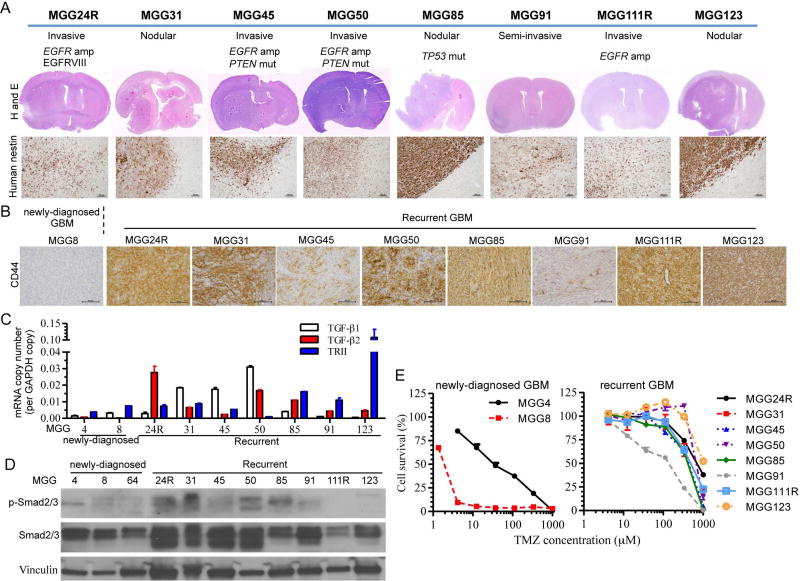
Figure 1. Generation of recurrent GSCs-derived orthotopic xenografts and characterization of their mesenchymal phenotype.
(A) Histopathological and molecular characterization of orthotopic xenografts generated from recurrent GSCs established from 8 patients. Molecular (EGFR amplification, P53 and PTEN status) and phenotypic features (invasive vs nodular)(upper). Hematoxylin and eosin (H&E) stain of coronal sections of xenografts (middle) and microscopic images of human nestin immunohistochemistry (lower, original magnification, 100×, scale bars: 100 µm). (B) CD44 immunohistochemistry of GSC xenografts. All the xenografts generated from recurrent GBM expressed CD44 (brown, original magnification, 200×, scale bars: 100 µm). Newly diagnosed GBM-derived model, MGG8, served as negative control. (C) Quantitative RT-PCR analysis of TGF-β1, TGF-β2 and TGF-β receptor type II (TRII) mRNA levels in newly diagnosed and recurrent GSCs. GAPDH was used as reference. Data are shown as mean ± SD. (D) Western blot analysis of TGF-β receptor signal transducer Smad2/3 and its phosphorylation in newly diagnosed and recurrent GSCs. Vinculin is loading control. (E) Cell viability assay showing temozolomide (TMZ) dose response curves of newly diagnosed (left) and recurrent GSCs (right) in vitro. Cells were exposed to TMZ for 5 days. Data are shown as mean ± SD.