Abstract
Objectives
To assess the feasibility and acceptability of a mindfulness-based stress reduction (MBSR)-based intervention and determine if the intervention is associated with a significant signal on empathy and emotional competencies.
Design
Two pre–post proof-of-concept studies.
Setting
Participants were recruited at the University of Montreal’s Psychology Department (Study 1) and the CHU Sainte-Justine Department of Hematology-Oncology (Study 2).
Participants
Study 1: 12 students completed the 8-week programme (mean age 24, range 18–34). Study 2: 25 professionals completed the 8-week programme (mean age 48, range 27–63).
Intervention
Standard MBSR programme including 8-week mindfulness programme consisting of 8 consecutive weekly 2-hour sessions and a full-day silent retreat.
Outcomes measures
Mindfulness as measured by the Mindful Attention Awareness Scale; empathy as measured by the Interpersonal Reactivity Index (IRI)’s Perspective Taking and Empathic Concern subscales; identification of one’s own emotions and those of others as measured by the Profile of Emotional Competence (PEC)’s Identify my Emotions and Identify Others’ Emotions subscales; emotional acceptance as measured by the Acceptance and Action Questionnaire-II (AAQ-II) and the Emotion Regulation Scale (ERQ)’s Expressive Suppression subscale; and recognition of emotions in others as measured by the Geneva Emotion Recognition Test (GERT).
Results
In both studies, retention rates (80%–81%) were acceptable. Participants who completed the programme improved on all measures except the PEC’s Identify Others’ Emotions and the IRI’s Empathic Concern (Cohen’s d median=0.92, range 45–1.72). In Study 2, favourable effects associated with the programme were maintained over 3 months on the PEC’s Identify my Emotions, the AAQ-II, the ERQ’s Expressive Suppression and the GERT.
Conclusions
The programme was feasible and acceptable. It was associated with a significant signal on the following outcomes: perspective taking, the identification of one’s own emotions and emotional acceptance, thus, justifying moving towards efficacy trials using these outcomes.
Keywords: mindfulness-based stress reduction, haematology-oncology, empathy, emotional competence, profesional caregivers
Strengths and limitations of this study.
Two feasibility studies of a mindfulness-based stress reduction (MBSR)-based intervention in students and professionals had high attendance rates and acceptability levels.
Results suggested a significant clinical signal on most measured outcomes in the domains of emotion regulation and empathy, with effects lasting at follow-up for identification of one’s own emotions and emotional acceptance.
The same pattern of results was obtained in two independent small-scale studies.
A limitation to theses studies is that samples were not randomly selected, had limited size, and no control groups were used.
Another limitation is that most outcomes were self-reported and could be subject to desirability bias.
Introduction
In professional caregivers, empathy and its related emotional processes have been recognised as being of utmost importance.1 Empathy has been described as a multidimensional construct that encompasses the ability to cognitively adopt another person’s point of view (perspective taking; PT) and the tendency to experience other-oriented feelings such as compassion and concern (empathic concern; EC).2 A recent meta-analysis suggested that the professional–patient relationship impacts healthcare outcomes.3 Higher empathy would relate to better health outcomes in patients, including a reduction in the duration and severity of minor conditions, improved adherence to treatment, higher patient satisfaction and lower psychological distress.4–7 In professionals themselves, experimental research from social neuroscience has confirmed the long-standing clinical assumption that difficulty maintaining an adequate emotional distance from the suffering of patients could lead to emotional exhaustion, the latter being a core component of burnout.8 Research has also shown that sharing emotions without regulating effectively one’s emotions could lead to a reduced empathy.9 Abilities to regulate one’s emotions and empathy are all the more important in the context of serious paediatric conditions where professionals are even more likely to develop burnout and exhaustion.10–14
Emotional competencies are particularly important in a context where being empathetic could have an emotional cost to professional caregivers.15 To avoid emotional confusion, it is essential that professionals distinguish between their own emotions and their patient’s emotions.16 This is based on an adequate identification of one’s own emotions and the emotions of others (ie, identifying the agent of the emotional experience).17 An important skill allowing adequate identification of the source of emotion is to accept emotions as they arise rather than trying to avoid or suppress them. In this context, three key emotional competencies have been identified as core to empathic processes: (1) identifying one’s own emotions, (2) identifying the emotions in others and (3) accepting one’s own emotions.
Mindfulness-based interventions, including mindfulness-based stress reduction (MBSR), are deemed to promote a better awareness and acceptance of emotions as they occur and therefore could help develop emotional competencies in professional caregivers.18 However, despite the importance of empathy in healthcare and the suggested capacity of mindfulness practice to increase empathy and its related emotional competencies, these have seldom been selected as primary or secondary outcomes in previous studies.19 20 We conducted two inter-related studies to test for the effect of mindfulness on these outcomes in a population of professionals vulnerable to burnout.
The first objective of the studies was to determine if an MBSR-derived programme was a feasible and acceptable intervention for students and professional caregivers working in a tertiary paediatric haematology–oncology treatment centre. The second objective was to determine if the programme could achieve a significant clinical signal on empathy and the following emotional competencies: identification of one’s own emotions, identification of others’ emotions and emotional acceptance.
Methods
Design
As recommended in existing programme development methodological guidelines when examining new outcomes of a manualised intervention, we performed two phase IIa proof-of-concept studies focusing on feasibility and clinical signals on the new domains in an original population.21 The first study was used to set up the programme and the modalities for data collection in a student population; the second was designed to replicate the first in a professional setting, to extend it to a larger scale and to include a follow-up. Both studies were designed as one-group pretest–post-test studies to inform future trials. Measures were taken at pre and post for Study 1 and at pre, post and a 3-month follow-up for Study 2.
Participants and procedure
Study 1 took place between October 2015 and March 2016 at the University of Montreal and involved university psychology students. Study 2 took place at the CHU Sainte-Justine Department of Hematology-Oncology (Montreal, Canada) from March to May 2016 and involved professional caregivers working in paediatric haematology–oncology. Inclusion criteria for both studies were: (1) the ability to comply with the requirements of the programme, (2) no previous participation in MBSR, (3) no active substance dependence, (4) no psychotic symptoms and (5) no suicidality.
Study 1
Participants were recruited at the University of Montreal Psychology Department. All psychology undergraduate and graduate students (n=1130) were approached via email to participate in this 8-week stress reduction programme.
Study 2
Participants of Study 2 were recruited among day shift professional caregivers and employees working at the CHU Sainte-Justine Department of Hematology-Oncology (n=109). Potential participants were invited to an information meeting. The instructor (ML) met participants who were interested individually.
Participants gave written informed consent before the beginning of the study. They received $C50 for the completion of the programme and the surveys.
Intervention
The Pleine conscience, Empathie, Acceptation et Compétences Émotionnelles (PEACE) programme was modelled on MBSR developed by Kabat-Zinn18 which had already been tested in paediatric haematology–oncology (but with other outcomes).22 The intervention consisted of 8 weekly 2-hour sessions and a full-day silent retreat between sessions 6 and 7. Participants received a workbook and audio recordings of guided meditations to help them with home practice (see online supplementary file 1 for a transcript from an audio recording distributed to participants). The intervention was led by an instructor with extended meditation practice and training in MBSR at the University of Massachusetts Medical School (ML). To ensure the integrity of the programme, the instructor was supervised by a certified MBSR instructor, a pioneer in the field with more than a decade of experience teaching MBSR to caregivers in Canada and Europe (PD, see Acknowledgements section). All sessions were videotaped for that purpose.
bmjopen-2017-018421supp001.pdf (310.4KB, pdf)
Feasibility and acceptability
We assessed the feasibility of conducting an 8-week mindfulness-based programme with professionals working in paediatric haematology–oncology by evaluating their interest in the programme, the retention rates and adherence to practice. The interest in the programme was measured by the proportion of professionals interested among those meeting the eligibility criteria. The retention rate was measured by the proportion of professionals enrolled in the study who completed the study protocol (at least 6 of the 8 weekly sessions). The adherence to practice was estimated by the number of hours of home practice as recorded by the participants, including formal practice (ie, yoga, meditation, body scan, walking meditation) and informal practice (eg, being mindful while performing daily tasks such as brushing one’s teeth).
We also included three open-ended evaluation questions in the poststudy questionnaire to explore the acceptability of the programme: (1) ‘What is your general appreciation of the programme?’, (2) ‘What are the obstacles you have encountered during the programme?’ and (3) ‘What did you learn from your participation in the programme?’ In addition, in the prestudy questionnaire, participants were asked to set three personal goals for the programme. In the poststudy questionnaire, they were asked whether the programme had helped them achieve these goals.
Measures
At all time points, participants completed validated French-language versions of self-report questionnaires electronically via SurveyMonkey. They also completed an emotion recognition task23 online via the survey tool of the Qualtrics Research Suite (2016 Qualtrics, Provo, Utah, USA).
Mindfulness
The Mindful Attention Awareness Scale (MAAS)24 was used to measure mindfulness. The MAAS is a validated 15-item questionnaire that measures attention to and awareness of the present moment on a 6-point Likert scale (1=almost always; 6=almost never).24 25 The total score is the mean of the items (range 1–6). An example of an item is: ‘I do jobs or tasks automatically, without being aware of what I’m doing’. The internal consistency coefficient for both Study 1 and Study 2 was α=0.84.
Empathy
Empathy was measured with the Interpersonal Reactivity Index (IRI),26 a 28-item answered on a 5-point Likert scale (0=does not describe me well, 4=describes me very well). Two subscales of the IRI were used for this study (seven items each): the PT subscale, which measures the tendency to adopt others’ viewpoints (cognitive empathy); and the EC subscale, which measures the tendency to feel warmth, concern and compassion for others (emotional empathy). The score of each subscale is the sum of the items (range 0–28). An example of a PT item is: ‘When I’m upset at someone, I usually try to ‘put myself in his shoes’ for a while’. An example of an EC item is: ‘I often have tender, concerned feelings for people less fortunate than me’. In Study 1, the Cronbach alphas were 0.67 for PT and 0.75 for EC; in Study 2, the Cronbach alphas were 0.75 for PT and 0.73 for EC.
Emotional competencies
Identification of one’s own emotions: Identification of one’s own emotions was measured with the Profile of Emotional Competence (PEC),27 which measures emotional competencies on a 5-point Likert scale (1=not at all/never; 5=very well/often). We used the 5-item subscale ‘Identify my Emotions’. The score of the subscale is the mean of the items (range 1–5). An example of the items includes: ‘I am aware of my emotions as soon as they arise’. The subscale’s Cronbach alphas for Study 1 and Study 2 were 0.81 and 0.54, respectively.
Identification of emotions in others: Identification of emotions in others was measured with the PEC’s 5-item subscale ‘Identify Others’ Emotions’.27 The score of the subscale is the mean of the items (range 1–5). An example of an item is:‘I am good at sensing what others are feeling’. The subscale’s Cronbach alphas for Study 1 and Study 2 were 0.84 and 0.67, respectively.
Emotional acceptance: Emotional acceptance was measured with the Acceptance and Action Questionnaire-II, a 10-item questionnaire using a 7-point Likert scale (1=never true, 7=always true).28 The scale measures experiential avoidance; items were reversed to obtain a measure of acceptance. The score of the scale is the sum of the items (range 10–70). An example of an item is: ‘I’m afraid of my feelings’. The Cronbach alphas for Study 1 and Study 2 were 0.91 and 0.79, respectively.
We also used the Emotion Regulation Scale,29 a 7-item questionnaire using a 7-point Likert scale (1=strongly agree, 7=strongly disagree) to assess the suppression of emotions (4-item Expressive Suppression subscale), reflecting less emotional acceptance. The score of the 4-item subscale is the mean of the items (range 1–7). An example of an item is: ‘I control my emotions by not expressing them’. The subscale’s Cronbach alphas for Study 1 and Study 2 were 0.67 and 0.84, respectively.
Recognition of others’ emotions task
The Geneva Emotion Recognition Test (GERT)23 was used to measure the participants’ ability to recognise emotions in others. This is a facial emotion recognition task consisting of 83 short videos (with audio recordings) in which actors express 14 different emotions. The task can be completed in approximately 20 min (10 min for the short version). After each video, participants had to choose which emotion was expressed by the actor on the video. The full 83-item GERT was used for Study 1 and due to time concerns the short 42-item version (GERT-S) was used for Study 2.30 The score is the sum of the items (range 0–83 for the GERT and 0–42 for the GERT-S).
Statistical analysis
Descriptive statistics were used to describe sociodemographic characteristics of the samples. We performed Student’s t-tests to compare baseline scores of participants in Study 1 with those of participants in Study 2. For Study 1, we performed Student’s t-tests to compare pre/post differences. For Study 2, we performed General Linear Models with three levels (pre, post, follow-up) that included a Mauchly’s test of sphericity. A Greenhouse-Geisser correction was used when the assumption of sphericity was violated. Pairwise comparisons were performed with a Bonferroni correction for multiple comparisons. Statistical significance was established at P<0.05. In line with our objectives, we computed Cohen’s d to assess effect sizes for pre/post, post/follow-up and pre/follow-up differences. Statistical analyses were performed with IBM SPSS Statistics, V.24.0.
Results
Participants
Participants’ demographic characteristics for both studies are shown in table 1. The mean (SD) number of hours of formal practice at home for the entire programme was on average 9.8 (6.2) for Study 1 and 24.9 (12.9) for Study 2. Hours of informal practice were on average 2.5 (1.8) for Study 1 and 11.4 (15.3) for Study 2.
Table 1.
Characteristics of participants
| Study 1 (Students, n=12) |
Study 2 (Professionals, n=25) |
|
| n (%)/M (SD) | n (%)/M (SD) | |
| Sex | ||
| Female | 11 (92%) | 22 (88%) |
| Male | 1 | 3 |
| Age | 24.0 (4.2) range 18–34 |
48.1 (10.8) range 27–63 |
| Marital status | ||
| Married, civil union, common law | 5 (42%) | 12 (48%) |
| Living alone | 7 (58%) | 13 (52%) |
| University level (Study 1)/level of education (Study 2) | ||
| College | – | 3 (12%) |
| Bachelor | 7 (58) | 12 (48%) |
| Master | – | 6 (24%) |
| Doctorate | 5 (42) | 4 (16%) |
| Profession (Study 2) | ||
| Nurse | – | 13 (52%) |
| Physician | – | 2 (8%) |
| Professionals* | – | 4 (16%) |
| Support staff† | – | 6 (24%) |
*Two physiotherapists and two supportive care professionals.
†Four research staff and two community organisation professionals.
Feasibility and acceptability
Study 1
Forty-three students showed interest in participating in the study. Sixteen were interviewed and screened for eligibility, with 15 recruited to take part in the study. Among these, 12/15 completed at least six sessions, yielding a retention rate of 80%. Furthermore, 15/15 (100%) completed the preintervention survey, 12/15 (80%) completed the postsurvey and 11/12 (92%) attended the 1-day silent retreat. Three students (20%) left the programme (two after the first session for personal reasons and one after the fourth session due to a scheduling conflict). The final sample for analyses was thus composed of 12 students.
Postintervention data indicated high levels of satisfaction with the PEACE programme. Thus, 11/12 (92%) reported that the programme had helped them achieve the goals they had set for themselves and 12/12 (100%) reported that the programme made them more aware of their experience of the present moment. Participants reported that the programme was (1) ‘varied’, (2) ‘structured’, (3) ‘instructive’ and (4) ‘beneficial’. Participants’ comments were positive regarding their overall appreciation of the programme (eg, ‘I did it to sleep better and it worked’, ‘This program helped me improve my stress management skills and I want to continue meditating’). Students reported that they had learned from the programme (eg, ‘I learned that it’s very important to take time for myself’). The most frequent obstacles reported by the students were as follows: (1) ‘the length of the daily home practice’, (2) ‘lack of assiduity’, (3) ‘difficulty finding time for home practice’, (4) ‘motivation for home practice’ and (5) ‘sleepiness during the exercises’.
Study 2
Forty-one out of 109 (38%) eligible employees showed interest in participating in the study. Among these, 28/41 (68%) were enrolled in the study; 13/41 (32%) could not participate due to scheduling conflicts or personal reasons. However, 2/28 (7%) left before the beginning of the programme because of scheduling difficulties. Twenty-six employees were therefore eventually enrolled in the programme. Although one participant (4%) abandoned the programme after two sessions due to a scheduling conflict, 21/26 participants completed at least six sessions, leading to a retention rate of 81%. Furthermore, 19/26 (73%) attended the 1-day silent retreat, 26/26 (100%) completed the preintervention survey, 25/26 (96%) completed the postintervention survey and 24/26 (92%) completed the follow-up survey.
All employees (100%) who completed the study reported that the programme had helped them achieve the goals they had set for themselves and had made them more aware of their experience. Participants reported that the programme was (1) ‘excellent’, (2) ‘interesting’ and (3) ‘a very good initiative’. Participants’ comments were positive regarding their overall appreciation of the programme (eg, ‘I would recommend it to others’). They reported that they had learnt many things from their participation in the programme (eg, ‘The importance of living the present moment and to put oneself in the shoes of the other in the caregiver–patient relationship’). Obstacles reported by the participants included: (1) ‘lack of time for home practice’, (2) ‘lack of time to participate in the 8 weekly sessions’ and (3) ‘lack of self-discipline’.
Outcome results
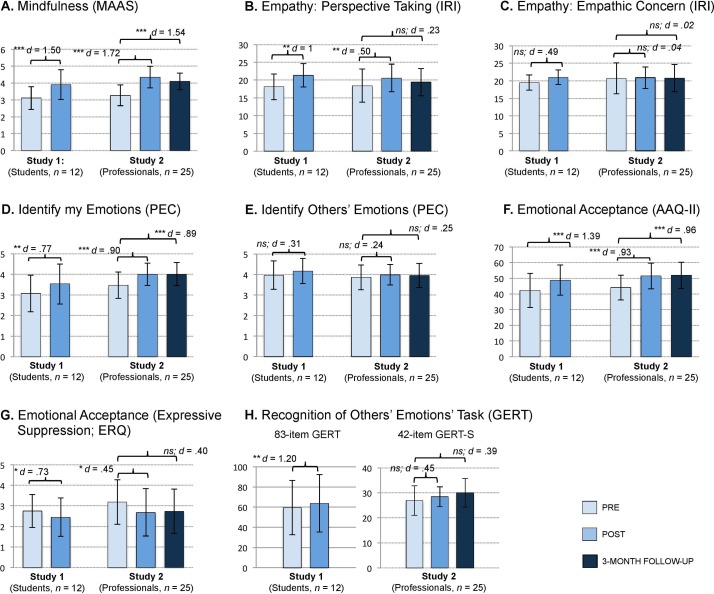
A preliminary analysis checked that the programme was actually related to changes on the mindfulness measure. Results showed very large effect sizes pre–post in Study 1, d=1.53; t(11)=5.29, P<0.001 and Study 2, d=1.72, P<0.001 (figure 1A). Changes were also maintained at follow-up in Study 2, d=1.54, P<0.001. In Study 2, a repeated measures analysis of variance (ANOVA) showed differences in scores over the three time points, F(1.43, 32.90)=35.72, P<0.001, ηp2=.61.
Figure 1.
Changes in outcomes for Study 1 (12 students) and Study 2 (25 professionals) following the PEACE programme. The PEACE programme is an 8-week intervention based on the mindfulness-based stress reduction. (A) Change in mindfulness scores as measured by the Attention Awareness Scale (MAAS). (B) Change in Perspective Taking scores as measured by the Interpersonal Reactivity Index (IRI). (C) Change in Empathic Concern scores as measured by the IRI. (D) Change in the ability to identify one’s own emotions as measured by the Profile of Emotional Competence (PEC). (E) Change in the ability to identify others’ emotions as measured by the PEC. (F) Change in acceptance as measured by the Acceptance and Action Questionnaire (AAQ-II). (G) Change in expressive suppression as measured by the Emotion Regulation Scale (ERQ). (H) Change in the ability to recognise others’ emotions in the face, voice and body as measured by the Geneva Emotion Recognition Test (GERT and GERT-S). *P<0.05; **P<0.01; ***P<0.001. Cohen’s d: 2=small; 5=medium; 8=large; ns, non-significant.
When comparing Study 1 and Study 2 scores at baseline, the differences were small, except for Identify my Emotions and the Geneva Emotion Recognition Test (GERT), and none were statistically significant (online supplementary table S1). When exploring the size of changes associated with the programme, we observed large effect sizes on several pertinent outcomes (figure 1).
bmjopen-2017-018421supp002.pdf (308.6KB, pdf)
Study 1
For Study 1 pre/post comparisons, very large effect sizes were observed for the following: Emotional Acceptance, d=1.39; t(11)=4.81, P<0.001 (figure 1F); the Emotion Recognition Task, d=1.20; t(11)=4.14, P<0.01(figure 1H) and PT (d=1.00; t(11)=3.46, P<0.01 (figure 1B). A medium-to-large effect size was observed for Identify my Emotions (d=0.77; t(11) = 2.67, P<0.05 (figure 1D); and Expressive Suppression, d=0.73; t(11)=2.53, P<0.05 (figure 1G). EC (figure 1C) and Identify Others’ Emotions (figure 1E) showed a small-to-medium effect size but did not reach statistical significance (d=0.49; t(11)=1.70, P=0.118 and d=0.31, t(11) = 1.09, P=0.301, respectively). Table 2 includes full detailed results.
Table 2.
Study 1 and Study 2 outcomes scores at different time points
| Study 1 (students, n=12) | Study 2 (professionals, n=25) | ||||||||||||
| Pre | Post | Pre | Post | Follow-up | |||||||||
| Measure | M | SD | M | SD | P | M | SD | M | SD | P | M | SD | P |
| Mindfulness (MAAS) |
3.11 | 0.67 | 3.91 | 0.88 | <0.001 | 3.27 | 0.62 | 4.35 | 0.64 | <0.001 | 4.13 | 0.49 | <0.001 |
| Perspective Taking (IRI) |
2.58 | 0.52 | 3.05 | 0.47 | 0.005 | 2.63 | 0.67 | 2.94 | 0.56 | 0.009 | 2.77 | 0.55 | 0.594 |
| Empathic Concern (IRI) |
2.79 | 0.31 | 3.00 | 0.29 | 0.118 | 2.96 | 0.63 | 2.98 | 0.44 | 1.00 | 2.97 | 0.56 | 1.00 |
| Identify my Emotions (PEC) | 3.07 | 0.88 | 3.53 | 0.97 | 0.022 | 3.47 | 0.64 | 4.00 | 0.54 | <0.001 | 4.01 | 0.57 | 0.001 |
| Identify Others’ Emotions (PEC) | 3.97 | 0.69 | 4.17 | 0.61 | 0.301 | 3.86 | 0.60 | 3.99 | 0.50 | 0.515 | 3.95 | 0.59 | 1.00 |
| Acceptance (AAQ-II) | 42.25 | 10.83 | 48.83 | 9.61 | 0.001 | 44.08 | 7.85 | 51.54 | 8.21 | <0.001 | 51.88 | 8.42 | <0.001 |
| Expressive Suppression (ERQ) | 2.75 | 0.81 | 2.44 | 0.94 | 0.028 | 3.18 | 1.09 | 2.68 | 1.15 | 0.023 | 2.74 | 1.09 | 0.143 |
| Recognition of Emotions (GERT)∗ | 58.58 | 4.01 | 63.83 | 6.16 | 0.002 | 26.75 | 5.89 | 29.00 | 4.00 | 0.250 | 29.00 | 5.72 | 0.136 |
P values are for changes over time.
*The 83-item original version of the GERT was used for Study 1 and the 42-item short version (GERT-S) was used for Study 2.
AAQ-II, Acceptance and Action Questionnaire; ERQ, Emotion Regulation Questionnaire; GERT, Geneva Emotion Recognition Recognition Test;
IRI, Interpersonal Reactivity Index; MAAS, Mindfulness Attention & Awareness Scale; PEC, Profile of Emotional Competence.
Study 2
The repeated measures ANOVA showed differences in scores over the three time points. These involved the following: PT, F(1.58, 36.40)=5.83, P<0.01, ηp2=0.20; Identify my Emotions, F(2, 46)=16.64, P<0.001, ηp2=0.42; Emotional Acceptance, F(2, 46)=25.78, P<0.001, ηp2=0.53 and Expressive Suppression, F(2, 46)=4.39, P<0.01, ηp2=0.16. We did not find significant differences on EC F(2, 46)=0.023, P=0.977, ηp2=0.001; Identify Others’ Emotions F(2, 46)=1.116, P=0.336, ηp2=0.046 and the Emotion Recognition Task F(2, 46)=2.91, P=0.07, ηp2=0.16 (table 2).
Post hoc pairwise comparisons revealed pre/post improvements with large effect sizes for Emotional Acceptance (d=0.93; figure 1F) and Identify my Emotions (d=0.90; figure 1D). A medium effect size was observed for pre/post differences in PT (d=0.50; figure 1B) and Expressive Suppression (d=0.45; figure 1G). A medium effect size was also observed on the Emotion Recognition Task (d=0.45; figure 1H), but that difference was not statistically significant. A small effect size was observed for the pre/post difference on Identify Others’ Emotions (d=0.24; figure 1D), but the difference was not statistically significant. No effect was noted on EC (d=0.04; figure 1C; online supplementary table S2). In Study 2, we found that effects associated with the programme were maintained over 3 months on the following outcomes: Identify my Emotions (figure 1D), Emotional Acceptance (figure 1F), Expressive Suppression (figure 1G) and the Emotion Recognition Task (figure 1H).
When exploring the role of home practice, we did not find correlations between formal practice with changes on outcomes measured in Study 1. In Study 2, formal practice (yoga, sitting meditation and body scan) was moderately correlated with improvements on Identify my Emotions, r=0.42; P<0.05 and Expressive Suppression, r=–0.52, P<0.01, but did not correlate with other outcomes. Informal practice did not correlate with other outcome changes over time.
Discussion
These two studies are the first to specifically examine the effects of a mindfulness-based programme on students’ and professional caregivers’ emotional competencies. We found that the MBSR-based programme is a feasible and acceptable intervention and that it could achieve an important clinical signal across different emotional measures, particularly in a vulnerable population, namely professional caregivers working in paediatric haematology–oncology.
Participants in this programme showed improvements in their mindfulness skills, with effect sizes larger than those found in previous studies using the same measure with professionals in training31–34 and larger than those reported in studies using other mindfulness scales with healthcare professionals.35–37 Participants also improved on the identification of one’s own emotions, with effect sizes larger than those found in other studies.36 38 During the programme, participants were specifically instructed to attend to their own physical sensations, which allowed them to be more aware of their emotions. Of note, the more professionals practised the formal meditation exercises at home during the programme, the more they reported postintervention improvements on this specific emotional competency (Study 2). Moreover, these improvements were maintained at 3 months postintervention in Study 2, which suggests that the intervention could have lasting effects.
There was no significant improvement in the self-reported ability to identify others’ emotions. This unexpected result could be due to the fact that participants’ prestudy scores were already high on this outcome. To test this hypothesis, we performed an additional analysis comparing our studies’ average baseline scores on the ability to identify other’s emotions (PEC’s Identify Others’ Emotions) with the norms established by the authors of the scale (n=4306).27 Participants in both our studies had very similar baseline scores than the established norms (Study 1: t(4316)=1.44, P=0.151, d=0.42); Study 2: t(4329)=1.36, P=0.174, d=0.27). This suggests that the participants in our studies were not better at identifying others’ emotions at baseline compared with the general population. Thus, there are reasons to believe that the surprising null result for the PEC’s Identify Others’ Emotions in both our studies could be because all formal meditation exercises focused on being attentive to one’s own internal experiences. Perhaps more specific interventions focusing on interpersonal awareness, such as narrative medicine, could be included in the programme to teach participants how to attend to others’ emotions.35 In healthcare, correct identification of emotions in patients is crucial for effective communication, good care planning and patient safety outcomes.39 40 Although some of the exercises practised at the weekly meetings were performed in dyads and incorporated mindful communication, this apparently did not spread to the relation to others’ emotions, as measured with self-report. This contrasts with results from the emotion recognition task (GERT), a more ecological measure, which allows for a direct measure of participants’ ability to recognise a large range of emotions. Interestingly, participants in Study 1 improved significantly on this task with a very large effect size, while the improvement for professionals was not significant. Nevertheless, the latter showed a medium effect size.
Participants also showed improvements in emotional acceptance and these results were maintained at 3 months postintervention in Study 2. These results are in line with previous research, which indirectly measured this competence.36 38 41 42 Mindfulness focuses on the acceptance of one’s own experience in the present moment, whether experienced as positive or negative, without judgement and with an attitude of openness.18 43 44 Instead of trying to avoid or distract themselves from so-called negative emotions, participants here were invited to welcome and pay attention to whatever thoughts and emotions arose in their field of consciousness from moment to moment. It is essential that professional caregivers learn how to accept their emotions instead of avoiding or suppressing them. Previous studies have indeed demonstrated that acceptance was linked to fewer psychological symptoms such as anxiety and depression.45–47
Furthermore, participants improved in PT. These results are consistent with those of Krasner et al,35 who reported an increased ability for PT following an 8-week MBSR-based programme among primary care physicians using the Jefferson Scale of Physician Empathy.35 This study reported a small-to-medium effect size, similar to the effect size found in our second study with professional caregivers. Different pathways might explain improvements in PT in our studies. First, a concurrent improvement in emotional competencies might help caregivers adopt their patients’ point of views. To explore this hypothesis, we performed additional analyses correlating the emotional competencies with PT. Interestingly, change in PT were correlated with change in the PEC total score, which encompasses interpersonal and intrapersonal emotional competencies (Study 1; r=0.67; P<0.01; Study 2: r=0.38; P=0.059). Second, it has been suggested that keeping an emotional distance is advisable in patient care in order to maintain professionals’ emotional balance.48 Perhaps the emotional competencies measured in this study fostered such a distance. Alternatively, they may prevent professional caregivers from confounding their personal experience with that of the patient. A recent study suggests that concentrating too highly on personal emotions is associated with decreased ability to detect distress in persons affected by cancer.49 Future studies should explore more systematically the mechanisms underlying the effects of emotional competencies on PT. Participants did not improve on EC. Although this result may appear surprising, it is consistent with the cognitive effect expected from mindfulness training. This result is also in line with previous results on healthcare providers, which found no significant change on the IRI’s EC.50 51 Perhaps mindfulness does not affect EC: a study found that mindfulness increases PT, but not EC.52 Future research should disentangle cognitive and affective aspects of empathy as they seem differently impacted by mindfulness and have been shown to interact when explaining burnout.53
We should acknowledge certain limitations to our studies. First, participants were self-selected and sample sizes were limited. However, self-selection is relatively ecological as it is a reflection of what would happen if the programmes were offered. Importantly, a large sample selected at random is not necessary at the proof-of-concept stage.21 The results of our studies justify progressing towards more rigorous testing with larger samples in randomised controlled trials. Another limitation lies in the use of self-reports as they bear desirability. Future studies should include more tasks like the one used in this study to approach emotional competence before and after training. Another limitation is the lack of gender balance in our samples. This should be addressed in future studies, as research has suggested that men could be less responsive to empathy-related training than women.54 A final limitation is the low reliability of the ‘Identify my Emotions’ subscale in Study 2.
Notwithstanding these limitations, an important strength of this research is the replication of results between Study 1 and Study 2 on very different populations. Another strength is the high attendance rates (80% and 81%, respectively), which could be explained by the fact that potential participants were well informed about the nature and the structure of the PEACE programme, as well as the required level of commitment before enrolling. For example, professional caregivers were given the chance to attend an information session where they could try a brief meditation session and ask questions about the programme before participating in the study. The instructor also met each participant individually prior to starting the training, in order to evaluate their willingness and readiness to engage in the programme.
In conclusion, the results of these two proof-of-concept studies suggest that MBSR could improve professional caregivers’ PT skills (the cognitive dimension of empathy), but maybe not their EC (the affective dimension of empathy). MBSR could also improve professionals’ emotional competencies, such as identifying and accepting one’s own emotions, which could contribute to the prevention of burnout. MBSR could also be integrated with other forms of interventions to improve professional caregivers’ empathic skills.55 Furthermore, this research could have interesting applications in the training and continuing education of professionals in paediatric oncology and in others emotionally challenging specialities, such as pulmonology, immunology and rheumatology.
Supplementary Material
Acknowledgments
The authors wish to acknowledge the students and professionals who participated in the PEACE programme. We also acknowledge Patricia Dobkin for her very helpful advice and supervision. We are grateful to Marie-Claude Charrette for her help in the recruitment process. We thank Marie-Pier Bilodeau for her work in collecting the data, and Emilie Rondeau for her work through all the stages of the study. Finally, particular thanks to Lucie Gouveia and Sarah Bérubé for their suggestions in the writing of the manuscript.
Footnotes
Contributor: ML participated in the design of the study, coordinated the study, performed the statistical analysis and wrote the manuscript. MD helped design the study and participant recruitment, and revised the manuscript. PM provided advice for the statistical analysis and revised the manuscript. YDP revised the manuscript. SS participated in the design of the study and the coordination of the study, found financial support and coordinated the writing of the manuscript. All authors read and approved the final manuscript.
Funding: This research was supported by the CHU Sainte-Justine Foundation. ML was supported by Grant No. GSM 136461 from the Canadian Institutes of Health Research (CIHR)—Canada Graduate Scholarships-Master’s Programme and Grant No. 32083 from the Fond de recherche du Québec-Santé (FRQS)—Doctoral training.
Competing interests: None declared.
Ethics approval: Research ethics committees of the University of Montreal’s Faculty of Arts and Sciences, and the CHU Sainte-Justine (no 2016–1068).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Hojat M. Empathy in patient care: antecedents, development, measurement, and outcomes. New York, NY: Springer, 2007. [Google Scholar]
- 2.Davis MH. Empathy: a social psychological approach. Madison, Wis: Brown & Benchmark Publishers, 1994. [Google Scholar]
- 3.Kelley JM, Kraft-Todd G, Schapira L, et al. . The influence of the patient-clinician relationship on healthcare outcomes: a systematic review and meta-analysis of randomized controlled trials. PLoS One 2014;9:e94207 10.1371/journal.pone.0094207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hojat M, Louis DZ, Markham FW, et al. . Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med 2011;86:359–64. 10.1097/ACM.0b013e3182086fe1 [DOI] [PubMed] [Google Scholar]
- 5.Rakel D, Barrett B, Zhang Z, et al. . Perception of empathy in the therapeutic encounter: effects on the common cold. Patient Educ Couns 2011;85:390–7. 10.1016/j.pec.2011.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lelorain S, Brédart A, Dolbeault S, et al. . A systematic review of the associations between empathy measures and patient outcomes in cancer care. Psychooncology 2012;21:1255–64. 10.1002/pon.2115 [DOI] [PubMed] [Google Scholar]
- 7.Blatt B, LeLacheur SF, Galinsky AD, et al. . Does perspective-taking increase patient satisfaction in medical encounters? Acad Med 2010;85:1445–52. 10.1097/ACM.0b013e3181eae5ec [DOI] [PubMed] [Google Scholar]
- 8.Decety J, Yang CY, Cheng Y. Physicians down-regulate their pain empathy response: an event-related brain potential study. Neuroimage 2010;50:1676–82. 10.1016/j.neuroimage.2010.01.025 [DOI] [PubMed] [Google Scholar]
- 9.Decety J, Lamm C. Empathy versus personal distress - recent evidence from social neuroscience. The Social Neuroscience of Empathy. Cambridge, MA: MIT Press, 2009. [Google Scholar]
- 10.Altounji D, Morgan H, Grover M, et al. . A self-care retreat for pediatric hematology oncology nurses. J Pediatr Oncol Nurs 2013;30:18–23. 10.1177/1043454212461951 [DOI] [PubMed] [Google Scholar]
- 11.Mukherjee S, Beresford B, Glaser A, et al. . Burnout, psychiatric morbidity, and work-related sources of stress in paediatric oncology staff: a review of the literature. Psychooncology 2009;18:1019–28. 10.1002/pon.1534 [DOI] [PubMed] [Google Scholar]
- 12.Roth M, Morrone K, Moody K, et al. . Career burnout among pediatric oncologists. Pediatr Blood Cancer 2011;57:1168–73. 10.1002/pbc.23121 [DOI] [PubMed] [Google Scholar]
- 13.Liakopoulou M, Panaretaki I, Papadakis V, et al. . Burnout, staff support, and coping in Pediatric Oncology. Support Care Cancer 2008;16:143–50. 10.1007/s00520-007-0297-9 [DOI] [PubMed] [Google Scholar]
- 14.Bowden MJ, Mukherjee S, Williams LK, et al. . Work-related stress and reward: an Australian study of multidisciplinary pediatric oncology healthcare providers. Psychooncology 2015;24:1432–8. 10.1002/pon.3810 [DOI] [PubMed] [Google Scholar]
- 15.Gleichgerrcht E, Decety J. The costs of empathy among health professionals Decety J, Empathy: from bench to bedside. London, England: The MIT Press, 2012:245–61. [Google Scholar]
- 16.Decety J, Meyer M. From emotion resonance to empathic understanding: a social developmental neuroscience account. Dev Psychopathol 2008;20:1053–80. 10.1017/S0954579408000503 [DOI] [PubMed] [Google Scholar]
- 17.Decety J. The neurodevelopment of empathy in humans. Dev Neurosci 2010;32:257–67. 10.1159/000317771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kabat-Zinn J. Full catastrophe living: using the wisdom of your body and mind to face stress, pain, and illness. Revised and updated edition. New York, NY: Bantam Books trade paperback, 2013. [Google Scholar]
- 19.Lamothe M, Rondeau É, Malboeuf-Hurtubise C, et al. . Outcomes of MBSR or MBSR-based interventions in health care providers: a systematic review with a focus on empathy and emotional competencies. Complement Ther Med 2016;24:19–28. 10.1016/j.ctim.2015.11.001 [DOI] [PubMed] [Google Scholar]
- 20.Dean S, Foureur M, Zaslawski C, et al. . The effects of a structured mindfulness program on the development of empathy in healthcare students. NursingPlus Open 2017;3:1–5. 10.1016/j.npls.2017.02.001 [DOI] [Google Scholar]
- 21.Czajkowski SM, Powell LH, Adler N, et al. . From ideas to efficacy: The ORBIT model for developing behavioral treatments for chronic diseases. Health Psychol 2015;34:971–82. 10.1037/hea0000161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moody K, Kramer D, Santizo RO, et al. . Helping the helpers: mindfulness training for burnout in pediatric oncology--a pilot program. J Pediatr Oncol Nurs 2013;30:275–84. 10.1177/1043454213504497 [DOI] [PubMed] [Google Scholar]
- 23.Schlegel K, Grandjean D, Scherer KR. Introducing the Geneva emotion recognition test: an example of rasch-based test development. Psychol Assess 2014;26:666–72. 10.1037/a0035246 [DOI] [PubMed] [Google Scholar]
- 24.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol 2003;84:822–48. 10.1037/0022-3514.84.4.822 [DOI] [PubMed] [Google Scholar]
- 25.Jermann F, Billieux J, Larøi F, et al. . Mindful Attention Awareness Scale (MAAS): psychometric properties of the French translation and exploration of its relations with emotion regulation strategies. Psychol Assess 2009;21:506–14. 10.1037/a0017032 [DOI] [PubMed] [Google Scholar]
- 26.Davis MH. A multidimensional approach to individual differences in empathy. JSAS Catalog of Selected Documents in Psychology 1980;10:85. [Google Scholar]
- 27.Brasseur S, Grégoire J, Bourdu R, et al. . The Profile of Emotional Competence (PEC): development and validation of a self-reported measure that fits dimensions of emotional competence theory. PLoS One 2013;8:e62635 10.1371/journal.pone.0062635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bond FW, Hayes SC, Baer RA, et al. . Preliminary psychometric properties of the acceptance and action questionnaire-II: a revised measure of psychological inflexibility and experiential avoidance. Behav Ther 2011;42:676–88. 10.1016/j.beth.2011.03.007 [DOI] [PubMed] [Google Scholar]
- 29.Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol 2003;85:348–62. 10.1037/0022-3514.85.2.348 [DOI] [PubMed] [Google Scholar]
- 30.Schlegel K, Scherer KR. Introducing a short version of the Geneva Emotion Recognition Test (GERT-S): psychometric properties and construct validation. Behav Res Methods 2016;48:1383–92. 10.3758/s13428-015-0646-4 [DOI] [PubMed] [Google Scholar]
- 31.Newsome S, Waldo M, Gruszka C. Mindfulness group work: preventing stress and increasing self-compassion among helping professionals in training. J for Spec in Group Work 2012;37:297–311. 10.1080/01933922.2012.690832 [DOI] [Google Scholar]
- 32.Gökhan N, Meehan EF, Peters K. The value of mindfulness-based methods in teaching at a clinical field placement. Psychol Rep 2010;106:455–66. 10.2466/pr0.106.2.455-466 [DOI] [PubMed] [Google Scholar]
- 33.Cohen JS, Miller LJ. Interpersonal mindfulness training for well-being: a pilot study with psychology graduate students. Teachers College Record 2009;111:2760–74. [Google Scholar]
- 34.Shapiro SL, Brown KW, Biegel GM. Teaching self-care to caregivers: effects of mindfulness-based stress reduction on the mental health of therapists in training. Train Educ Prof Psychol 2007;1:105–15. 10.1037/1931-3918.1.2.105 [DOI] [Google Scholar]
- 35.Krasner MS, Epstein RM, Beckman H, et al. . Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA 2009;302:1284–93. 10.1001/jama.2009.1384 [DOI] [PubMed] [Google Scholar]
- 36.Amutio A, Martínez-Taboada C, Hermosilla D, et al. . Enhancing relaxation states and positive emotions in physicians through a mindfulness training program: A one-year study. Psychol Health Med 2015;20:720–31. 10.1080/13548506.2014.986143 [DOI] [PubMed] [Google Scholar]
- 37.Brady S, O’Connor N, Burgermeister D, et al. . The impact of mindfulness meditation in promoting a culture of safety on an acute psychiatric unit. Perspect Psychiatr Care 2012;48:129–37. 10.1111/j.1744-6163.2011.00315.x [DOI] [PubMed] [Google Scholar]
- 38.Manotas M, Segura C, Eraso M, et al. . Association of brief mindfulness training with reductions in perceived stress and distress in Colombian health care professionals. Int J Stress Manag 2014;21:207–25. 10.1037/a0035150 [DOI] [Google Scholar]
- 39.Codier E, Codier D. A model for the role of emotional intelligence in patient safety. Asia Pac J Oncol Nurs 2015;2:112–7. 10.4103/2347-5625.157594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Codier E, Muneno L, Freitas E. Emotional intelligence abilities in oncology and palliative care. J Hosp Palliat Nurs 2011;13:183–8. 10.1097/NJH.0b013e31820ce14b [DOI] [Google Scholar]
- 41.de Vibe M, Solhaug I, Tyssen R, et al. . Mindfulness training for stress management: a randomised controlled study of medical and psychology students. BMC Med Educ 2013;13:107 10.1186/1472-6920-13-107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Asuero AM, Queraltó JM, Pujol-Ribera E, et al. . Effectiveness of a mindfulness education program in primary health care professionals: a pragmatic controlled trial. J Contin Educ Health Prof 2014;34:4–12. 10.1002/chp.21211 [DOI] [PubMed] [Google Scholar]
- 43.Hayes SC, Luoma JB, Bond FW, et al. . Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther 2006;44:1–25. 10.1016/j.brat.2005.06.006 [DOI] [PubMed] [Google Scholar]
- 44.Linehan M. Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press, 1993. [Google Scholar]
- 45.Bond FW, Bunce D. Mediators of change in emotion-focused and problem-focused worksite stress management interventions. J Occup Health Psychol 2000;5:156–63. 10.1037/1076-8998.5.1.156 [DOI] [PubMed] [Google Scholar]
- 46.Plumb JC, Orsillo SM, Luterek JA. A preliminary test of the role of experiential avoidance in post-event functioning. J Behav Ther Exp Psychiatry 2004;35:245–57. 10.1016/j.jbtep.2004.04.011 [DOI] [PubMed] [Google Scholar]
- 47.Márquez-González M, Cabrera I, Losada A, et al. . Attentional avoidant biases as mediators in the association between experiential avoidance and blood pressure in dementia family caregivers. Aging Ment Health 2017:1–9. 10.1080/13607863.2017.1293003 [DOI] [PubMed] [Google Scholar]
- 48.Hojat M, Gonnella JS, Mangione S, et al. . Physician empathy in medical education and practice: experience with the Jefferson scale of physician empathy. Seminars in Integrative Medicine 2003;1:25–41. 10.1016/S1543-1150(03)00002-4 [DOI] [Google Scholar]
- 49.Gouveia L, Janvier A, Dupuis F, et al. . Comparing two types of perspective taking as strategies for detecting distress amongst parents of children with cancer: A randomised trial. PLoS One 2017;12:e0175342 10.1371/journal.pone.0175342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Beddoe AE, Murphy SO. Does mindfulness decrease stress and foster empathy among nursing students? J Nurs Educ 2004;43:305–12. [DOI] [PubMed] [Google Scholar]
- 51.Galantino ML, Baime M, Maguire M, et al. . Association of psychological and physiological measures of stress in health-care professionals during an 8-week mindfulness meditation program: mindfulness in practice. Stress and Health 2005;21:255–61. 10.1002/smi.1062 [DOI] [Google Scholar]
- 52.Birnie K, Speca M, Carlson LE. Exploring self-compassion and empathy in the context of mindfulness-based stress reduction (MBSR). Stress and Health 2010;26:359–71. 10.1002/smi.1305 [DOI] [Google Scholar]
- 53.Lamothe M, Boujut E, Zenasni F, et al. . To be or not to be empathic: the combined role of empathic concern and perspective taking in understanding burnout in general practice. BMC Fam Pract 2014;15:15:15 10.1186/1471-2296-15-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hall JA, Blanch-Hartigan D, Roter DL. Patients’ satisfaction with male versus female physicians: a meta-analysis. Med Care 2011;49:611–7. 10.1097/MLR.0b013e318213c03f [DOI] [PubMed] [Google Scholar]
- 55.Riess H, Kelley JM, Bailey RW, et al. . Empathy training for resident physicians: a randomized controlled trial of a neuroscience-informed curriculum. J Gen Intern Med 2012;27:1280–6. 10.1007/s11606-012-2063-z [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-018421supp001.pdf (310.4KB, pdf)
bmjopen-2017-018421supp002.pdf (308.6KB, pdf)