Abstract
We describe three cases of inadvertent placement of the urinary catheter into the ureter. An 85-year-old gentleman on long-term indwelling catheter (IDC) for neurogenic bladder presented with fever and right flank pain. CT of abdomen and pelvis demonstrated the tip of the IDC to be located within the right vesicoureteric junction with acute right hydronephrosis and acute pyelonephritis. A 74-year-old woman, on long-term IDC for neurogenic bladder was found to have hydronephrosis on ultrasound imaging. Contrast-enhanced CT intravenous pyelography done subsequently showed the IDC was in the right distal ureter. A 47-year-old lady, on IDC for urinary retention and voiding dysfunction likely secondary to schizophrenia and anti-psychotic medications, presented with raised creatinine. A non-enhanced CT of her abdomen and pelvis was done and showed that the tip of the urethral IDC was located up to the left vesicoureteric junction. In all patients, the hydronephrosis resolved after changing the catheter and they were well on discharge. We also review the literature to identify the incidence, outcomes and possible risk factors. To our knowledge, only 20 cases have been reported thus far in the English literature. Although serious complications can occur, the incidence is very low. One risk factor that has been identified is long-term catheterization in patients with neurogenic bladder. We do not recommend routine imaging after catheterization in this group of patients. However, we should still be mindful of the possibility of this occurrence and evaluate and treat as necessary when clinical suspicion arises.
Keywords: Indwelling catheter, Ureter, Complication
1. Introduction
Insertion of urinary catheters, either indwelling urethral catheters (IDC) or supra-pubic catheters (SPC), is among the most common urological clinical procedures performed. In the majority of cases, this is uneventful with the tip and the balloon of catheter residing within the urinary bladder. Inadvertent placement of the urinary catheter into the ureter is a rare but possible occurrence and may cause complications such as ureteric obstruction with hydronephrosis, ureteric injury or even ureteric rupture.
The purpose of this paper is to describe three such cases encountered in our institution, to review the literature, to suggest the possible reasons for this rare occurrence and to suggest measures to prevent this.
2. Case report
2.1. Case 1
An 85-year-old Malay gentleman, with a past medical history of hypertension, hyperlipidaemia & chronic obstructive pulmonary disease (COPD); on long-term urethral catheter for neurogenic bladder secondary to cystic schwannoma at the L2/L3 level, presented with acute onset of high grade fever, chills and right flank pain. He had his catheter changed by a nurse at the nursing home 2 days prior to presentation.
Contrast-enhanced computer tomographic scan of his abdomen and pelvis (CT AP) demonstrated the tip of the urethral catheter to be located within the right vesicoureteric junction (VUJ) and obstructing it with resultant acute right hydronephrosis and hydroureter (Fig. 1). The right kidney was also noted to be bulky and showed multiple non-enhancing areas with perinephric fat stranding suggestive of acute pyelonephritis.
Figure 1.
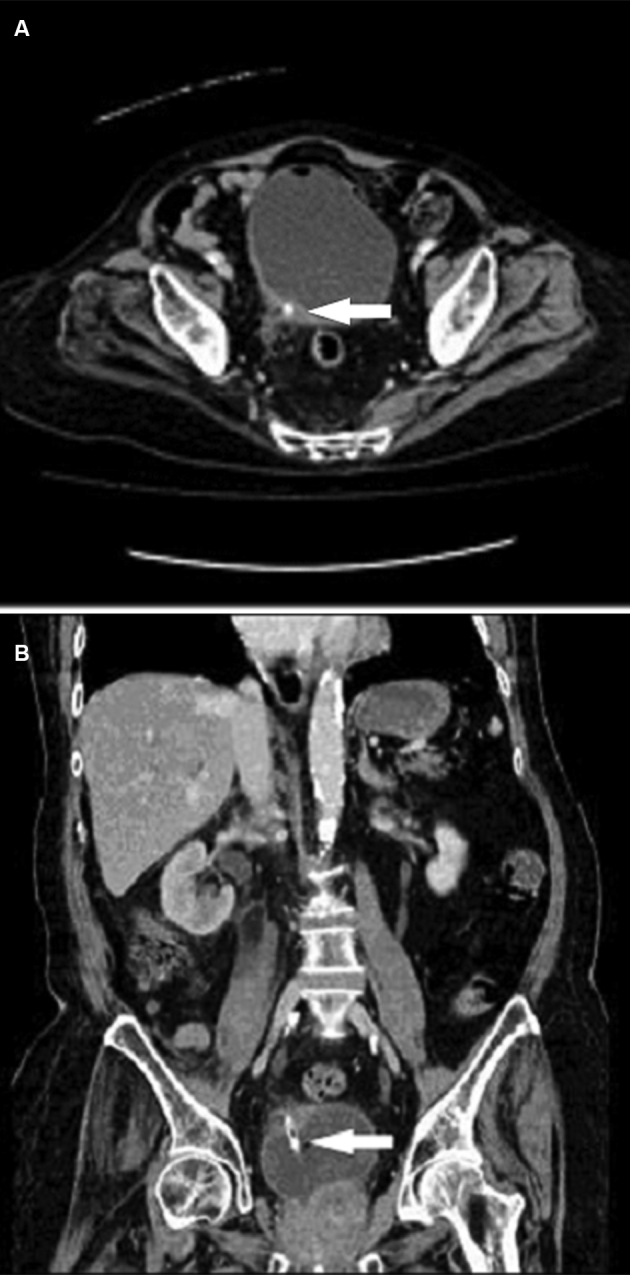
An 85-year old man, CT scan: the tip of the vesicoureteric catheter within the right vesicoureteric junction (arrows). (A) Cross section; (B) Coronal view.
The aberrantly placed catheter was removed and a new Foley catheter was reinserted. He was treated with intravenous Aztreonam based on positive blood and urine cultures which grew Klebsiella pneumoniae. The patient was discharged after completion of 14 days of antibiotics with resolution of all symptoms.
Nine months after this episode, the patient presented at our institution with the complaint of no urine output from urethral IDC. Ultrasound of his kidneys and bladder was performed and showed that the tip of the catheter was within the right VUJ again (Fig. 2). A new catheter was placed but the tip was found to still lie within the right ureter 2 days after insertion. The urethral catheter was then removed and the patient was taught clean intermittent catheterization (CIC).
Figure 2.
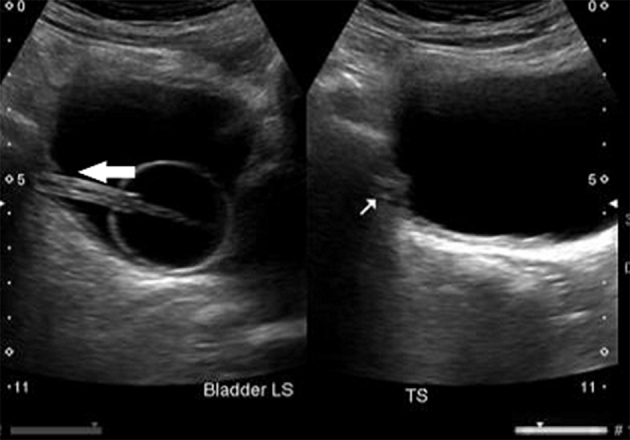
An 85-year old man, ultrasound: the tip of the catheter in the right junction with balloon within urinary bladder (arrows).
2.2. Case 2
A 74-year-old Chinese woman, with a past medical history of hypertension and uterine cancer status post hysterectomy and radiotherapy; on long-term urethral IDC for detrusor underactivity following radiotherapy, was admitted to our institution following a fall. An ultrasound (US) scan of her abdomen, which was performed for investigation of transaminitis, showed incidental bilateral hydronephrosis. Contrast-enhanced CT intravenous pyelography (CT IVP) showed right hydronephrosis and hydroureter secondary to obstruction from the tip of the urethral catheter which had be placed in the right distal ureter. Her IDC was removed and she was able to void with minimal residual urine.
She was subsequently transferred to the medical intensive care unit (MICU) in view of desaturation secondary to hospital acquired pneumonia and required intubation and ventilatory support. During her stay in the MICU, a urethral IDC was inserted for monitoring of her urine output. However, no output was noted from the newly inserted IDC. A non-contrast CT scan of her abdomen and pelvis was done and showed the urinary catheter with its inflated balloon and tip to be located in the right mid-ureter again with resultant right hydronephrosis. A new urethral catheter was inserted and a repeat CT pelvis was performed to confirm that the location of the tip of the IDC was located within the urinary bladder (Fig. 3). The scan showed that the right mid-ureter appeared dilated and hyperdense. Due to the absence of contrast, ureteric injury or rupture was unable to be excluded.
Figure 3.

A 74-year old woman, CT scan: the tip of urinary catheter in the right ureter with balloon (arrows) inflated. (A) Cross section; (B) Coronal view.
Flexible cystoscopy with right ureteric catheter insertion and right retrograde pyelography (RPG) was performed in order to exclude ureteric rupture. Cystoscopy showed the bladder to be small and contracted while the right ureteric orifice was noted to be dilated and patulous. The RPG showed no contrast extravasation. A new urethral catheter was then placed for urine output monitoring.
The patient was treated with oral Ciprofloxacin according to urine and blood cultures which grew enterobacter. Her IDC was subsequently removed and she was able to void successfully. Her condition improved and she was well on discharge.
2.3. Case 3
A 47-year-old Chinese lady, on long-term urethral IDC for urinary retention and voiding dysfunction likely secondary to schizophrenia and anti-psychotic medications, presented to urology clinic with raised creatinine. A non-enhanced CT abdomen and pelvis (Fig. 4) was performed and it showed that the tip of the urethral IDC was located up to the left vesicoureteric junction.
Figure 4.
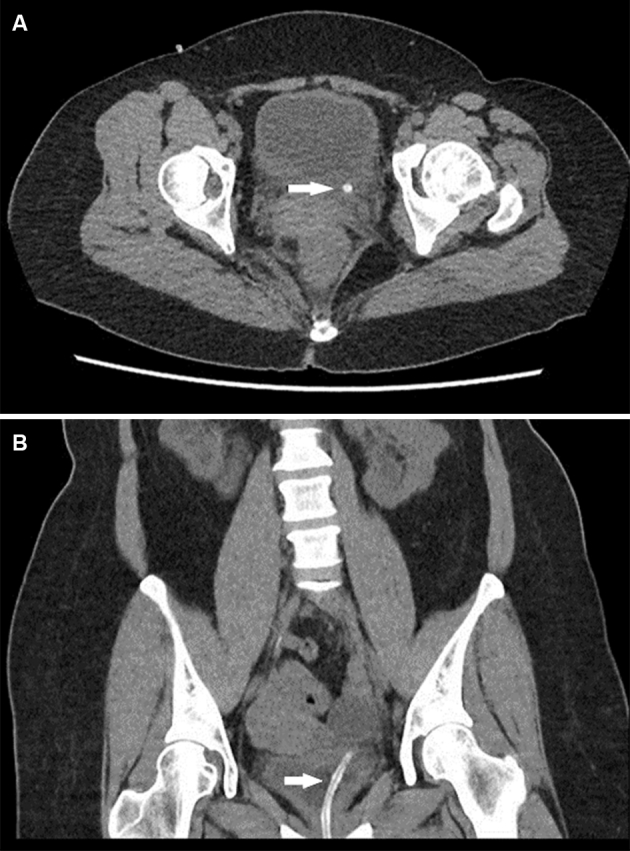
CT scan cross section: the tip of the urinary catheter in the left ureter. (A) Cross section; (B) Coronal view.
The patient was called back to clinic due to the CT findings. The IDC was removed and a new IDC was reinserted. Subsequently an ultrasound bladder was performed which showed the tip of the urethral catheter was in the bladder. The patient was then discharged well from clinic.
3. Literature review
Reports of such cases are few and this reflects the low incidence of the aberrant urethral or suprapubic catheter. To our knowledge, only 20 cases have been reported thus far in the English literature (16 cases of IDC and four cases of SPC). These cases are summarised in Table 1.
Table 1.
Cases reported in the English literature.
| Author | Year | Case | IDC/SPC | Age (year) | Gender | Side | Long-term catheter | Presentation | Diagnosis | Consequences | Treatment |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Borrero et al. [1] | 1987 | 1 | SPC | 35 | Male | Left | Yes | Left flank pain, fever | IVU | Pyelonephritis | Catheter changed |
| Singh and Eardley [2] | 1996 | 1 | IDC | 26 | Female | Right | Yes | Incidental | Intra-operative | Ureteric rupture | Surgical repair |
| Kato [3] | 1997 | 1 | IDC | 74 | Female | Left | Yes | Blocked IDC | Fluoroscopy | No adverse outcomes | Catheter changed |
| Ogan and Berger [4] | 2001 | 1 | IDC | 47 | Female | Right | No | Incidental finding during angiography | Angiography | No adverse outcomes | Catheter changed |
| Muneer et al. [5] | 2002 | 1 | IDC | 77 | Male | Right | Yes | Loin pain, blocked IDC |
Cystoscopy | Catheter removed with endoscopic incision | Cystoscopy |
| Hara et al. [6] | 2005 | 1 | IDC | 51 | Female | Left | No | Peri-catheter urine leakage | Catheterography | No adverse outcomes | Insertion of DJ stent |
| George and Tharian [7] | 2005 | 1 | IDC | 14 | Male | Right | Yes | Peri-catheter urine leakage | US | No adverse outcomes | Catheter changed |
| Wang and Foote [8] | 2006 | 1 | IDC | 30 | Female | Right | No | Blocked IDC, unable to deflate balloon | Cystoscopy | No adverse outcomes | Catheter changed |
| Maegele et al. [9] | 2007 | 1 | IDC | 86 | Female | Left | N.A. | Abdominal pain, fever | CT | Pyelonephritis | Catheter changed |
| Kim and Park [10] | 2008 | 1 | IDC | 38 | Female | Right | Yes | Lower abdominal pain | Cystography | Ureteric rupture | DJ stent (failed) PCN |
| Dangle et al. [11] | 2010 | 1 | SPC | 50 | Female | Right | Yes | Flank pain | CT | Pyelonephritis | Catheter changed |
| Hale et al. [12] | 2012 | 1 | IDC | 80 | Female | Left | N.A. | Flank pain | CT | Ureteric rupture | Surgical repair |
| Papacharalabous et al. [13] | 2011 | 1 | IDC | 68 | Female | Left | No | Incidental | Intra-operative | Ureteric rupture | Surgical repair |
| Adeyemo et al. [14] | 2013 | 1 | SPC | 55 | Male | Right | Yes | Blocked SPC | CT | Pyelonephritis | Catheter changed |
| Baker et al. [15] | 2013 | 1 | IDC | 59 | Female | Left | Yes | Blocked IDC | CT | Ureteric rupture | PCN |
| Modi et al. [16] | 2014 | 1 | SPC | 83 | Female | Right | Yes | N.A. | N.A. | Ureteric rupture | DJ stent (failed) PCN |
| Ishikawa et al. [17] | 2014 | 1st | IDC | 81 | Male | Left | Yes | Fever | CT | Pyelonephritis | Catheter changed |
| 2nd | IDC | 67 | Female | Left | Yes | Fever | CT | Pyelonephritis | Catheter changed | ||
| 3rd | IDC | 37 | Female | Left | Yes | Peri-catheter urine leakage | US | No adverse outcomes | Catheter changed | ||
| Viswanatha et al. [18] | 2014 | 1 | IDC | 28 | Female | Right | No | Pain, unable to deflate balloon | RPG and ureteroscopy | No adverse outcomes | Catheter removed via ureteroscopy |
| Total | 20 | IDC 16 | Male 5 | R 10 | Long-term catheter 13 | ||||||
| SPC 4 | Female 15 | L 10 | |||||||||
CT, computed tomography; DJ stent, double J stent; IDC, indwelling catheter; IVU, intravenous urogram; N.A., unable to make sure the duration of catheter; PCN, percutaneous nephrostomy; RPG, retrograde pyelogram; SPC, suprapubic catheter; US, ultrasound.
Female patients are at a higher risk with a 1:3 male-to-female ratio. There was no difference between right and left sided ureteric involvement. Of the 20 cases, 15 patients were on long-term catheters and most of them were because of neurogenic bladder.
Seven patients presented with loin, flank or abdominal pain; eight patients presented with blocked catheter or peri-catheter urine leakage; four patients presented with fever; two patients presented with inability to deflate the balloon of the catheter; three cases were noted incidentally during abdominal surgery or angiography.
Seven cases were diagnosed by CT imaging; six cases diagnosed by X-ray studies with contrast (intravenous urography, retrograde pyelography or catheterography); two cases were diagnosed by ultrasound imaging; two cases were diagnosed intra-operatively; and two cases were diagnosed by cystoscopy which was performed to deflate the balloon of the catheter which had failed to be deflated.
After insertion of the catheter into the ureter, seven patients developed ureteric rupture; seven patients developed pyelonephritis; and 7 patients had no adverse outcomes.
Six out of the seven patients with ureteric rupture underwent open surgical repair while the remaining one underwent percutaneous nephrostomy insertion after failing ureteric stent insertion. For patients not complicated by ureteric rupture, one underwent successful ureteric stent insertion; while another required percutaneous nephrostomy (PCN) after failing double J stent insertion. Their catheters were changed or removed and the patients recovered. For the remaining 11 patients, their IDC or SPC was removed or changed and any urinary tract infection was treated.
4. Discussion
Inadvertent insertion of the IDC or SPC into the ureter is a rare complication of urinary catheterisation. Patients at higher risk are those who are on long-term IDC or SPC. There are a few possible reasons to account for this.
Firstly, for patients on long-term catheter, their bladder tends to become contracted (thus altering the anatomical relationship between the bladder neck and ureteric orifices) thus making it easier for the catheter to enter the ureter. This was seen in the second case in which her bladder was noted to be small and contracted. Secondly, their catheters have to be changed regularly and hence they have more opportunities for the catheter to be inadvertently placed into the ureter. Thirdly, patients on long-term urinary catheters for neurogenic bladders may also have vesicoureteric reflux with patulous ureteric orifices which are easier for the tip of the catheter to enter.
Based on the cases reported thus far, most patients are on long-term catheter for neurogenic bladder and majority of them have impaired sensation of varying degrees. As a result, their presentation may be delayed due to the absence of pain or discomfort. For these patients, the first clue may be the resistance encountered when inflating the balloon, peri-catheter urine leakage or blocked catheter, especially when flushing of the catheter is unsuccessful or causes pain. If the inadvertent placement of the catheter in the ureter is not detected in time or rupture of the ureter has occurred, these patients will subsequently present with symptoms of ureteric rupture, pyelonephritis or even pyonephrosis.
Though most cases are reported in patients on long-term catheter, the inadvertent placement of the catheter into the ureter can occur at the first insertion. For this group of patients, they are more likely to complain of lower abdominal or flank pain with earlier recognition of the problem.
The clinician should consider the diagnosis of a misplaced catheter in patients who present with blocked urinary catheters which are difficult to flush and if they complain of flank pain during flushing. An ultrasound of the bladder can be performed to confirm the location of the catheter and its balloon. As seven out of 20 reported cases were complicated by ureteric rupture and another seven patients were complicated by pyelonephritis, a contrast-enhanced CT scan should be considered to evaluate for possible complications and the need for subsequent intervention.
Patients without ureteric injury can be managed conservatively by either changing or removing the catheter and treating any urinary tract infection with antibiotics. Patients with ureteric rupture require urinary diversion either in the form of insertion of a ureteric stent or percutaneous nephrostomy. Surgical repair is indicated for severe ureteric injury or in the case of ureteric rupture.
Patients with history of insertion of the urinary catheter into the ureter, especially when the balloon is inflated within the ureter, are at risk of developing ureteric strictures in the future which may result in ipsilateral upper urinary tract obstruction. Such patients should be monitored with upper tract imaging such as ultrasound of the kidneys or CT IVP.
Patients with neurogenic bladders are at a higher risk of inadvertent placement of urinary catheters into the ureteric orifice. For this group of patients, we recommend the use of short-tip urinary catheters to reduce the incidence of ureteric catheterisation. If resources are available, we also recommend a bedside ultrasound of the bladder after insertion of the catheter to confirm that the location of the tip lies within the bladder.
Conflicts of interest
The authors declare no conflict of interest.
Footnotes
Peer review under responsibility of Second Military Medical University.
References
- 1.Borrero G.O., Miller P.R., Vora K., Nepjuk C.A. Acute ureteral obstruction as a complication of suprapubic catheterization. Urol Radiol. 1987;9:171–173. doi: 10.1007/BF02932654. [DOI] [PubMed] [Google Scholar]
- 2.Singh N.P., Eardley I. An uncommon complication of urethral catheterization. Br J Urol. 1996;77:316–317. doi: 10.1046/j.1464-410x.1996.91532.x. [DOI] [PubMed] [Google Scholar]
- 3.Kato H. Incorrect positioning of an indwelling urethral catheter in the ureter. Int J Urol. 1997;4:417–418. doi: 10.1111/j.1442-2042.1997.tb00218.x. [DOI] [PubMed] [Google Scholar]
- 4.Ogan K., Berger R.M. Aberrant Foley catheter placement into the proximal right ureter. BJU Int. 2001;88:124. [Google Scholar]
- 5.Muneer A., Minhas S., Harrison S.C. Aberrant Foley catheter placement into the proximal right ureter. BJU Int. 2002;89:795. doi: 10.1046/j.1464-410x.2002.t01-7-02801.x. [DOI] [PubMed] [Google Scholar]
- 6.Hara N., Koike H., Bilim V., Takahashi K. Placement of a urethral catheter into the ureter: an unexpected complication after retropubic suspension. Int J Urol. 2005;12:217–219. doi: 10.1111/j.1442-2042.2005.01011.x. [DOI] [PubMed] [Google Scholar]
- 7.George J., Tharion G. Transient hydroureteronephrosis caused by a Foley's catheter tip in the right ureter. ScientificWorldJournal. 2005;5:367–369. doi: 10.1100/tsw.2005.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang D., Foote A. A rare complication of an indwelling urinary catheter – ureteral entrapment. Aust N Z J Obestet Gynaecol. 2006;46:459–460. doi: 10.1111/j.1479-828X.2006.00636.x. [DOI] [PubMed] [Google Scholar]
- 9.Maegele M., Gruetzner U., Wenzel D. Transurethral catheter in the distal ureter as a cause for acute abdominal pain. Emerg Med J. 2007;24:599. doi: 10.1136/emj.2006.040402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim M.K., Park K. Unusual complication of urethral catheterization:a case report. J Korean Med Sci. 2008;23:161–162. doi: 10.3346/jkms.2008.23.1.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dangle P.P., Tycast J., Vasquez E., Geary B., Chehval M. Suprapubic cystostomy: a bizarre complication of catheter migration causing ureteric obstruction. Can Urol Assoc J. 2010;4:E127–E128. doi: 10.5489/cuaj.934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hale N., Baugh D., Womack G. Mid-ureteral rupture: a rare complication of urethral catheterization. Urology. 2012;80:e65–e66. doi: 10.1016/j.urology.2012.07.011. [DOI] [PubMed] [Google Scholar]
- 13.Papacharalabous E., Ford M., Butler-Manuel S., Tailor A. Inadvertent insertion of a Foley's catheter through the orifice of a duplex ureter during catheterisation for laparotomy. Gynecol Surg. 2011;8:99–101. [Google Scholar]
- 14.Adeyemo B., Makovitch S., Foo D. A peculiar complication of suprapubic catheterization: recurrent ureteral obstruction and hydronephrosis. J Spinal Cord Med. 2013;36:166–169. doi: 10.1179/2045772312Y.0000000080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baker K.S., Dane B., Edelstein Y., Malhotra A., Gould E. Ureteral rupture from aberrant Foley catheter placement: a case report. J Radiol Case Rep. 2013;7:33–40. doi: 10.3941/jrcr.v7i1.1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Modi P.K., Salmasi A.H., Perlmutter M.A. Inadvertent foley catheterization of the ureter. Can J Urol. 2014;21:7326–7329. [PubMed] [Google Scholar]
- 17.Ishikawa T., Araki M., Hirata T., Watanabe M., Ebara S., Watanabe T. A rare complication: misdirection of an indwelling urethral catheter into the ureter. Acta Med Okayama. 2014;68:47–51. doi: 10.18926/AMO/52144. [DOI] [PubMed] [Google Scholar]
- 18.Viswanatha R.K., Moore C.M., Thakar R. Intra-ureteric placement of a urinary catheter in the previously undiagnosed duplex ureter. Int Urogynecol J. 2014;25:143–144. doi: 10.1007/s00192-013-2099-6. [DOI] [PubMed] [Google Scholar]


