Abstract
Background:
There currently are no data on the relative frequency of endoscopic sinus surgeries (ESS) performed for chronic rhinosinusitis with nasal polyposis (CRSwNP) versus chronic rhinosinusitis without nasal polyposis (CRSsNP) in the United States.
Objectives:
To compare the rate of surgical interventions for CRSwNP and CRSsNP.
Methods:
Cases identified by CPT codes were extracted from the 2009–2011 State Ambulatory Surgery Databases for California, Florida, Maryland, and New York. Patient demographics, extent of surgery, mean charges, and operating room (OR) time were compared.
Results:
A total of 97,228 ESS cases were performed in the four states; 29.3% of surgeries were for patients with CRSwNP, 66.0% of patients with CRSsNP, and 4.8% for other indications. The proportion of ESS for CRSwNP varied across states, with California having the highest percentage (34.6%) and Maryland having the lowest (26.4%) (p < 0.0001). Patients with Medicaid (33.8%) and Medicare (32.2%) had higher rates of surgery for CRSwNP compared with patients with private insurance (29.9%) (p < 0.001). Surgeons who performed a higher volume of sinus surgery compared to lower volume surgeons performed a lower percentage of surgery for CRSwNP (24.4 versus 33.5%; p < 0.001). ESS cases for CRSwNP were more extensive (relative risk of four sinus surgeries of 1.88; p < 0.0001), used image guidance more frequently (relative risk, 1.39; p < 0.0001), and were less likely to include a balloon procedure (relative risk, 0.69; p < 0.0001). Patients with CRSwNP had longer OR times (ESS that involved all four sinuses took 14 minutes longer) (p < 0.0001), but no difference in charges compared with patients with CRSsNP who underwent a similar extent of surgery.
Conclusion:
Almost 30% of ESS were performed for CRSwNP, and these cases were, on average, more extensive, used more OR time, and more often used image guidance than surgeries for CRSsNP. The rate of surgery performed for CRSwNP varied based on geography, payer, and surgical volume, which indicted that patient selection impacted surgical management.
Keywords: Chronic rhinosinusitis, chronic rhinosinusitis with nasal polyposis, endoscopic sinus surgery, state ambulatory surgery database, charges, image guidance, surgical volume
Chronic rhinosinusitis (CRS) is characterized by mucosal inflammation of the nose and paranasal sinuses, and is divided into two broad clinical categories: CRS with nasal polyposis (CRSwNP) and CRS without nasal polyposis (CRSsNP).1 The incidence of CRSwNP is approximately one-tenth of the incidence of CRSsNP.2 The prevalence of CRSwNP is ∼1%, whereas the prevalence of CRSsNP is less clear but estimated at approximately 10-fold higher.3 CRSwNP is also biologically different. In Western populations, CRSwNP is near uniformly an eosinophilic condition, whereas CRSsNP is more heterogeneous.4,5
In the United States, there currently are no data on the relative frequency of endoscopic sinus surgeries (ESS) performed for CRSwNP versus CRSsNP. Previous studies on CRSwNP demonstrate increased rates of revision surgery but also greater improvements after sinus surgery compared with patients with CRSsNP.6–11 Patients with CRSwNP may also have a higher risk of complications during surgery due to increased bleeding, decreased visualization, and altered anatomy.12–14
The objectives of this study were to (1) determine the percentage of surgeries performed for CRSwNP compared with CRSsNP in an administrative data base that records all ambulatory surgeries, (2) compare the demographic information of patients who underwent procedures performed for CRSwNP compared with CRSsNP, (3) determine the extent of surgical interventions commonly performed for the diagnosis of CRSwNP compared with CRSsNP, and (4) calculate the rate of complications and the mean charges and operating room (OR) times for procedures for patients with CRSwNP compared with those with CRSsNP.
METHODS
Data Source and Subjects
We used the State Ambulatory Surgery Database (SASD) of California, Florida, Maryland, and New York for 2009, 2010, and 2011. These states were selected to gain a wide geographic distribution.15,16 SASD is a product of the Healthcare Cost and Utilization Project (HCUP), conducted by the federal Agency for Healthcare Research and Quality, and the sources of the data are the specific states that submit data to HCUP.17 The data bases capture all hospital-based ambulatory surgery encounters in all four states and, in addition, all freestanding ambulatory surgery center encounters in Florida, California, and New York. Current Procedural and Terminology (CPT) codes for balloon or combined balloon and endoscopic dilation (BCD) were available beginning in 2011, therefore, only the 2011 data sets were used for analyses that compared BCD with traditional ESS.
Compilation of Analytic Data Set
We defined the study cohort from the state data files by using CPT codes. We extracted information of all patients with CPT codes for ESS (CPT 31233, 31235, 31254, 31255, 31256, 31267, 31276, 31287, 31288) and/or BCD (CPT 31295, 31296, 31297). Surgeries were deemed to be for CRSwNP if any one of the 20 codes in The International Classification of Diseases, Ninth Revision (ICD-9)18 was 471.X and for CRSsNP if the ICD-9 code was 473.X, and none of the codes were 471.X. We excluded patients <18 years of age and those who had surgery for and ICD-9 code other than 471.X or 473.X (n = 4619), which left 92,609 observations for demographic analyses.
To analyze total charges and OR time, we subset the data set to exclude patients who underwent procedures in addition to traditional ESS and/or BCD other than inferior turbinate, septoplasty, polypectomy, or concha bullosa procedures. When applying these criteria, 52,056 observations remained for total charge analysis, and 22,083 observations remained for OR time analysis (OR time data is only available for New York). We obtained estimates of the total populations of California, Florida, and New York from the U.S. Census Bureau July Intercensal Estimates.19,20
Covariate Factors
We obtained patient demographic information, including age, gender, race (white, black, Hispanic, Asian/Pacific Islander, or other), number of chronic diseases (0, 1–3, or ≥4), median income quartile of patients' (zip or other). We obtained surgery center information, including urban versus rural location and hospital based versus freestanding ambulatory surgery center. We calculated the volume of procedures performed at each surgical site and determined terciles for low- (≤52 procedures/y), medium- (52–122 procedures/y), and high-volume (≥123 procedures/y) surgery centers. Only Maryland and Florida included data regarding surgeon identifiers, and so, for these states, we also calculated the volume of procedures performed by individual surgeons and determined surgical volume terciles with an equal number of surgeons: low (≤15 procedures/y), medium (16–34 procedures/y) and high (≥35 procedures/y). We also defined a variable for the count of types of sinus procedures performed for each patient discharge.21 We defined the number of sinus procedures per case as the count of the sinuses operated on (range, 1–4). The SASD data set does not distinguish between uni- versus bilateral sinus procedures.21 For this reason, paired procedures (e.g., bilateral maxillary procedures) were only counted as a single procedure type.
Outcome Measures
Outcomes of length of stay and death during admission were obtained from the data set. Patients with retrobulbar hemorrhage were identified based on ICD-9 codes for orbital hemorrhage or edema (376.32 or 376.33), with cerebrospinal fluid (CSF) leak by ICD-9 codes for CSF leak 320.X or 349.81, or CPT codes for lumbar drain or skull base repair (31290, 31291, 61618, 61619, 62272), and with blood transfusion by CPT code 36430.22 To facilitate the comparison of the total charge and OR time, we created variables for mini-ESS (defined as a maxillary antrostomy either via endoscopic or balloon techniques and ethmoidectomy), and for pan-ESS (defined as maxillary antrostomy, sphenoidotomy, and frontal sinus exploration via endoscopic or balloon techniques and ethmoidectomy).
Other combinations of sinus procedures that would fall between mini-ESS and pan-ESS were included in an overall comparison. Of note, only the data set for New York contained information regarding OR time, defined as the total time actually in the OR, exclusive of preoperative (preparation) and postoperative (recovery) time. Maryland, New York, and Florida data sets included data on total charges. The total charges do not include professional fees and noncovered charges, and professional fees are removed from the total charge during HCUP processing.17 A single total charge value was reported by the surgical center without further itemization.
Statistical Analysis
We used t-tests for continuous variables and χ2 or Fisher exact tests for categorical variables to perform bivariate analyses of patient factors, surgery center factors and volume, surgeon case volume, types of procedure, and outcomes between the groups of the patients who underwent procedures for CRSwNP or CRSsNP. We used a Bonferroni multiple comparison correction for post hoc testing when the overall χ2 test was significant. The Poisson regression was used to compare the normalized rate of ESS between state adult populations for states that had both freestanding and hospital-based surgery center data. The normality of the distribution for total charges and OR time was tested by use of the Kolmogorov-Smirnov test statistic.
Because the total charge and OR time data (and the log of both) were not normally distributed, we used the Wilcoxon rank sum nonparametric test for bivariate analyses that assessed cost and OR time between the group of patients with or without polyps who underwent mini-ESS, pan-ESS, or any sinus procedure. We performed all data management and analyses by using SAS (SAS Institute Inc., Cary, NC). Statistical significance was determined at a two-tailed level of p < 0.05. The Northwestern University Institutional Review Board deemed this study of publicly available deidentified information exempt from human subject reviews.
RESULTS
In 2009–2011 in California, Florida, Maryland, and New York, 97,228 ESS were performed; 29.3% of surgeries were for patients with CRSwNP (ICD-9 471.X), 66.0% of cases were for patients with CRSsNP (ICD-9 473.X), and 4.8% were for other indications. A total of 92,609 balloon sinuplasties or ESS for CRSwNP or CRSsNP were performed at 859 facilities. Within the subset of patients from Florida and Maryland who had unique surgeon identifier codes, 1085 surgeons performed 36,438 sinus surgeries.
The demographics of patients who had surgery for CRSwNP compared with those who had surgery for CRSsNP are presented in Table 1. Patients who had surgery for CRSwNP were older by 2 years when mean ages were compared. Patients with CRSwNP were more likely to be men and to have their surgery in a hospital-based rather than a freestanding surgery center. There were global differences in age groups, race, number of chronic diseases, median household state income quartile for patient zip code, urban versus rural location of patient zip code, hospital volume, and state, but we did not perform specific tests between CRSwNP and CRSsNP groups for these variables.
Table 1.
Demographic data for cases performed on patients with a diagnosis of CRSwNP vs patients with a diagnosis of CRSsNP
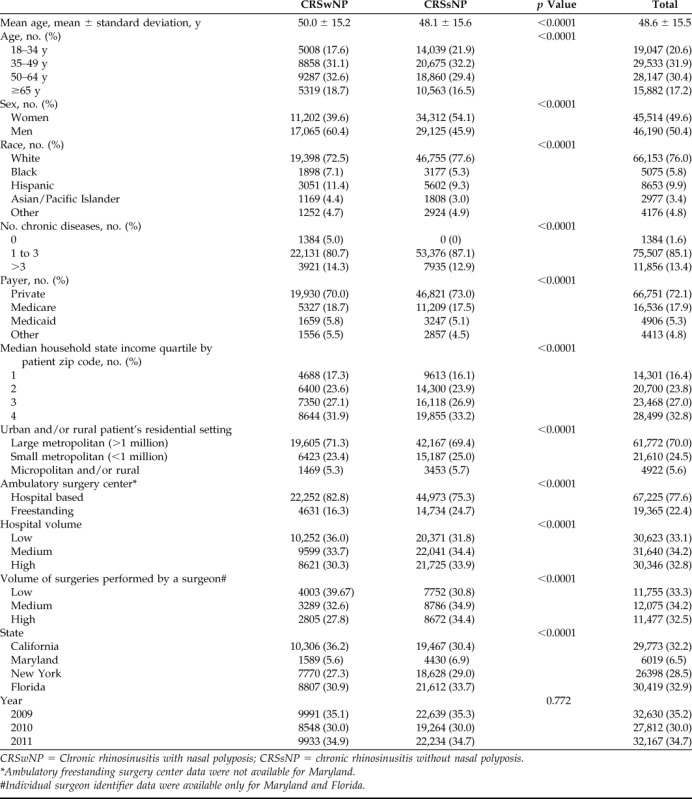
CRSwNP = Chronic rhinosinusitis with nasal polyposis; CRSsNP = chronic rhinosinusitis without nasal polyposis.
*Ambulatory freestanding surgery center data were not available for Maryland.
#Individual surgeon identifier data were available only for Maryland and Florida.
When adjusting for multiple comparisons, patients with Medicaid (33.8%) and Medicare (32.2%) had higher rates of surgery for CRSwNP compared with patients with private insurance (29.9%) (p < 0.001 for both). Also, surgeons who performed a higher volume of surgery compared to surgeons who performed a lower volume of surgery performed a lower percentage of surgery for CRSwNP (24.4 versus 33.5%; p < 0.001). The normalized rates of ESS were calculated based on state adult populations. California had a lower rate of ESS (35.4 ESS per 100,000 adults; p-value 0.027) compared with New York (58.3 ESS per 100,00 adults). Florida's (68.2 ESS per 100,000 adults; p-value 0.44) rate of surgery did not differ from that of New York (overall p < 0.001 for the Poisson regression).
The patients with CRSwNP had more extensive surgery and were more likely to have a pan-ESS, frontal sinus procedures, and image guidance (Table 2). For the patients with CRSwNP, the mean number of sinuses opened were 2.67 ± 1.04 and, for patients with CRSsNP, the mean number was 2.29 ± 0.98. Patients with CRSsNP had an increased rate of septoplasty compared with patients with CRSwNP (Table 2). In total, 8.25% of ESS cases for patients with CRSwNP or with CRSsNP had a balloon procedure performed in 2011. The patients with CRSwNP were less likely to have a balloon procedure compared with the patients with CRSsNP (Table 3).
Table 2.
Procedure types performed for patients with a diagnosis of CRSwNP vs patients with a diagnosis of CRSsNP
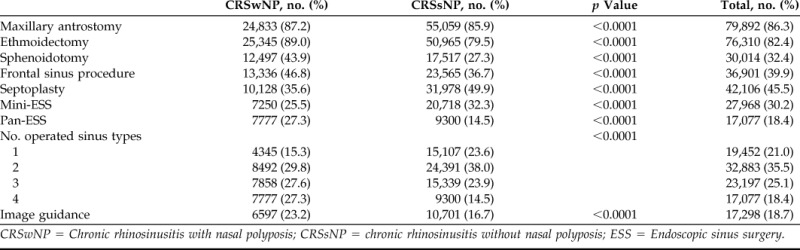
CRSwNP = Chronic rhinosinusitis with nasal polyposis; CRSsNP = chronic rhinosinusitis without nasal polyposis; ESS = Endoscopic sinus surgery.
Table 3.
Traditional endoscopic sinus surgery vs balloon or combined procedures performed for patients with a diagnosis of CRSwNP versus patients with a diagnosis of CRSsNP in 2011*
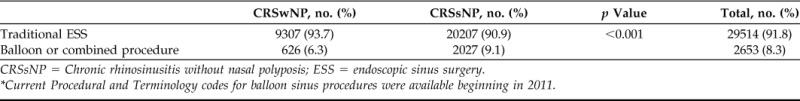
CRSsNP = Chronic rhinosinusitis without nasal polyposis; ESS = endoscopic sinus surgery.
Current Procedural and Terminology codes for balloon sinus procedures were available beginning in 2011.
There was no difference in the rates of CSF leak or blood transfusion during surgeries for patients with or without polyps. One patient died during the surgical admission, which was not statistically significant between the groups (p = 0.99, Fisher exact test). During the 3-year period, 0.01% of the patients had an orbital hemorrhage, and there was no significant difference between the groups (p = 0.68, Fisher exact test). The patients with CRSwNP were admitted for observation in 3.23% of surgeries compared with the patients with CRSsNP, who were admitted in 3.61% of surgeries (p = 0.02). Overall, the patients with CRSwNP had more extensive surgery and incurred higher total charges for their surgeries compared with the patients with CRSsNP. There was no difference in charges for patients with and those without polyps who had a mini-ESS or a pan-ESS procedure (Table 4). The patients with CRSwNP had significantly longer OR times (an average of 9 minutes longer for ESS of maxillary and anterior ethmoids, an average if 14 minutes longer for ESS that involved all four sinuses) compared with those with CRSsNP (Table 5).
Table 4.
The charges for procedures performed for patients with a diagnosis of CRSwNP vs patients with diagnosis of CRSsNP*
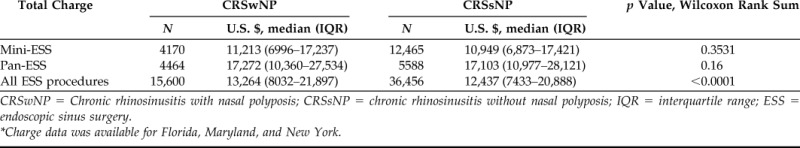
CRSwNP = Chronic rhinosinusitis with nasal polyposis; CRSsNP = chronic rhinosinusitis without nasal polyposis; IQR = interquartile range; ESS = endoscopic sinus surgery.
Charge data was available for Florida, Maryland, and New York.
Table 5.
The operating time for procedures performed for patients with a diagnosis of CRSwNP vs patients with a diagnosis of CRSsNP*
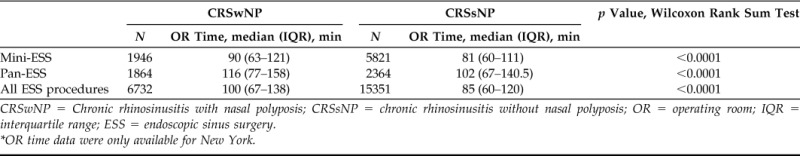
CRSwNP = Chronic rhinosinusitis with nasal polyposis; CRSsNP = chronic rhinosinusitis without nasal polyposis; OR = operating room; IQR = interquartile range; ESS = endoscopic sinus surgery.
OR time data were only available for New York.
DISCUSSION
This cross-sectional study examined data from four states, California, Florida, Maryland, and New York, for patients ≥18 years old who underwent endoscopic or balloon sinus surgery in 2009–2011 for the diagnosis of CRSwNP or CRSsNP. Overall, 92,609 surgeries were performed with 30.7% for patients with CRSwNP and 69.3% for patients with CRSsNP. The percentage of surgeries for CRSwNP varied across states, with California with the highest, at 34.6%; New York and Florida, both with 29%; and Maryland with the lowest, at 26.4%. In addition, California had an overall lower rate of ESS normalized to state adult populations compared with New York and Florida. Previous studies also noted geographic variations in the prevalence of CRS and the rate of ESS but have not reported on variations in sinus surgery based on polyposis.23–27
The rates of surgery for CRSwNP in the United States contrasts with a cross-sectional survey of 87 National Health System Hospitals in England and Wales in 2006, which found that 69.6% of ESS were for patients with polyposis compared with 30.4% of surgeries for patients without polyps.6 Although these differences may be due to geographic differences in environmental or genetic factors that lead to polyposis, they may also result from differential rates of surgery. For example, patients on Medicaid had significantly higher rates of surgery (33.8%) for CRSwNP compared with patients with private insurance (29.9%).
Interestingly, lower-volume surgeons performed a higher rate of surgery (33.5%) for CRSwNP compared with higher-volume surgeons (24.4%). This was similar to the study by Svider et al.,26 which found that the number of both endoscopic and open frontal cases billed per year had an inverse relationship with fellowship-trained rhinologists who practice in the area. The reason for these findings is unclear but may be because higher-volume surgeons can achieve a surgical competence with complicated CRSwNP cases and then need fewer revision surgeries.26 Our data set did not distinguish between revision and primary cases, and, therefore, further studies are necessary to determine how surgeon volume affects the timing and number of revision surgeries performed.
Similar to previous studies, patients with a diagnosis of CRSwNP were more likely to be older and to be men compared with those with CRSsNP.6,11,28–30 In a prospective study on the incidence of symptomatic CRSwNP, Larsen and Tos28 found an estimated incidence of 0.86 per thousand per year for men and 0.39 per thousand per year for women, which reached a peak with age of 1.68 and 0.82 patients per thousand per year, respectively, among those 50–59 years. In the cross-sectional study of 1 year of sinus surgery in England discussed above, two-thirds of all patients who underwent polypectomy were men compared with fewer than half of patients who underwent surgery for CRS, and the mean age in years for patients with nasal polyps was 51.6 years compared with 44.6 years old for patients without polyps.6 Similarly, Tan et al.29 examined a large cohort of the primary care patients over a 10-year period and found that 54% of the patients diagnosed with CRSwNP were men compared with 41.8% of the patients diagnosed with CRSsNP.
The patients with CRSwNP were more likely to undergo an extensive surgery that involved image guidance compared with those with CRSsNP. Patients with CRSwNP generally have more extensive disease with higher Lund-Mackay scores that are correlated with eosinophilia, although they have similar health utility.31,32 Surgical techniques for CRSwNP range from simple polypectomy to extensive surgery with mega maxillary antrostomies and removal of the middle turbinates, and there currently is insufficient evidence to define the optimal timing and extent of surgery.33 Although patients with CRSwNP were less likely than patients with CRSsNP to have a balloon device used during their surgery, 6% of patients with CRSwNP did have a balloon device used during their surgery to open one or more sinuses.
There is a significant enrichment of CRSwNP in surgically managed CRS compared with the incidence of patients with CRSwNP. For example, Tan et al.29 found that, in a cohort of primary care patients, the average incidence of CRSwNP was ∼83 cases per 100,000 person-years and of CRSsNP was ∼1048 cases per 100,000 person-years. Therefore, the incidence of CRSwNP was less than one-tenth the incidence of CRSsNP, yet patients with CRSwNP accounted for 30% of all ESS cases in our sample. This would indicate that patients with CRSwNP are more likely to need surgical intervention or need it more often.
We found no difference in the rates of transfusion, CSF leak, and orbital hemorrhage between surgeries for patients with CRSwNP compared with patients with CRSsNP. However, this study was underpowered to detect differences in complication rates. The rate of CSF leak was 0.09%, whereas the rate of orbital hemorrhage was 0.01% and transfusion was 0.02%. The rates of complications were lower than those reported in the audit of sinus surgery at National Health System Hospitals published in 2006, and with a systematic review that reported orbital and/or periorbital hemorrhage rates of 0.15%, transfusion rates of 0.2%, and CSF leakage rate of 0.3%.6,33,34
However, our data only captured complications during the perioperative admission and, therefore, were most likely an understatement of postoperative complications during a longer time course. Previous studies found that nasal polyposis is a risk factor for surgical complications.12–14 Due to the limitations of the data set, we were only able to analyze major complications with specific diagnosis codes that occurred at the time of surgery and were not able to analyze minor complications such as epistaxis or longer-term complications such as readmission, synechiae formation, and stenosis.
Procedures for patients with nasal polyposis, overall, were more expensive, most likely due to more extensive surgery because there was no difference in cost when similar surgeries were compared. Patients with CRSwNP had significantly longer OR times compared with those with CRSsNP, even when similar extents of surgery were compared. The longer OR time was most likely due to increased burden of disease, increased bleeding, and decreased visualization during surgery for CRSwNP compared with CRSsNP, as previously documented.34–36
Our study faced many of the challenges associated with analyzing administrative data. There was a disparity in the collected variables across states. There were limitations with using CPT codes to identify cases and with ICD-9 codes to determine diagnosis because it was not possible to know the exact indications for surgery because they are not explicitly linked in the data set.37 The data set also does not provide any information regarding the burden of disease, such as the 22-item Sino-Nasal Outcome Test scores or the Lund-Mackay scores. As with all studies that used administrative data bases, this study was dependent on the accuracy of the coding of the surgical procedure. Another limitation of the data set was the lack of cost to charge conversion and so the data represented how much the surgical centers charge but not what they were paid (charge data in SASD also do not include professional fees).
CONCLUSION
Approximately 30% of all ESS in the four states studied were performed for patients with polyps. The rate of surgery for CRSwNP varied across states, with California the highest and Maryland the lowest. Cases for patients with CRSwNP on average were more extensive and used greater resources than those for patients without polyps. Rates of surgery performed for CRSwNP varied based on geography, payer, and surgical volume. Further studies may determine whether patient selection impacts surgical management at the national level.
Footnotes
Podium presentation, Triological Combined Sections meeting, New Orleans, Louisiana, January 19–21, 2017
B.K. Tan is supported by National Institutes of Health grant K23DC012067. S.S. Smith is supported by the Northwestern University—Patient-centered Intervention and Engagement Training K12 Faculty Scholars Training Program (K12HS023011) and Chronic Rhinosinusitis Integrative Studies Program (U19 AI106683)
The authors have no conflicts of interest to declare pertaining to this article
REFERENCES
- 1. Chaaban MR, Walsh EM, Woodworth BA. Epidemiology and differential diagnosis of nasal polyps. Am J Rhinol Allergy. 2013; 27:473–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tan BK, Chandra RK, Pollak J, et al. Incidence and associated premorbid diagnoses of patients with chronic rhinosinusitis. J Allergy Clin Immunol. 2013; 131:1350–1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hulse KE, Stevens WW, Tan BK, Schleimer RP. Pathogenesis of nasal polyposis. Clin Exp Allergy. 2015; 45:328–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tan BK, Klingler AI, Poposki JA, et al. Heterogeneous inflammatory patterns in chronic rhinosinusitis without nasal polyps in Chicago, Illinois. J Allergy Clin Immunol. 2016; 139:699–703.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wang X, Zhang N, Bo M, et al. Diversity of TH cytokine profiles in patients with chronic rhinosinusitis: A multicenter study in Europe, Asia, and Oceania. J Allergy Clin Immunol. 2016; 138:1344–1353. [DOI] [PubMed] [Google Scholar]
- 6. Hopkins C, Browne JP, Slack R, et al. The national comparative audit of surgery for nasal polyposis and chronic rhinosinusitis. Clin Otolaryngol. 2006; 31:390–398. [DOI] [PubMed] [Google Scholar]
- 7. Smith TL, Mendolia-Loffredo S, Loehrl TA, et al. Predictive factors and outcomes in endoscopic sinus surgery for chronic rhinosinusitis. Laryngoscope. 2005; 115:2199–2205. [DOI] [PubMed] [Google Scholar]
- 8. Georgalas C, Cornet M, Adriaensen G, et al. Evidence-based surgery for chronic rhinosinusitis with and without nasal polyps. Curr Allergy Asthma Rep. 2014; 14:427. [DOI] [PubMed] [Google Scholar]
- 9. Poetker DM, Mendolia-Loffredo S, Smith TL. Outcomes of endoscopic sinus surgery for chronic rhinosinusitis associated with sinonasal polyposis. Am J Rhinol. 2007; 21:84–88. [DOI] [PubMed] [Google Scholar]
- 10. Wynn R, Har-El G. Recurrence rates after endoscopic sinus surgery for massive sinus polyposis. Laryngoscope. 2004; 114:811–813. [DOI] [PubMed] [Google Scholar]
- 11. Fokkens WJ, Lund VJ, Mullol J, et al. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology. 2012; 50:1–12. [DOI] [PubMed] [Google Scholar]
- 12. Hopkins C, Browne JP, Slack R, et al. Complications of surgery for nasal polyposis and chronic rhinosinusitis: The results of a national audit in England and Wales. Laryngoscope. 2006; 116:1494–1499. [DOI] [PubMed] [Google Scholar]
- 13. Stankiewicz JA, Lal D, Connor M, Welch K. Complications in endoscopic sinus surgery for chronic rhinosinusitis: A 25-year experience. Laryngoscope. 2011; 121:2684–2701. [DOI] [PubMed] [Google Scholar]
- 14. Asaka D, Nakayama T, Hama T, et al. Risk factors for complications of endoscopic sinus surgery for chronic rhinosinusitis. Am J Rhinol Allergy. 2012; 26:61–64. [DOI] [PubMed] [Google Scholar]
- 15. Ference EH, Graber M, Conley D, et al. Operative utilization of balloon versus traditional endoscopic sinus surgery. Laryngoscope. 2015; 125:49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ference EH, Schroeder JW, Jr, Qureshi H, et al. Current utilization of balloon dilation versus endoscopic techniques in pediatric sinus surgery. Otolaryngol Head Neck Surg. 2014; 151:852–860. [DOI] [PubMed] [Google Scholar]
- 17. SASD Database Documentation. Available online at http://www.hcup-us.ahrq.gov/db/state/sasddbdocumentation.jsp; accessed January 9, 2017.
- 18. Medicode (Firm). ICD-9-CM: International classification of diseases, 9th revision, clinical modification. Salt Lake City, Utah: Medicode; 1996. [Google Scholar]
- 19. United States Census Bureau. State Population by Characteristics Tables: 2010–2015. Available online at https://www.census.gov/data/tables/2016/demo/popest/state-total.html; accessed January 9, 2017.
- 20. United States Census Bureau. State Intercensal Estimates (2000–2010). 2012. Available online at https://www.census.gov/popest/data/intercensal/state/state2010.html; accessed January 9, 2017.
- 21. Pynnonen MA, Davis MM. Extent of sinus surgery, 2000 to 2009: A population-based study. Laryngoscope. 2014; 12:820–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ramakrishnan VR, Kingdom TT, Nayak JV, Hwang PH, Orlandi RR. Nationwide incidence of major complications in endoscopic sinus surgery. Int Forum Allergy Rhinol. 2012; 2:34–39. [DOI] [PubMed] [Google Scholar]
- 23. Rudmik L, Holy CE, Smith TL. Geographic variation of endoscopic sinus surgery in the United States. Laryngoscope. 2015; 125:1772–1778. [DOI] [PubMed] [Google Scholar]
- 24. Venkatraman G, Likosky DS, Morrison D, Zhou W, Finlayson SRG, Goodman DC. Small area variation in endoscopic sinus surgery rates among the Medicare population. Arch Otolaryngol Neck Surg. 2011; 137:253–257. [DOI] [PubMed] [Google Scholar]
- 25. Venkatraman G, Likosky DS, Zhou W, Finlayson SR, Goodman DC. Trends in endoscopic sinus surgery rates in the Medicare population. Arch Otolaryngol Head Neck Surg. 2010; 136:426–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Svider PF, Sekhsaria V, Cohen DS, Eloy JA, Setzen M, Folbe AJ. Geographic and temporal trends in frontal sinus surgery. Int Forum Allergy Rhinol. 2015; 5:46–54. [DOI] [PubMed] [Google Scholar]
- 27. DeConde AS, Soler ZM. Chronic rhinosinusitis: Epidemiology and burden of disease. Am J Rhinol Allergy. 2016; 30:134–139. [DOI] [PubMed] [Google Scholar]
- 28. Larsen K, Tos M. The estimated incidence of symptomatic nasal polyps. Acta Otolaryngol. 2002; 122:179–182. [DOI] [PubMed] [Google Scholar]
- 29. Tan BK, Chandra RK, Pollak J, et al. Incidence and associated premorbid diagnoses of patients with chronic rhinosinusitis. J Allergy Clin Immunol. 2013; 131:1350–1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Busaba NY, Sin HJ, Salman SD. Impact of gender on clinical presentation of chronic rhinosinusitis with and without polyposis. J Laryngol Otol. 2008; 122:1180–1184. [DOI] [PubMed] [Google Scholar]
- 31. Min JY, Ocampo CJ, Stevens WW, et al. Proton pump inhibitors decrease eotaxin-3/CCL26 expression in patients with chronic rhinosinusitis with nasal polyps: Possible role of the nongastric H,K-ATPase. J Allergy Clin Immunol. 2017; 139:130–141.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ference EH, Stubbs V, Lidder AK, et al. Measurement and comparison of health utility assessments in chronic rhinosinusitis. Int Forum Allergy Rhinol. 2015; 5:929–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Dessouky O, Hopkins C. Surgical versus medical interventions in CRS and nasal polyps: Comparative evidence between medical and surgical efficacy. Curr Allergy Asthma Rep. 2015; 15:66. [DOI] [PubMed] [Google Scholar]
- 34. Dalziel K, Stein K, Round A, et al. Endoscopic sinus surgery for the excision of nasal polyps: A systematic review of safety and effectiveness. Am J Rhinol. 2006; 20:506–519. [DOI] [PubMed] [Google Scholar]
- 35. Georgalas C, Cornet M, Adriaensen G, et al. Evidence-based surgery for chronic rhinosinusitis with and without nasal polyps. Curr Allergy Asthma Rep. 2014; 14:427. [DOI] [PubMed] [Google Scholar]
- 36. Ko MT, Chuang KC, Su CY. Multiple analyses of factors related to intraoperative blood loss and the role of reverse Trendelenburg position in endoscopic sinus surgery. Laryngoscope. 2008; 118:1687–1691. [DOI] [PubMed] [Google Scholar]
- 37. Lui JT, Rudmik L. Case definitions for chronic rhinosinusitis in administrative data: A systematic review. Am J Rhinol Allergy. 2015; 29:e146–e151. [DOI] [PubMed] [Google Scholar]


