomenology, prevalence, and comorbidity. Child Adolesc Psychiatr Clin N Am. 2005;14:631–648. doi: 10.1016/j.chc.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 30.Birmaher B, Khetarpal S, Brent D, et al. The screen for child anxiety related emotional disorders (SCARED): Scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry. 1997;36:545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- 31.Angold A, Costello EJ, Messer SC, Pickles A, Winder F, Silver D. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. Int J Methods Psychiatr Res. 1995;5:237–249. [Google Scholar]
- 32.Klein DN, Dougherty LR, Olino TM. Toward guidelines for evidence-based assessment of depression in children and adolescents. J Clin Child Adolesc Psychol. 2005;34:412–432. doi: 10.1207/s15374424jccp3403_3. [DOI] [PubMed] [Google Scholar]
- 33.Silverman WK, Fleisig W, Rabian B, Peterson RA. Childhood anxiety sensitivity index. J Clin Child Psychol. 1991;20:162–168. [Google Scholar]
- 34.Stringaris A, Goodman R, Ferdinando S, et al. The Affective Reactivity Index: a concise irritability scale for clinical and research settings. J Child Psychol Psychiatry. 2012;53:1109–1117. doi: 10.1111/j.1469-7610.2012.02561.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carver CS, White TL. Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: The BIS/BAS scales. J Pers Soc Psychol. 1994;67:319–333. [Google Scholar]
- 36.Wolpe J. The Practice of Behavior Therapy. New York: Pergamon Press; 1969. [Google Scholar]
- 37.Leyro TM, Zvolensky MJ, Bernstein A. Distress tolerance and psychopathological symptoms and disorders: A review of the empirical literature among adults. Psychol Bull. 2010;136:576–600. doi: 10.1037/a0019712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sanderson WC, Rapee RM, Barlow DH. The influence of an illusion of control on panic attacks induced via inhalation of 5.5% carbon dioxide-enriched air. Arch Gen Psychiatry. 1989;46:157–162. doi: 10.1001/archpsyc.1989.01810020059010. [DOI] [PubMed] [Google Scholar]
- 39.Lubke GH, Muthén BO. Investigating population heterogeneity with factor mixture models. Psychol Methods. 2005;10:21–39. doi: 10.1037/1082-989X.10.1.21. [DOI] [PubMed] [Google Scholar]
- 40.Eaves LJ, Silberg JL, Hewitt JK, et al. Analyzing twin resemblance in multisymptom data: Genetic applications of a latent class model for symptoms of conduct disorder in juvenile boys. Behav Genet. 1993;23:5–19. doi: 10.1007/BF01067550. [DOI] [PubMed] [Google Scholar]
- 41.Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A monte carlo simulation study. Struct Equ Model Multidiscip J. 2007;14:535–569. [Google Scholar]
- 42.Muthén BO, Muthén LK. Mplus User’s Guide. 8. Los Angeles, CA: Muthén and Muthén; 1998. [Google Scholar]
- 43.Clark SL, Muthén BO. [Accessed September 19, 2017];Relating Latent Class Analysis Results to Variables Not Included in the Analysis. 2009 Retrieved from https://www.statmodel.com/download/relatinglca.pdf.
- 44.Ryan TA. Multiple comparison in psychological research. Psychol Bull. 1959;56:26. doi: 10.1037/h0042478. [DOI] [PubMed] [Google Scholar]
- 45.Blakesley RE, Mazumdar S, Dew MA, et al. Comparisons of methods for multiple hypothesis testing in neuropsychological research. Neuropsychology. 2009;23:255–264. doi: 10.1037/a0012850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: 2015. [Accessed September 18, 2017]. https://www.R-project.org/ [Google Scholar]
- 47.Bates D, Machler M, Bolker B, Walker S. Fitting linear mixed-effects models using {lme4} J Stat Softw. 2015;67:1–48. [Google Scholar]
- 48.Halekoh U, Hojsgaard S. A kenward-roger approximation and parametric bootstrap methods for tests in linear mixed models -- The {R} package {pbkrtest} J Stat Softw. 2014;59:1–30. [Google Scholar]
- 49.Revelle W. Psych: Procedures for Personality and Psychological Research. Evanston, Illinois: Northwestern University; 2015. [Accessed September 18, 2017]. http://CRAN.R-project.org/package=psych. [Google Scholar]
- 50.Wickham H. ggplot2: Elegant Graphics for Data Analysis. New York: Springer-Verlag; 2009. [Google Scholar]
- 51.Schutters SI, Viechtbauer W, Knuts IJ, Griez EJ, Schruers KR. 35% CO2 sensitivity in social anxiety disorder. J Psychopharmacol (Oxf) 2012;26:479–486. doi: 10.1177/0269881111430750. [DOI] [PubMed] [Google Scholar]
- 52.Vidal-Ribas P, Brotman MA, Valdivieso I, Leibenluft E, Stringaris A. The status of irritability in psychiatry: a conceptual and quantitative review. J Am Acad Child Adolesc Psychiatry. 2016;55:556–570. doi: 10.1016/j.jaac.2016.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rappaport LM, Moskowitz DS, Galynker I, Yaseen ZS. Panic symptom clusters differentially predict suicide ideation and attempt. Compr Psychiatry. 2014;55:762–769. doi: 10.1016/j.comppsych.2013.10.017. [DOI] [PubMed] [Google Scholar]
- 54.Roberson-Nay R, Latendresse SJ, Kendler KS. A latent class approach to the external validation of respiratory and non-respiratory panic subtypes. Psychol Med. 2012;42:461–74. doi: 10.1017/S0033291711001425. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.