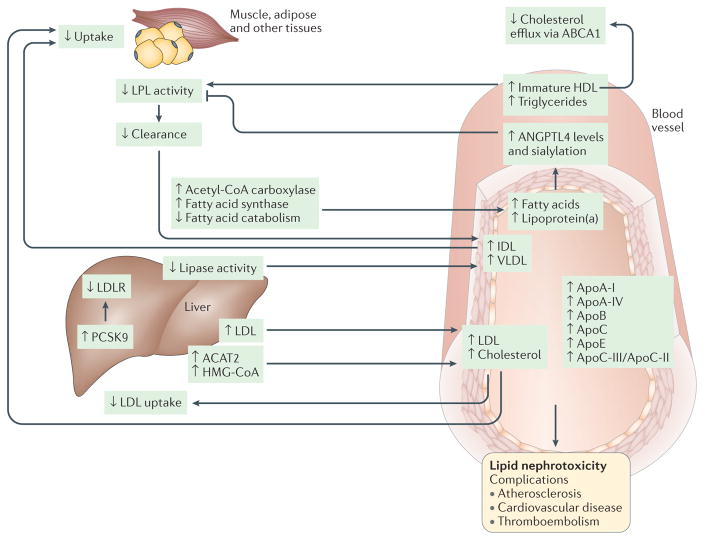
Figure 2. Pathophysiology of dyslipidaemia in nephrotic syndrome.
Alterations of lipid and lipoprotein metabolism in nephrotic syndrome result in ‘lipid nephrotoxicity’ and other complications, such as atherosclerosis, cardiovascular disease and thromboembolism. The major lipoproteins, including intermediate density lipoprotein (IDL), very low density lipoprotein (VLDL) and low-density lipoprotein (LDL), and cholesterol are increased in the plasma of patients with nephrotic syndrome, owing mainly to impaired clearance and, to a lesser extent, increased biosynthesis. Impaired clearance is a direct result of decreased hepatic lipase activity and decreased lipoprotein lipase (LPL) activity in the endothelium and peripheral tissues, such as muscle and adipose. In addition, hepatic levels of proprotein convertase subtilisin/kexin type 9 (PCSK9) are increased in patients with nephrotic syndrome; PCSK9 degrades the LDL receptor (LDLR), and is thus a major therapeutic target for lipid lowering. Furthermore, the composition and function of the lipoproteins are also altered, with substantial increases in the plasma levels of apolipoprotein A I (ApoA I), ApoA IV, ApoB, ApoC and ApoE, and in the ApoC III/ApoC II ratio. The level of immature HDL in the plasma is also increased, resulting in reduced cholesterol efflux, which occurs mainly via ATP binding cassette subfamily A member 1 (ABCA1), in peripheral organs, including in podocytes. Another major lipid abnormality in nephrotic syndrome is hypertriglyceridaemia, as well as increased production and sialylation of ANGPTL4, which is driven primarily by increased circulating free fatty acids. ANGPTL4 in turn suppresses LPL activity by either preventing its dimerization or by inhibiting its activity noncompetitively. Hypercholesterolaemia and increased LDL levels occur in conjunction with upregulation of the expression and activity of liver acetyl CoA acetyltransferase 2 (ACAT2), which results in enhanced esterification of cholesterol and a reduction in the level of intracellular free cholesterol. Cholesterol synthesis via 3 hydroxy 3 methylglutaryl CoA (HMG CoA) reductase is also increased in experimental models of nephrotic syndrome. Evidence also exists that LDL oxidation in nephrotic syndrome may be augmented by lipoprotein(a), the level of which is also increased in patients with nephrotic syndrome. Accumulation of oxidized LDL, IDL and chylomicron remnants stimulates monocytes and macrophages to release proin ammatory cytokines and chemokines, and accelerates in ammation, which may in turn promote the progression of chronic kidney disease.