Abstract
Purpose:
The aim is to evaluate the diagnostic accuracy of digital fundus photography in diabetic retinopathy (DR) screening at a single university hospital.
Methods:
This was a cross-sectional hospital-based study. One hundred and ninety-eight diabetic patients were recruited for comprehensive eye examination by two ophthalmologists. Five-field fundus photographs were taken with a digital, nonmydriatic fundus camera, and trained primary care physicians then graded the severity of DR present by single-field 45° and five-field fundus photography. Sensitivity and specificity of DR grading were reported using the findings from the ophthalmologists’ examinations as a gold standard.
Results:
When fundus photographs of the participants’ 363 eyes were analyzed for the presence of DR, there was substantial agreement between the two primary care physicians, κ = 0.6226 for single-field and 0.6939 for five-field photograph interpretation. The sensitivity and specificity of DR detection with single-field photographs were 70.7% (95% Confidence interval [CI]; 60.2%–79.7%) and 99.3% (95% CI; 97.4%–99.9%), respectively. Sensitivity and specificity for five-field photographs were 84.5% (95% CI; 75.8%–91.1%) and 98.6% (95% CI; 96.5%–99.6%), respectively. The receiver operating characteristic was 0.85 (0.80–0.90) for single-field photographs and 0.92 (0.88–0.95) for five-field photographs.
Conclusion:
The sensitivity and specificity of fundus photographs for DR detection by primary care physicians were acceptable. Single- and five-field digital fundus photography each represent a convenient screening tool with acceptable accuracy.
Keywords: Diabetic retinopathy, fundus camera, fundus photography, screening
Diabetic retinopathy (DR) is a common microvascular complication in diabetic patients. In Maha Sarakham province in the northeast of Thailand, the number of diabetic patients requiring medical assistance sometimes exceeds the number of available ophthalmologists. Although diabetic patients in a university hospital's contracting unit for primary care are registered on Maha Sarakham provincial public health office's health data center system, the rate of diabetic care access at the time of this study was just 46.94%.[1] Furthermore, the rate of DR screening was in danger of missing Thailand's Ministry of Public Health service plan targets, just 33.81% for this hospital and 1.35%–76.40% for the province as a whole.[1]
Since Thailand's Ministry of Public Health and Ministry of Education, initiated their collaborative project to increase rural doctors in 1995 and similar subsequent projects, the number of doctors per capita has steadily improved. In 2015, there was one doctor for every 2035 people.[2] Primary care physicians are therefore the prime movers for distributing health services in rural areas, including DR screening.
Many studies have reported the accuracy of different screening tools for DR. For example, the early treatment of DR Study (ETDRS) showed that seven-field 30° stereoscopic color fundus photography detects retinal lesions accurately,[3] but that it is time-consuming and dependent on patient cooperation. Single-field fundus photography is another method, one which is convenient and widely used for community screening. Single-field fundus photography can use 45°, 60°, or ultra-wide fields.[4,5,6,7] An important limitation with single-field photography, however, is that it is unable to detect peripheral lesions, and there is, therefore, a risk of DR progression.[6,8] Due to this, single-field fundus photography is not a substitute for a pupil-dilated comprehensive eye examination.[9,10] A novel method for detecting DR without pupillary dilatation has also been proposed, one using full-field flicker electroretinograph (ERG) as an adjunctive screening tool, but further studies are required to determine its accuracy in large populations.[11]
The study reports the accuracy of single- and five-field fundus photography following pupillary dilatation (which is practicable for patient instruction) for DR detection by trained primary care physicians. Slit lamp fundoscopy and indirect ophthalmoscopy-based diagnosis by qualified ophthalmologists was used as the gold standard.
Methods
Study design
This was a cross-sectional study, carried out between January and May 2017 at the ophthalmology clinic at a single university hospital. The study was approved by the ethics committee for research involving human subjects. All investigations were carried out in accordance with the tenets of the Declaration of Helsinki, and all participants gave informed written consent.
Participants
Participants were diabetic patients requiring DR screening who had been attending a noncommunicable diseases clinic, and who met the inclusion criteria of having received a diagnosis of diabetes from an internist. Patients were excluded if they generated a poor quality photograph (due to anterior segment ocular media opacity or a small pupil from any other cause), if the eyes had previously undergone retinal laser treatment, if there was missing data, if the patient rejected our request to be enrolled, if there was a physical limitation that prevented the patient undergoing an eye examination in a fully upright position, or if mydriatic drug use was contraindicated for the patient.
Data collection
Slit lamp biomicroscopy was done to evaluate the anterior segment and to assess the anterior chamber depth for safe dilatation of the pupils. Tetracaine hydrochloride 0.5% and tropicamide 1% were instilled in all cases for pupillary dilatation, and phenylephrine hydrochloride 10% in some indicated cases. After full pupillary dilatation, the type of cataract was graded. Retinal examination was performed by ophthalmologists through slit lamp fundoscopy using a noncontact slit lamp lens or through indirect ophthalmoscopy with a 20-diopter lens.
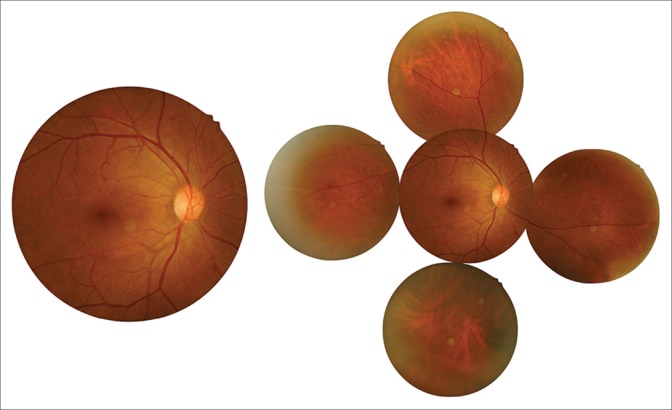
Posterior segment photography was also performed using a nonmydriatic, digital fundus camera (Kowa nonmyd alpha-DIII, Kowa Company Ltd., Tokyo, Japan) to obtain single-field central posterior 45° images (covered optic disc and macula), and the additional four fields (temporal, nasal, superior, and inferior) of both eyes [Fig. 1]. This was performed by well-trained nurse practitioners. The manual for DR retinograph interpretation was then used to instruct both of primary care physicians according to the International Council of Ophthalmology (ICO) Guidelines for Diabetic Eye Care developed by the ICO.[12] The severity of DR was classified according to the International Clinical DR Disease Severity Scale.[13] Photographs showing previous retinal laser treatment, poor quality photographs, and corrupted files were excluded from the study. Both primary care physicians were blinded to the gold standard results. The accuracy of fundus photograph interpretation was determined first for single-field central posterior 45° photography, then the additional four fields, using the Ophthamologists’ findings by mydriatic pupil examination as the gold standard.
Figure 1.
Fundus photographs of single-field central posterior 45° image (covered optic disc and macula) and the additional four fields
Data analysis and statistics
The presence or absence of DR was noted, and the degree of DR was graded. Clinically, significant macular edema (CSME) was defined as described in the ETDRS.[14] In cases where a fundus could not be evaluated, that eye was excluded from the study. Sensitivity and specificity were analyzed and reported in terms of the receiver operating characteristic (ROC) curve. The accuracy of primary care physician interpretations and inter-examiner variation in interpretations were assessed using Kappa coefficient agreement analysis. For DR grading and detection of CSME, P values are presented.
Results
Accuracy of fundus photograph interpretation
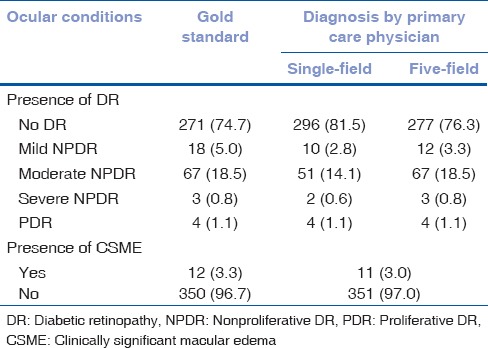
All eye photographs were included for accuracy analysis. Out of a total of 396 eyes (198 patients), one eye had to be excluded due to a dense cataract and obscured fundus evaluation. Of the remaining 395 eyes, 32 had to be excluded-20 due to poor photograph quality, 2 due to photograph loss and 10 due to previous retinal laser treatment. This left 363 fundus photographs available for grading. The prevalence of DR determined by ophthalmologist examination was 25.3% (92 eyes) −5.0% for mild nonproliferative DR (NPDR), 18.5% for moderate NPDR, 0.8% for severe NPDR, and 1.1% for (PDR) [Table 1].
Table 1.
Accuracy of single-field 45° and five-field fundus photography in detecting diabetic retinopathy, with examination by ophthalmologists used as the gold standard
Diagnostic characteristics for detecting diabetic retinopathy
Two primary care physicians (NW and PS) were provided with photographs from the ICO Guidelines for Diabetic Eye Care, and independently graded the severity of DR from the same computer with files of the same resolution. When findings of the two physicians were compared, the inter-rater validity showed substantial agreement. The Kappa statistic was 0.6226 (P < 0.001) for single-field and 0.6939 (P < 0.001) for five-field photographs interpretation. The main interpreter (NW) graded all photographs.
When the findings of the ophthalmologists’ retinal examination and the primary care physician's interpretations are compared, the sensitivity and specificity are respectively 70.7% (95% Confidence interval [CI]; 60.2%, 79.7%) and 99.3% (95% CI; 97.4%, 99.9%) for single-field interpretation, and 84.5% (95% CI; 75.8%, 91.1%) and 98.6% (95% CI; 96.5%, 99.6%) for five-field interpretation [Table 2].
Table 2.
Diagnostic characteristics for detecting any diabetic retinopathy and clinically significant macular edema
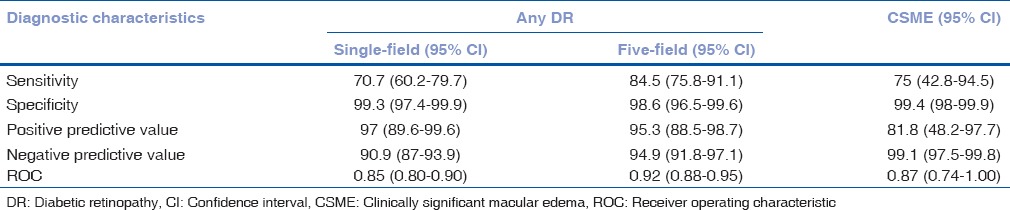
DR grade underestimates by the primary care physicians were attributable to some of the central 45° photographs not covering the peripheral retinal lesion. DR grade overestimates were due to drusen misinterpreted as hard exudate, microaneurysm misinterpreted as dot hemorrhage, or intraretinal hemorrhage from hypertensive retinopathy. Positive predictive values, negative predictive values, and ROC are shown in Table 2. For CSME detection, one eye was excluded due to unavailable results. The sensitivity and specificity of CSME detection are also shown in Table 2.
Discussion
This study has demonstrated that images obtained by single- and five-field fundus photography and interpreted by trained primary care physician is an accurate method for the detection of DR. The study results are in agreement with previous studies showing that single-field photograph interpretation is a convenient screening tool with acceptable results.[4,5] Misinterpreted images were mostly in the no DR, mild NPDR, and moderate NPDR groups. Five-field photography was more sensitive than single-field photography for DR detection as single-field images missed some of the peripheral retinal lesions and underestimated DR grade. Although single-field photography is a more convenient, more economical and less labor intensive screening method than five-field photography, it might, therefore, be inadequate in situations where lesions are peripherally located.[6,7,8,9] However, the single-field images of PDR cases in this study can be correctly diagnosed, because the distribution of neovascularization of the optic disc and neovascularization elsewhere were posteriorly located. It is also worth stating that the sensitivity determined for single-field interpretation in the present study might be higher than that achievable in clinical practice as photos were taken through mydriatic pupils.
We assigned primary care physicians as interpreters in this study so that accessibility to DR screening could be improved for diabetic patients resident in rural areas that lack ophthalmologists. Encouragingly, substantial agreement was achieved after testing for inter-rater reliability. However, instructions relating to potential angle closure examination for five-field mydriatic pupil image acquisition should be improved to increase screening sensitivity with safety performance.
The study has two important limitations. First, all of the images obtained were from mydriatic pupils so that we may have overestimated the sensitivity of these screening tests. Second, the results obtained were for just two primary care physicians, so inter-rater reliability may have been overestimated. The study finding that single- and five-field image interpretation generates accurate results is important as five-field image photography is less complicated for physicians requires less patient instruction and can be performed more quickly than standard seven-field image interpretation. Image enhancement and interpretation software might improve the accuracy of these screening methods further. The image transferring and registration systems could improve the quality of future diabetic care as well.
Conclusion
Single- and five-field fundus photograph interpretation by primary care physicians are two noninvasive screening methods for DR, each with acceptable accuracy and requiring minimal staff training. However, neither method is as accurate as a comprehensive pupil-dilated retinal examination by an ophthalmologist, and the latter method is preferable in some situations.
Financial support and sponsorship
Research grant from Mahasarakham University Faculty of Medicine.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ministry of Public Health. Health Data Center Report 2017. Thailand: Ministry of Public Health; 2017. [Last accessed on 2017 Jun 16]. Available from: http://www.mkm.hdc.moph.go.th/hdc . [Google Scholar]
- 2.National Economic and Social Development Board. Thailand: National Economic and Social Development Board; 2017. [Last accessed on 2017 Jun 16]. Available from: http://www.social.nesdb.go.th/SocialStat/StatSubDefault_Final.aspx?catid=3 . [Google Scholar]
- 3.Grading diabetic retinopathy from stereoscopic color fundus photographs – An extension of the modified Airlie House classification. ETDRS report number 10. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1991;98:786–806. [PubMed] [Google Scholar]
- 4.Ruamviboonsuk P, Wongcumchang N, Surawongsin P, Panyawatananukul E, Tiensuwan M. Screening for diabetic retinopathy in rural area using single-field, digital fundus images. J Med Assoc Thai. 2005;88:176–80. [PubMed] [Google Scholar]
- 5.Suansilpong A, Rawdaree P. Accuracy of single-field nonmydriatic digital fundus image in screening for diabetic retinopathy. J Med Assoc Thai. 2008;91:1397–403. [PubMed] [Google Scholar]
- 6.Silva PS, Cavallerano JD, Haddad NM, Kwak H, Dyer KH, Omar AF, et al. Peripheral lesions identified on ultrawide field imaging predict increased risk of diabetic retinopathy progression over 4 years. Ophthalmology. 2015;122:949–56. doi: 10.1016/j.ophtha.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 7.Møller F, Hansen M, Sjølie AK. Is one 60 degrees fundus photograph sufficient for screening of proliferative diabetic retinopathy? Diabetes Care. 2001;24:2083–5. doi: 10.2337/diacare.24.12.2083. [DOI] [PubMed] [Google Scholar]
- 8.Herbert HM, Jordan K, Flanagan DW. Is screening with digital imaging using one retinal view adequate? Eye (Lond) 2003;17:497–500. doi: 10.1038/sj.eye.6700409. [DOI] [PubMed] [Google Scholar]
- 9.Williams GA, Scott IU, Haller JA, Maguire AM, Marcus D, McDonald HR, et al. Single-field fundus photography for diabetic retinopathy screening: A report by the American Academy of Ophthalmology. Ophthalmology. 2004;111:1055–62. doi: 10.1016/j.ophtha.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 10.Moss SE, Meuer SM, Klein R, Hubbard LD, Brothers RJ, Klein BE, et al. Are seven standard photographic fields necessary for classification of diabetic retinopathy? Invest Ophthalmol Vis Sci. 1989;30:823–8. [PubMed] [Google Scholar]
- 11.Fukuo M, Kondo M, Hirose A, Fukushima H, Ikesugi K, Sugimoto M, et al. Screening for diabetic retinopathy using new mydriasis-free, full-field flicker ERG recording device. Sci Rep. 2016;6:36591. doi: 10.1038/srep36591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.International Council of Ophthalmology (ICO). ICO Guidelines for Diabetic Eye Care. 2017. [Last accessed on 2017 Jun 16]. Available from: http://www.icoph.org/resources/309/ICO-Guidelines-for-Diabetic-Eye-Care.html .
- 13.International Diabetes Federation. IDF Diabetes Atlas. 7th ed. Belgium: International Diabetes Federation; 2015. [PubMed] [Google Scholar]
- 14.Photocoagulation for diabetic macular edema. Early treatment diabetic retinopathy study report number 1. Early Treatment Diabetic Retinopathy Study Research Group. Arch Ophthalmol. 1985;103:1796–806. [PubMed] [Google Scholar]