Abstract
Purpose
The aim of this prospective pilot study was to compare alveolar ridge preservation (ARP) procedures with open-healing approach using a single-layer and a double-layer coverage with collagen membranes using radiographic and clinical analyses.
Methods
Eleven molars from 9 healthy patients requiring extraction of the maxillary or mandibular posterior teeth were included and allocated into 2 groups. After tooth extraction, deproteinized bovine bone mineral mixed with 10% collagen was grafted into the socket and covered either with a double-layer of resorbable non-cross-linked collagen membranes (DL group, n=6) or with a single-layer (SL group, n=5). Primary closure was not obtained. Cone-beam computed tomography images were taken immediately after the ARP procedure and after a healing period of 4 months before implant placement. Radiographic measurements were made of the width and height changes of the alveolar ridge.
Results
All sites healed without any complications, and dental implants were placed at all operated sites with acceptable initial stability. The measurements showed that the reductions in width at the level 1 mm apical from the alveolar crest (including the bone graft) were −1.7±0.5 mm in the SL group and −1.8±0.4 mm in the DL group, and the horizontal changes in the other areas were also similar in the DL and SL groups. The reductions in height were also comparable between groups.
Conclusions
Within the limitations of this study, single-layer and double-layer coverage with collagen membranes after ARP failed to show substantial differences in the preservation of horizontal or vertical dimensions or in clinical healing. Thus, both approaches seem to be suitable for open-healing ridge preservation procedures.
Keywords: Alveolar process, Bone regeneration, Cone-beam computed tomography, Tooth extraction
Graphical Abstract
INTRODUCTION
The inevitable life-long atrophic process of the alveolus after tooth extraction has been recognized [1,2]. Schropp et al. [3] demonstrated that the width of the alveolar ridge decreased by 50% in 12 months, with two-thirds of the loss occurring within 3 months. Additionally, the buccal crest has been found to undergo significantly more atrophy than the lingual crest, along with the disappearance of bundle bone [4]. Additionally, Tan et al. [5] reported that the mean horizontal and vertical reduction of the alveolar ridge at 6 months post-extraction was 3.79±0.23 mm and 1.24±0.11 mm, respectively, in their systematic review. This amount of atrophy can prevent clinicians from carrying out ideal restorative treatments, and invasive surgical procedures may be needed to fully restore the missing bony structure.
To prevent the substantial reduction of the alveolar ridge after tooth extraction, the alveolar ridge preservation (ARP) technique has been proposed and utilized for more than 20 years as an effective method of markedly counteracting the reduction of the edentulous ridge [6,7,8]; nonetheless, many methodological considerations still await a consensus, such as the selection of biomaterials, the surgical protocol, and the loading protocol for implants. Among the many issues raised regarding the treatment guidelines of ARP, the necessity of primary closure after ARP has been particularly controversial, as some authors still recommend obtaining primary closure by mobilizing the mucoperiosteal flaps, based on the concept of the guided bone regeneration technique. However, recent studies have reported that the ARP technique can be successfully performed without primary closure and that with the proper utilization of resorbable collagen membranes, exposed ARP sites can show satisfactory healing comparable to that obtained through conventional techniques involving primary closure [9,10,11]. Cardaropoli and Cardaropoli [9] and Mardas et al. [12] have shown similar results with the partial exposure of collagen membranes without primary closure after ARP; moreover, many studies have also been conducted with complete exposure of the collagen membrane coverage after ARP [13,14].
As mentioned above, the ARP technique has shown promising results for reducing the atrophy of the alveolar ridge both in the short term [9,13,15] and the long term [11], even without primary closure. However, collagen membranes undergo degradation when exposed to the oral cavity, and due to their tendency for fast resorption, it has been suspected that collagen membranes may not be able to provide suitable stabilization for bone grafts during the healing period, especially with single coverage. The authors of the present study have previously analyzed the effects of open-healing ARP in clinical, histological, and radiographic aspects in 2 previous studies [16,17]. In those studies, double-layer coverage with resorbable collagen membranes was used to protect the operated sites. The possible advantage of double-layer membrane coverage for guided bone regeneration was first suggested by Buser et al. [18,19]. Then, Kim et al. [20] verified that the double-layer technique showed a statistically significant benefit in comparison to the single-layer technique for maintaining the stability of block-bone grafts and protecting the bone graft from the resorption. Nonetheless, no previous report has explored the quantitative effects of single-layer vs. double-layer coverage with resorbable collagen during open-healing ARP. Therefore, the present authors hypothesized that double-layer coverage of collagen membranes would provide better healing results than single-layer coverage for ARP.
The aim of this randomized prospective pilot study was to compare the effects of ARP using single-membrane coverage with those of double-membrane coverage following ARP procedures after 4 months of healing, using radiographic and clinical analyses.
MATERIALS AND METHODS
Subjects
The inclusion criteria were patients ranging in age from 18 to 65 years old, with the presence of at least 1 periodontally compromised molar with vertical bone loss of less than 50% from the cementoenamel junction in the maxilla or the mandible requiring extraction, with the expectation that it could be replaced with a suitable dental implant. The exclusion criteria were uncontrolled periodontal disease, systemic diseases contraindicating surgical treatment, heavy smoking (>10 cigarettes per day), and pregnancy or lactation.
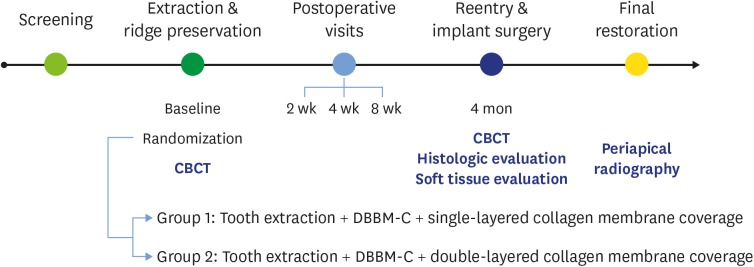
The research protocol (Figure 1) was authorized by the Ethical Committee of Dankook University Dental Hospital, Korea (H-1412/012/002).
Figure 1.
Schematic presentation of the study schedule and design.
CBCT: cone-beam computed tomography, DBBM-C: deproteinized bovine bone mineral with 10% porcine collagen.
Experimental groups
In this randomized prospective pilot trial, a total of 11 molars from 9 healthy patients requiring extraction were included. Eight patients had 1 molar that required extraction, and were randomly allocated into 2 equally sized groups. The other patient had 3 molars requiring extraction; 1 of the 3 molars was allocated to the single-layer membrane (SL) group and the other 2 were allocated to the double-layer membrane (DL) group.
Surgical procedure
Under local anesthesia (2% lidocaine with 1:80,000 epinephrine), the teeth were extracted atraumatically without flap elevation. The interior of the extraction sockets was curetted, and soft tissue remnants were thoroughly removed. The sockets were irrigated with sterile normal saline solution.
After tooth extraction, each extraction site was filled with 250 mg of deproteinized bovine bone matrix mixed with 10% collagen (DBBM-C, Bio-Oss® Collagen, Geistlich Pharma, Wolhusen, Switzerland) up to the highest bone level. After filling the sockets, the sites were randomly assigned to the SL group or the DL group. In the SL group, a single-layer of resorbable collagen membrane (13×25 mm, Bio-Gide®, Geistlich Pharma) was used to cover the operated sites at the level of the adjacent soft tissue. In the DL group, resorbable collagen membrane was trimmed into two pieces and double-layers of resorbable collagen membrane covered the sites. The ‘up’ sides of all the membranes were laid facing the occlusal plane. The membrane was held in place by suture thread (Ethilon 4-0, Ethicon, Cincinnati, OH, USA), using hidden X sutures [16] or X sutures, and secondary healing was obtained. No efforts were made to obtain primary closure. Four months after surgery, the flaps were elevated and non-submerged dental implants (Luna®, Shinhung, Seoul, Korea) were inserted immediately after cone-beam computed tomography (CBCT) re-scanning (Figure 2).
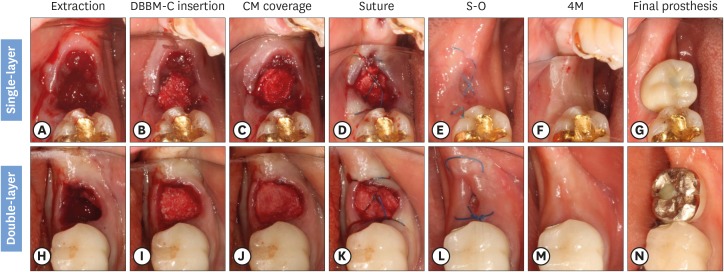
Figure 2.
Surgical procedures of the SL and DL open membrane healing technique. The procedures of the SL and DL groups were only different in the number of the resorbable collagen membranes used to cover the bone graft. (A) Extraction in the SL group. (B) DBBM-C insertion in the SL group. (C) Single-layer of collagen membrane coverage in the SL group. (D) The hidden X or the figure of 8 suture in the SL group. (E) Just before S-O. (F) Four months after extraction, immediately followed by dental implant placement. (G) Occlusal view of the final prosthesis. (H) Extraction in the DL group. (I) DBBM-C insertion in the DL group. (J) Double-layers of collagen membrane coverage in the DL group. (K) The hidden X or the figure of 8 suture in the DL group. (L) Just before S-O. (M) Four months after extraction, immediately followed by dental implant placement in the DL group. (N) Occlusal view of the final prosthesis in the DL group.
SL: the socket was filled with deproteinized bovine bone mineral with 10% collagen and covered by a single-layer of a collagen membrane, DL: the socket was filled with deproteinized bovine bone mineral with 10% collagen and covered by a double-layer of a collagen membrane, DBBM-C: deproteinized bovine bone mineral with 10% porcine collagen, S-O: stitch-out, 4M: 4 months after alveolar ridge preservation procedure.
Radiographic analysis
The CBCT scans were performed with a resolution of 1 mm (scan time of 17 seconds, exposure time of 17 seconds, 80 kV, 7 mA; Alphard 3030, Asahi Roentgen Industries, Kyoto, Japan) 2 times, immediately after ARP and before implant placement (Figure 3). The data were processed in the Digital Imaging and Communications in Medicine format.
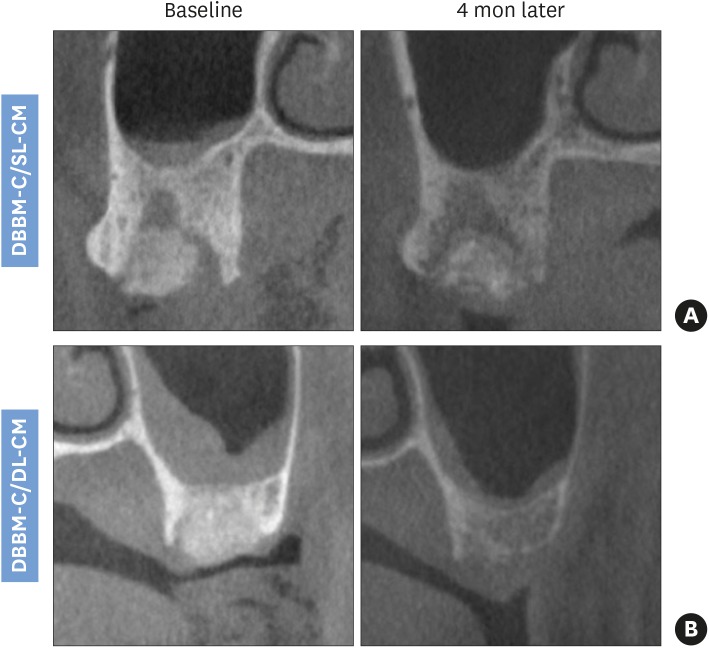
Figure 3.
Paraxial views from CBCT obtained 4 months after SL (A) and DL (B) ARP procedures.
CBCT: cone-beam computed tomography, SL: the socket was filled with deproteinized bovine bone mineral with 10% collagen and covered by a single-layer of a collagen membrane, DL: the socket was filled with deproteinized bovine bone mineral with 10% collagen and covered by a double-layer of a collagen membrane, ARP: alveolar ridge preservation, DBBM-C: deproteinized bovine bone mineral with 10% porcine collagen, CM: collagen membrane.
The CBCT images representing the buccopalatal plane of the fresh extraction sockets and healed sockets were identified and selected using stable reference points (e.g., the palatal vault and the inferior border of the basal bone for the mandible), and 2 corresponding scans were superimposed manually via a computer imaging program (Adobe Photoshop CS6, Adobe Systems, San Jose, CA, USA).
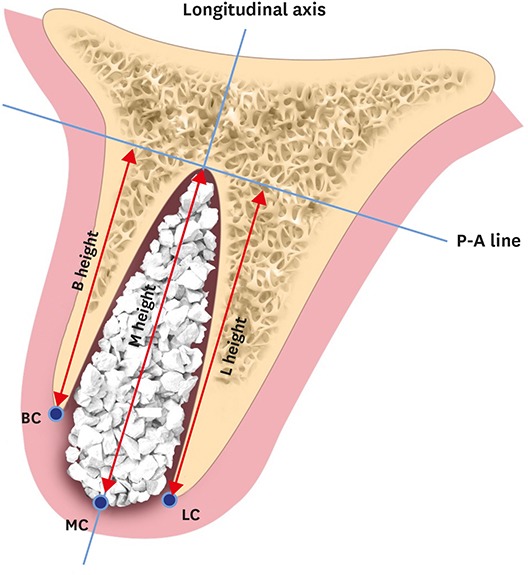
The following landmarks (Figure 4) were identified and the differences between the baseline and after-healing measurements were assessed to calculate the quantitative changes during the healing period. The long axis of the extracted socket was determined by considering the profile of the alveolar ridge, and the perpendicular line to the longitudinal axis at the apex of the socket (P-A line) was identified. The buccal, lingual/palatal, and mid-alveolar ridge crests (BC, PC, and MC lines, respectively) were identified.
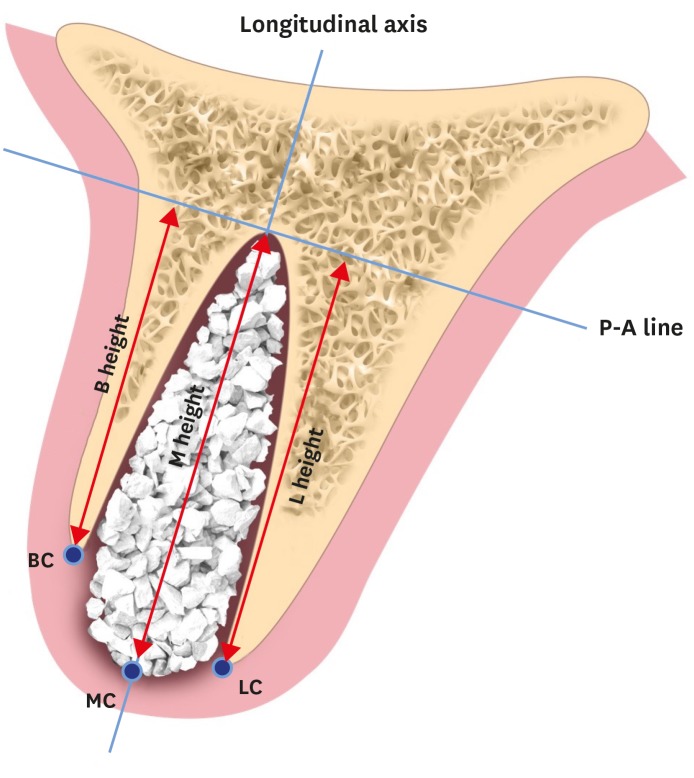
Figure 4.
Schematic drawing of references for measurements in the radiographic analysis. P-A line: perpendicular line to the longitudinal axis at apex of the socket, BC: buccal crest, B height: height of the buccal cortical plate from the P-A line, LC: lingual/palatal crest, L height: height of the lingual/palatal plate from the P-A line, MC: mid-alveolar crest, M height: height of the mid-alveolar crest from the P-A line.
Horizontal width in the 1-, 3-, and 5-mm subcrestal aspects (HW1, HW3, and HW5, respectively); the lines parallel to the P-A line lying 1-, 3-, and 5-mm apically from the MC line (the HW1, HW3, and HW5 lines, respectively) were identified and the distances between the peripheral points of the alveolar bone meeting the HW1, HW3, and HW5 were measured.
Vertical height in the buccal, lingual and middle aspects (BH, LH, and MH, respectively); the vertical distances between the P-A line and BC, LC, and MC (BH, LH, and MH, respectively) were measured.
Statistical analysis
Due to the pilot nature of the present study, a sample size calculation was not performed. All measurement values for each parameter are presented as the mean±standard deviation (SPSS version 21.0, IBM Corp., Armonk, NY, USA).
RESULTS
All sites healed without any complications. No operated area needed an additional bone graft for dental implant placement, and all implants showed satisfactory primary stability at 4 months after ARP. Additionally, the mucosal profile and the width of the keratinized tissue at each site were acceptable for dental implant placement without requiring additional soft tissue augmentation or a free gingival graft. All implants were connected to an abutment 8 weeks after surgery, and single crowns were fabricated following impression making. There was no sign of any pathological state until the final prostheses were delivered.
The measurement values for each parameter in the DL and the SL groups are presented in Tables 1 and 2. The horizontal changes were greater in HW1 (range, 1.2–2.4 mm), followed by HW3 and HW5. HW1, HW3, and HW5 in the SL and the DL groups were similar (−1.7±0.5 vs. −1.8±0.4 for HW1, −1.0±0.5 vs. −0.8±0.5 for HW3, and −0.5±0.2 vs. −0.4±0.3 mm for HW5, respectively).
Table 1. Horizontal and vertical ridge changes in the DL group from baseline to 4 months of healing.
| No. (n=6) | Tooth site | Horizontal ridge changes (mm) | Vertical ridge changes (mm) | ||||
|---|---|---|---|---|---|---|---|
| HW1 | HW3 | HW5 | BH | MH | LH | ||
| 1 | #34 | −1.6 | −0.9 | −0.4 | −3.3 | 1.4 | −1.1 |
| 2 | #36 | −2.4 | −1.1 | −0.8 | −1.3 | −1.0 | −0.2 |
| 3 | #37 | −2.1 | −1.4 | −0.6 | −0.7 | −0.2 | −0.3 |
| 4 | #36 | −1.2 | −0.1 | −0.1 | −1.3 | −3.9 | −0.5 |
| 5 | #37 | −1.6 | −0.7 | −0.4 | −0.2 | −0.7 | −3.3 |
| 6 | #37 | −1.8 | −0.3 | −0.1 | −1.0 | 0.3 | −0.4 |
| Mean±SD | −1.8±0.4 | −0.8±0.5 | −0.4±0.3 | −1.3±1.1 | −0.7±1.8 | −1.0±1.2 | |
DL: the socket was filled with deproteinized bovine bone mineral with 10% collagen and covered by a double-layer of a collagen membrane, HW1–5: horizontal width in the 1-, 3-, and 5-mm apically below the ridge crest, BH: vertical change of the buccal alveolar crest, MH: vertical change of the mid-alveolar crest, LH: vertical change of the lingual alveolar crest, SD: standard deviation.
Table 2. Horizontal and vertical ridge changes in the SL group from baseline to 4 months of healing.
| No. (n=5) | Tooth site | Horizontal ridge changes (mm) | Vertical ridge changes (mm) | ||||
|---|---|---|---|---|---|---|---|
| HW1 | HW3 | HW5 | BH | MH | LH | ||
| 1 | #17 | −1.6 | −1.4 | −0.5 | −0.6 | −0.9 | −0.3 |
| 2 | #47 | −1.2 | −0.6 | −0.2 | −0.4 | −1.2 | −0.4 |
| 3 | #46 | −2.4 | −0.7 | −0.6 | −2.0 | −0.6 | −1.1 |
| 4 | #35 | −1.8 | −0.5 | −0.6 | −0.7 | −0.6 | −1.2 |
| 5 | #47 | −1.3 | −1.6 | −0.5 | −0.4 | −0.4 | −0.5 |
| Mean±SD | −1.7±0.5 | −1.0±0.5 | −0.5±0.2 | −0.8±0.7 | −0.7±0.3 | −0.7±0.4 | |
SL: the socket was filled with deproteinized bovine bone mineral with 10% collagen and covered by a single-layer of a collagen membrane, HW1–5: horizontal width in the 1-, 3-, and 5-mm apically below the ridge crest, BH: vertical change of the buccal alveolar crest, MH: vertical change of the mid-alveolar crest, LH: vertical change of the lingual alveolar crest, SD: standard deviation.
Among the parameters for vertical changes (BH, MH, and LH), the mean value of BH in the DL group showed the greatest difference compared to the SL group, but this difference was attributable to tooth #1 in the DL group. BH, MH, and LH in the DL group were −1.3±1.1, −0.7±1.8, and −1.0±1.2 mm, respectively, and the corresponding values in the SL group were −0.8±0.7, −0.7±0.3, and −0.7±0.4 mm, respectively.
DISCUSSION
As mentioned above, the double-layer technique in guided bone regeneration was originally proposed by Buser et al. [18,19], and Kim et al. [20] reported that the double-layer technique significantly reduced the resorption rate of overlay block-bone graft. The same approaches have been reported in studies of ARP without primary closure. Some authors used a single-layer of a resorbable collagen membrane [9,10,13,15], while others used double-layers for open-healing ARP procedures [11]. To the best of the authors' knowledge, however, this is the first study to compare single coverage and double coverage with collagen membranes in open-healing ARP procedures in terms of the quantitative effects of counteracting the atrophy of the edentulous ridge.
Our initial hypothesis was that the double-layer would preserve the alveolar ridge dimension better than the single-layer, because 1) double-layers of collagen membrane take longer to be degraded than single-layer and can therefore provide better stabilization for bone graft materials, and 2) the inner layer of the double-layer would be rapidly incorporated into the host tissue and infiltrated by vascularization [21], while the outer layer was expected to function as a dressing for the inner layer, enhancing its barrier function. Nevertheless, the results did not show any substantial difference in the radiographic analysis or clinical analysis between the SL and DL groups in the quantitative evaluation, contrary to our hypothesis.
However, there are some limitations in this study. First, the severity of periodontitis in the enrolled patients when the tooth extraction was performed was not fully standardized. Second, the method of suturing used to finish the ARP technique was not consistent. Some of the subjects had X sutures, while others received hidden X sutures. In the previous study by the current authors, Hidden X sutures have been proven to be advantageous for counteracting alveolar ridge resorption and preserving more width of the keratinized tissue [16].
Despite these limitations, however, DL could have potential advantages. It is well accepted that exposure of collagen membranes to the oral environment makes them degrade even faster. Therefore, the outer layer of collagen membranes applied in double-layer coverage still can function as an extra barrier membrane, helping ensure a stable healing process by protecting the underlying collagen membrane [20]. Double-layer membrane coverage may prove useful for clinicians, especially when treating patients with a delayed healing potential or who cannot comply well with the oral hygiene requirements for soft tissue.
The current pilot study provided clinical and radiographic verification that single-layer and double-layer treatments provided comparable results in terms of preserving the edentulous ridge from atrophy, with similar healing results. The limitations of this study warrant further research to fully evaluate the difference between single-layer and double-layer membrane coverage for open-healing ARP.
Footnotes
Author Contributions: Conceptualization: Ho-Keun Choi, Jung-Chul Park; Formal analysis: Ho-Keun Choi, Hag-Yeon Cho, Sung-Jo Lee, Hyun-Chang Lim; Investigation: Ho-Keun Choi, Hag-Yeon Cho, In-Woo Cho, Hyun-Seung Shin; Methodology: Ho-Keun Choi, Sung-Jo Lee, In-Woo Cho, Hyun-Seung Shin; Project administration: Jung-Chul Park; Writing - original draft: Ho-Keun Choi; Writing - review & editing: Ki-Tae Koo, Hyun-Chang Lim, Jung-Chul Park.
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Tallgren A. The continuing reduction of the residual alveolar ridges in complete denture wearers: a mixed-longitudinal study covering 25 years. J Prosthet Dent. 1972;27:120–132. doi: 10.1016/0022-3913(72)90188-6. [DOI] [PubMed] [Google Scholar]
- 2.Atwood DA. Reduction of residual ridges: a major oral disease entity. J Prosthet Dent. 1971;26:266–279. doi: 10.1016/0022-3913(71)90069-2. [DOI] [PubMed] [Google Scholar]
- 3.Schropp L, Wenzel A, Kostopoulos L, Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003;23:313–323. [PubMed] [Google Scholar]
- 4.Araújo MG, Lindhe J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol. 2005;32:212–218. doi: 10.1111/j.1600-051X.2005.00642.x. [DOI] [PubMed] [Google Scholar]
- 5.Tan WL, Wong TL, Wong MC, Lang NP. A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clin Oral Implants Res. 2012;23(Suppl 5):1–21. doi: 10.1111/j.1600-0501.2011.02375.x. [DOI] [PubMed] [Google Scholar]
- 6.Kentros GA, Filler SJ, Rothstein SS. Six month evaluation of particulate Durapatite in extraction sockets for the preservation of the alveolar ridge. Implantologist. 1985;3:53–62. [PubMed] [Google Scholar]
- 7.Cohen ES. Ridge enhancement and socket preservation utilizing the subepithelial connective tissue graft: a case report. Pract Periodontics Aesthet Dent. 1995;7:53–58. [PubMed] [Google Scholar]
- 8.Artzi Z, Nemcovsky CE. The application of deproteinized bovine bone mineral for ridge preservation prior to implantation. Clinical and histological observations in a case report. J Periodontol. 1998;69:1062–1067. doi: 10.1902/jop.1998.69.9.1062. [DOI] [PubMed] [Google Scholar]
- 9.Cardaropoli D, Cardaropoli G. Preservation of the postextraction alveolar ridge: a clinical and histologic study. Int J Periodontics Restorative Dent. 2008;28:469–477. [PubMed] [Google Scholar]
- 10.Araújo MG, Lindhe J. Ridge alterations following tooth extraction with and without flap elevation: an experimental study in the dog. Clin Oral Implants Res. 2009;20:545–549. doi: 10.1111/j.1600-0501.2008.01703.x. [DOI] [PubMed] [Google Scholar]
- 11.Roccuzzo M, Gaudioso L, Bunino M, Dalmasso P. Long-term stability of soft tissues following alveolar ridge preservation: 10-year results of a prospective study around nonsubmerged implants. Int J Periodontics Restorative Dent. 2014;34:795–804. doi: 10.11607/prd.2133. [DOI] [PubMed] [Google Scholar]
- 12.Mardas N, Chadha V, Donos N. Alveolar ridge preservation with guided bone regeneration and a synthetic bone substitute or a bovine-derived xenograft: a randomized, controlled clinical trial. Clin Oral Implants Res. 2010;21:688–698. doi: 10.1111/j.1600-0501.2010.01918.x. [DOI] [PubMed] [Google Scholar]
- 13.Engler-Hamm D, Cheung WS, Yen A, Stark PC, Griffin T. Ridge preservation using a composite bone graft and a bioabsorbable membrane with and without primary wound closure: a comparative clinical trial. J Periodontol. 2011;82:377–387. doi: 10.1902/jop.2010.090342. [DOI] [PubMed] [Google Scholar]
- 14.Pellegrini G, Rasperini G, Obot G, Farronato D, Dellavia C. Soft tissue healing in alveolar socket preservation technique: histologic evaluations. Int J Periodontics Restorative Dent. 2014;34:531–539. doi: 10.11607/prd.1857. [DOI] [PubMed] [Google Scholar]
- 15.Barone A, Toti P, Piattelli A, Iezzi G, Derchi G, Covani U. Extraction socket healing in humans after ridge preservation techniques: comparison between flapless and flapped procedures in a randomized clinical trial. J Periodontol. 2014;85:14–23. doi: 10.1902/jop.2013.120711. [DOI] [PubMed] [Google Scholar]
- 16.Park JC, Koo KT, Lim HC. The hidden X suture: a technical note on a novel suture technique for alveolar ridge preservation. J Periodontal Implant Sci. 2016;46:415–425. doi: 10.5051/jpis.2016.46.6.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cho IW, Park JC, Shin HS. A comparison of different compressive forces on graft materials during alveolar ridge preservation. J Periodontal Implant Sci. 2017;47:51–63. doi: 10.5051/jpis.2017.47.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19(Suppl):43–61. [PubMed] [Google Scholar]
- 19.von Arx T, Buser D. Horizontal ridge augmentation using autogenous block grafts and the guided bone regeneration technique with collagen membranes: a clinical study with 42 patients. Clin Oral Implants Res. 2006;17:359–366. doi: 10.1111/j.1600-0501.2005.01234.x. [DOI] [PubMed] [Google Scholar]
- 20.Kim SH, Kim DY, Kim KH, Ku Y, Rhyu IC, Lee YM. The efficacy of a double-layer collagen membrane technique for overlaying block grafts in a rabbit calvarium model. Clin Oral Implants Res. 2009;20:1124–1132. doi: 10.1111/j.1600-0501.2009.01744.x. [DOI] [PubMed] [Google Scholar]
- 21.Zitzmann NU, Naef R, Schärer P. Resorbable versus nonresorbable membranes in combination with Bio-Oss for guided bone regeneration. Int J Oral Maxillofac Implants. 1997;12:844–852. [PubMed] [Google Scholar]