Abstract
Marfan syndrome is an autosomal dominant disorder involving mutation in the FBN1 gene, which encodes fibrillin-1, a protein critical to maintain the integrity of connective tissue. A mutation in this gene can affect multiple organ systems, but it is not classically associated with gastrointestinal complications. We describe a man with Marfan syndrome with multiple small bowel diverticula leading to small intestinal bacterial overgrowth and recurrent small bowel perforations.
Introduction
Small bowel diverticula are rare and are usually asymptomatic.1 Most small bowel diverticula are found in the duodenum, followed by the jejunum and ileum.1-3 Although they are usually not clinically significant, complications can occur, and they are more common in jejunoileal diverticula. Complications include bleeding, diverticulitis, perforation, obstructive ileus, volvulus, and malabsorptive diarrhea.2-4
Case Report
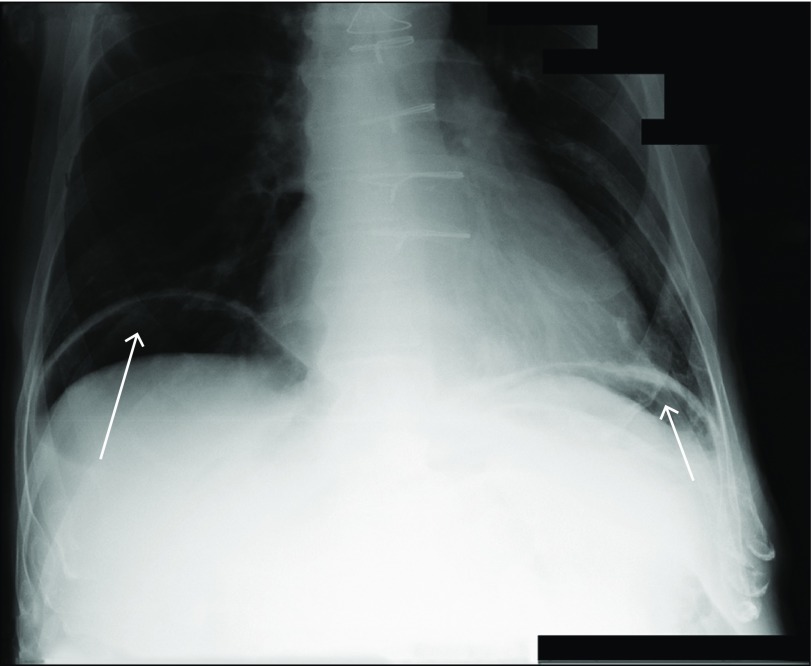
A 68-year-old man with a history of Marfan syndrome and aortic root replacement presented to the gastroenterology clinic with chronic diarrhea, abdominal bloating, and weight loss. He was diagnosed with Marfan syndrome by Ghent nosology criteria with aortic dilatation (i.e., Z score ≥2 above 20 years old), and his family history revealed Marfan syndrome in his son. A geneticist excluded an alternative diagnosis of connective tissue disorders (e.g., Shprintzen Goldberg syndrome, Loey-Dietz syndrome, and vascular Ehlers-Danlos syndrome) through genetic testing. On evaluation, the patient’s stool studies were consistent with a malabsorptive diarrhea. Small intestinal bacterial overgrowth (SIBO) was diagnosed via hydrogen breath test, with a baseline H2 of 221 parts per million (ppm; normal <10 ppm) and peak H2 of 416 ppm. This prompted a small bowel follow-through, which showed extensive jejunal and ileal diverticulosis (Figure 1). Despite repeated courses of antibiotics (metronidazole, ciprofloxacin, and doxycycline), symptoms persisted and serial hydrogen breath tests remained positive, although he was clinically stable without worsening or decompensation.
Figure 1.

Small bowel diverticulosis primarily involving the jejunum and ileum.
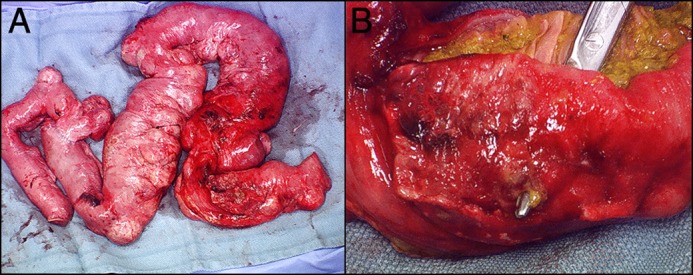
Approximately 3 years later, the patient presented to the hospital with diffuse, acute abdominal pain. Physical exam was consistent with marfanoid habitus and an acute abdomen. Labs were remarkable for leukocytosis 13.0 × 109/L and hemoglobin 9.0 g/dL. An anteroposterior chest x-ray demonstrated free intraperitoneal air (Figure 2). Urgent exploratory laparotomy showed diffuse diverticulosis of the small bowel with a perforated distal jejunal diverticulum and abscess (Figure 3). He underwent resection of the affected bowel with a primary anastomosis. Surgical pathology was consistent with acute diverticulitis with perforation.
Figure 2.
Chest x-ray with intraperitoneal free air (arrows).
Figure 3.
(A) Surgical resection specimen showing a dilated, necrotic small bowel with multiple diverticuli. (B) Close-up view of the perforation site.
One year later, despite cycling antibiotics for bacterial overgrowth, he presented with acute abdominal pain, and computed tomography (CT) demonstrated intraperitoneal free air (Figure 4). Upon laparotomy, a perforated jejunal diverticulum was noted near his previous anastomosis, as well as 4 feet of necrotic small bowel with large-mouthed diverticula. This diseased area and approximately 95% of the jejunal diverticula were resected. Pathology was remarkable for intestinal perforation secondary to diverticular disease without evidence of diverticulitis. Postoperatively, his symptoms initially improved, but he again developed recurrent bloating, and repeat hydrogen breath test was positive. Oral antibiotics were again prescribed on a cycling basis.
Figure 4.
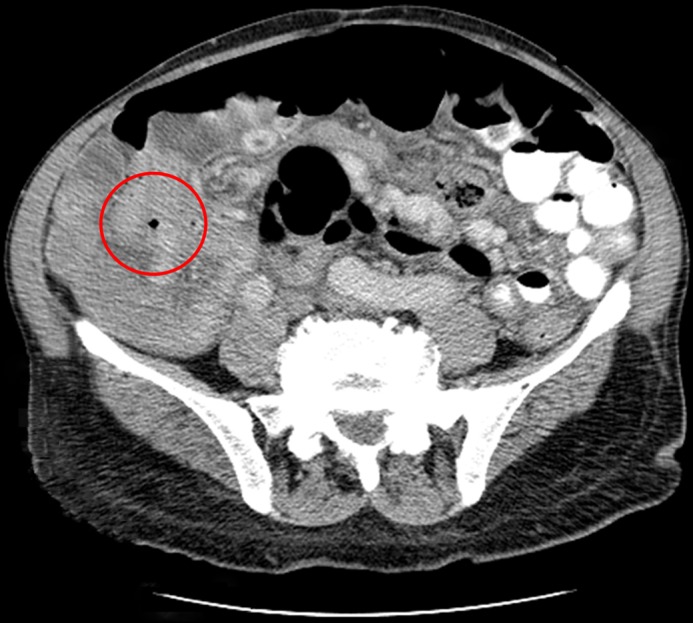
Computed tomography of the abdomen/pelvis with intraperitoneal free air (red circle).
The patient presented 6 years later with abdominal pain. An abdominal CT showed free air and diffuse small bowel inflammation. A third exploratory laparotomy again revealed a perforation just distal to the previous anastomosis at a residual small bowel diverticulum. Sixty centimeters of small bowel were removed, including nearly all of the remaining diverticulosis, because this segment was involved by adhesions in addition to the perforation. His pathology was notable for diverticulosis with subserosal abscess formation and severe acute serositis, consistent with perforated diverticulosis.
For over a year, his symptoms of bloating, abdominal cramping, and diarrhea improved considerably, presumably because the underlying anatomic predisposition to bacterial overgrowth was corrected, and he has remained free of subsequent intestinal perforations.
Discussion
Marfan syndrome is an autosomal dominant connective tissue disease with high penetrance caused by a fibrillin-1 gene mutation.5 This syndrome typically affects the ocular and vascular systems. Gastrointestinal complications are uncommon but can include bowel obstructions, colonic diverticula, and hiatal and inguinal hernias.6,7 Although there are several case reports describing colonic diverticula and subsequent large-bowel perforation in patients with Marfan syndrome, there are limited data regarding small bowel diverticular disease and perforation.
There are 3 reported cases of perforated diverticulitis of the small bowel in Marfan syndrome. One case describes a 27-year-old man with recurrent small bowel obstructions and a perforated diverticulum of the terminal ileum after presenting with an acute abdomen.8 A 30-year-old woman presented with a perforated diverticulum from diverticulitis proximal to a small bowel obstruction. It was hypothesized that the diverticulitis was secondary to the mechanical obstruction.9 Another case describes a 41-year-old man with known jejunal diverticula and SIBO hospitalized for pneumoperitoneum that resolved spontaneously.10
Our patient’s underlying connective tissue disorder may have predisposed him to structural defects along the small bowel wall, leading to diffuse diverticulosis. In turn, diverticulosis predisposed him to developing severe SIBO, which contributed to the initial episode of diverticulitis with perforation. His persistent SIBO likely compromised his small bowel wall further, which led to the diverticular-free wall perforations. His chronic antibiotic treatment for SIBO may have delayed or masked his presentation with pneumoperitoneum. In contrast to the other cases, which were largely reported decades ago, we describe a small bowel perforation secondary to diverticulitis that was not preceded by a small bowel obstruction. Our patient is also unique in that he presented with gastrointestinal manifestations of Marfan syndrome at an advanced age.
The importance of the defective mucosa in the pathogenesis of perforations was suggested by a case of Marfan syndrome with spontaneous recurrent perforations of the small bowel without the presence of diverticula.11 In that case, the histopathology showed abnormalities in the appearance of the small bowel submucosa similar to those found in the aorta in Marfan syndrome. Such a mucosal defect in the setting of small bowel diverticulosis may explain why our patient had recurrent perforations, although we do not have definitive evidence of this. It is also notable that chronic antibiotic use in this patient, while preventing subsequent bouts of diverticulitis, did not mitigate his bowel-perforation risk.
It is important to recognize that connective tissue diseases, like Marfan syndrome, can lead to structural defects in the gastrointestinal system, causing complications such as diverticulitis and small bowel perforation. Preventive measures may include surgical consultation for removal of all small bowel diverticula during the first episode of small bowel perforation in a patient with Marfan syndrome. Moreover, very high values on breath testing should trigger an evaluation for small bowel diverticulosis, particularly in patients with connective tissue disorders.
Disclosures
Author contributions: BS Robey wrote and edited the manuscript. AF Peery and ES Dellon edited the manuscript. ES Dellon is the article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
References
- 1.Gross SA, Katz S. Small bowel diverticulosis: An overlooked entity. Curr Treat Options Gastroenterol. 2003;6(1):3–11. [DOI] [PubMed] [Google Scholar]
- 2.Akhrass R, Yaffe MB, Fischer C, Ponsky J, Shuck JM. Small-bowel diverticulosis: Perceptions and reality. J Am Coll Surg. 1997;184(4):383–8. [PubMed] [Google Scholar]
- 3.Mantas D, Kykalos S, Patsouras D, Kouraklis G. Small intestine diverticula: Is there anything new? World J Gastrointest Surg. 2011;3(4):49–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hu JL, Chen WZ. Midgut volvulus due to jejunal diverticula: A case report. World J Gastroenterol. 2012;18(40):5826–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Canadas V, Vilacosta I, Bruna I, Fuster V. Marfan syndrome. Part 1: Pathophysiology and diagnosis. Nat Rev Cardiol. 2010;7(5):256–65. [DOI] [PubMed] [Google Scholar]
- 6.Thomas GP, Purkayastha S, Athanasiou T, Darzi A. General surgical manifestations of Marfan's syndrome. Br J Hosp Med (Lond). 2008;69(5):270–4. [DOI] [PubMed] [Google Scholar]
- 7.Eliashar R, Sichel JY, Biron A, Dano I. Multiple gastrointestinal complications in Marfan syndrome. Postgrad Med J. 1998;74(874):495–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clunie GJ, Mason JM. Visceral diverticula and the Marfan syndrome. Brit J Surg. 1962;50:51–2. [DOI] [PubMed] [Google Scholar]
- 9.Shapira O, Mavor E, Simon D, Rothstein H, Pfeffermann R. Multiple giant gastrointestinal diverticula complicated by perforated jejunoileal diverticulitis in Marfan syndrome. Dig Surg. 1992;9:58–60. [Google Scholar]
- 10.McLean AM, Paul RE Jr., Kritzman J, Farthing MJ. Malabsorption in Marfan (Ehlers-Danlos) syndrome. J Clin Gastroenterol. 1985;7(4):304–8. [DOI] [PubMed] [Google Scholar]
- 11.Darmaillacq RL, Moretti G. [Spontaneous perforations of the small intestine and Marfan's syndrome]. Mem Acad Chir (Paris). 1965;91:165–9. [PubMed] [Google Scholar]