Figure 1. Workflow for Electrophysiology-Guided, Noninvasive Cardiac Radioablation.
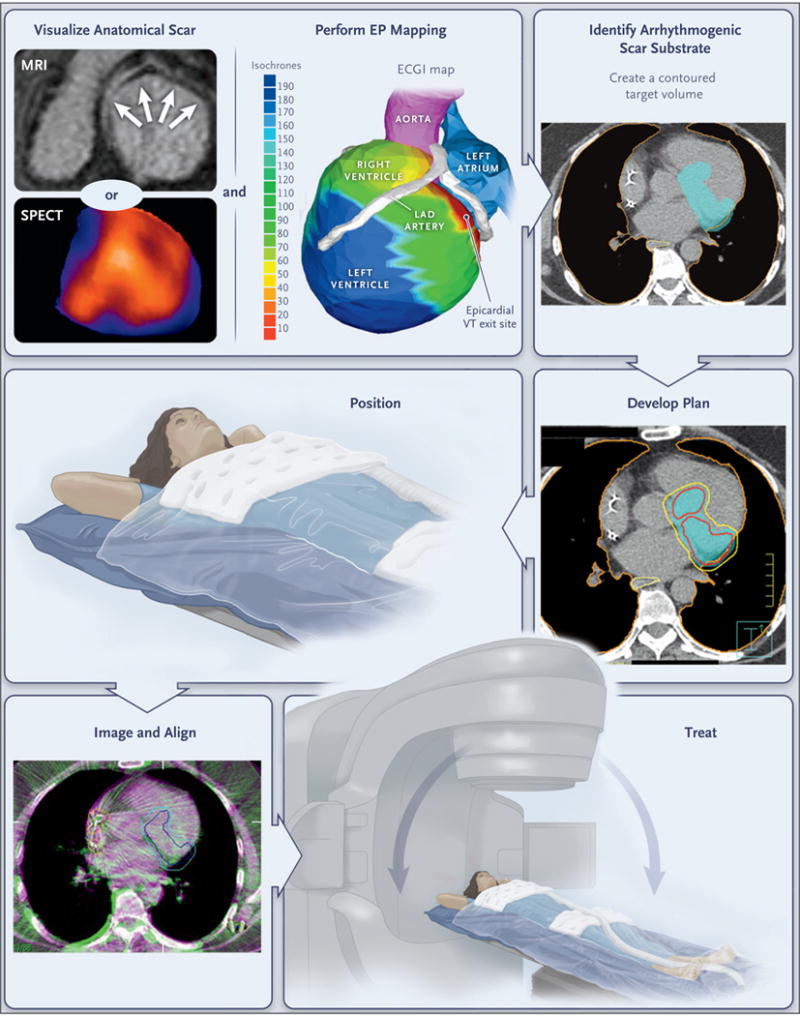
Patients undergo noninvasive visualization of the ventricular scar by means of MRI, CT, single-photon emission CT (SPECT), or a combination of methods, according to clinical routine. The zone of scarring is indicated by arrows on MRI and by blue regions on SPECT, including the base, inferior wall, and apex. Noninvasive electrophysiologic (EP) mapping is performed with electrocardiographic imaging (ECGI) of induced ventricular tachycardia (VT) with programed stimulation from the indwelling implantable cardioverter–defibrillator. The color scale shows the range of activation times of each area of the ventricular wall (isochrones), ranging from 10 msec (red) to 190 msec (deep blue) from the onset of VT activation. The electrophysiologist develops an ablation volume by targeting the full thickness of the ventricular wall harboring the first 10 msec of VT activation (the “exit site”) and the colocalized ventricular scar. (Details regarding scar imaging, EP mapping, and image fusion to develop the ablation volume are provided in the Supplementary Appendix.) The target volume is shown in light blue in the figure panel showing the arrhythmogenic scar substrate. This volume is transferred by the radiation oncologist onto a respiratory-correlated, four-dimensional CT scan, which allows an assessment of the total cardiac and pulmonary motion. In this example, a dose of 25 Gy in a single fraction is prescribed for delivery to the enhanced treatment volume, with a goal of achieving maximal coverage inside the volume while avoiding exposure to the surrounding organs at risk. The target volume is indicated in light blue in the figure panel showing the treatment plan; red and yellow boundaries indicate the distribution of zones projected to receive 2750 cGy and 2375 cGy of radiation, respectively; the lung is outlined in orange, and the yellow boundary behind the heart is the esophagus. If all plans pass standard internal physics quality assurance on a calibrated phantom, the patient is immobilized with the use of a vacuum-assisted device, and stereotactic radioablation is performed by means of an image-guided, radiotherapy-equipped linear accelerator that uses a cone-beam CT to align the radiotherapy treatment beams with the target volume. The dark blue boundary indicates the target, which includes the total cardiac and pulmonary motion. The light blue boundary indicates the target with an additional expansion to account for motion, setup uncertainty, and delivery uncertainty. Treatment is then delivered with the use of the radiotherapy delivery system. LAD denotes left anterior descending.
