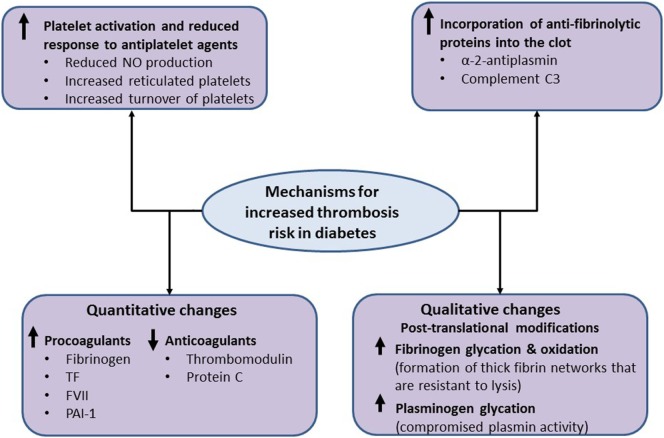
Figure 3.
Mechanistic pathways for increased thrombosis risk in diabetes. The metabolic changes in diabetes are associated with increased platelet activation, secondary to reduced nitric oxide (NO) production, an increase in reticulated platelets and increased platelet turnover, which can be only partially controlled by antiplatelet therapy. Diabetes is also associated with increased plasma levels of procoagulants and the antifibrinolytic protein levels, including fibrinogen, tissue factor (TF), factor VII (FVII), and plasminogen activator inhibitor-1 (PAI-1) as well as decreased levels of anticoagulants, including thrombomodulin and protein C. Moreover, qualitative changes in coagulation proteins, including increased oxidation and glycation of fibrinogen, have also been reported in diabetes, which result in the formation of thick fibrin networks that are resistant to lysis. Increased glycation of plasminogen compromises conversion to plasmin and alters protein activity. Finally, increased incorporation of antifibrinolytic proteins, such as α 2-antiplasmin and complement C3, into the clot impairs fibrinolysis and may represent a new therapeutic approach to reduce thrombosis risk in diabetes.