Abstract
Few studies have examined recent trends in the length of stay (LOS) among patients hospitalized with a first uncomplicated acute myocardial infarction (AMI) and the impact of early hospital discharge on various short-term outcomes in these low risk patients. We used data from 1,501 residents of central Massachusetts hospitalized with a first uncomplicated AMI at all central Massachusetts medical centers on a biennial basis between 2001 and 2011. The association between hospital LOS and subsequent hospital readmission or death was examined using logistic regression modelling. The average age of the study population was 63.7 years, 63.0% were men, and 91.4% were non-Hispanic whites. The average hospital LOS declined from 4.1 days in 2001 to 2.9 days in 2011. During the years under study, the average 30-day hospital readmission rate was 11.9%, while the 30-and 90-day death rates were 1.5% and 2.9%, respectively. The multivariable adjusted odds of a 30-day hospital readmission (OR=0.81, 95%CI=0.52–1.41), or 30-day (OR=0.93, 95%CI=0.29–2.98) and 90-day (OR=0.89, 95%CI=0.36–2.20) death rates were not significantly different between patients who were discharged from central Massachusetts medical centers during the first 2 days as compared with those discharged thereafter. In conclusion, the average LOS in patients with a first uncomplicated AMI declined during the years under study and early discharge from the hospital at day 2 or sooner of these low risk patients does not appear to be associated with an increased risk of adverse events post discharge compared with those discharged at a later time.
Keywords: Length of hospital stay, early hospital discharge, acute myocardial infarction
The average length of stay (LOS) for patients hospitalized with acute myocardial infarction (AMI) has declined significantly over the past several decades.1 In recent years, increasing pressure has been placed on hospitals to discharge patients early after an AMI when medically possible. However, early hospital discharge may negatively affect quality of care and lead to adverse outcomes. Prior observational studies and randomized clinical trials have shown that the early (≤72 hours) hospital discharge of patients with an uncomplicated, low risk, AMI is safe and cost-effective.2–5 However, few studies have examined recent trends in LOS among patients hospitalized with a first uncomplicated AMI, and the impact of early hospital discharge on short-term outcomes in these patients. We examined decade-long (2001–2011) trends in hospital LOS for patients with a first uncomplicated AMI and the impact of early hospital discharge on 30-day hospital readmissions and 30 and 90-day all-cause death rates in these patients.
METHODS
Data from the Worcester Heart Attack Study, an ongoing population-based investigation that is examining long-term trends in the incidence, hospital, and post-discharge case-fatality rates of AMI among residents of the Worcester, Massachusetts, metropolitan area, were used for this investigation. The details of this study have been described previously.6 In brief, the medical records of residents of central Massachusetts hospitalized for possible AMI at the 11 medical centers serving residents of this metropolitan area were individually reviewed and a diagnosis of AMI was validated according to criteria developed by the World Health Organization with further sub-classification into those with an ST-segment elevation AMI (STEMI) or Non-ST segment elevation AMI (NSTEMI).7 This investigation was approved by the Institutional Review Board at the University of Massachusetts Medical School.
We excluded 2,881 patients (out of a total eligible pool of 5,783 patients with confirmed AMI) who were admitted to participating study hospitals who developed any clinically significant complications during their acute hospitalization including heart failure, pulmonary edema, cardiogenic shock, ventricular arrhythmias or cardiac arrest, atrial fibrillation, a reinfarction, or who died (n=76) during the index hospital stay.4 We further excluded patients with a previously diagnosed AMI (n=747) to remove the potentially confounding effects of a previous AMI on the natural history and prognosis of these patients. We excluded 128 patients who underwent coronary artery bypass graft surgery, since these patients typically have a longer hospital stay post operation, and 206 patients with a Do Not Resuscitate order. Finally, we excluded 244 patients who had missing data on key study variables. The final study population consisted of 1,501 residents of the Worcester metropolitan area with a first uncomplicated AMI who were hospitalized at all 11 central Massachusetts medical centers during 6 biennial periods between 2001 and 2011.
A subsequent hospital admission for any reason within 30 days following discharge from the patient’s index hospitalization for AMI was considered a 30-day readmission. Trained study staff searched subsequent hospital medical records and state and national death certificates for any post discharge death among the 1,501 patients discharged from all 11 participating study hospitals after their index uncomplicated initial AMI. These trained staff members also searched subsequent medical records from the 3 major city of Worcester teaching and community hospitals to identify any subsequent hospital readmissions to these major medical centers among the 1,364 patients who were discharged from these hospitals after a first uncomplicated AMI. Since the death rates at 30 days post hospital discharge were low, we examined all-cause mortality at both 30 and 90 days after hospital discharge for the patient’s index AMI.
We categorized hospital LOS during the patient’s index AMI as either ≤2 days, 3 days, and ≥4 days. This categorization was based, in part, on the results of several clinical trials which have shown that hospital discharge at day 3 was safe and cost-effective for patients with a low risk AMI.4,5,8 We examined differences in the distribution of a number of patient demographic, medical history, and clinical characteristics between patients in the early (≤2 days) or late (≥4 days) versus 3 day groups (reference category) using Chi-square tests for discrete variables and the Kruskal -Wallis test for non-normally distributed continuous variables.
Trends in mean hospital LOS between 2001 and 2011 were examined after adjustment for a number of demographic and clinical factors using multiple linear regression modelling. Due to few deaths at 30 days (n=23) and at 90 days (n=43) in our study population, the association between LOS and death was examined using penalized maximum likelihood logistic regression by Firth’s method to reduce the bias in maximum likelihood estimation with a rare event.9 Potentially confounding variables to be included in our regression analyses were tested in an iterative fashion and variables that changed the estimates of the effects of LOS on our post-discharge outcomes by more than 10% were retained in the final regression models. Analyses for post-discharge mortality were conducted in the total sample of 1,501 patients discharged from all 11 Worcester metropolitan area hospitals, while the analyses for hospital readmission were conducted in the sample of 1,364 patients who were hospitalized at the 3-major city of Worcester medical centers in whom hospital readmission data were available. Since patients who were transferred to our 3-major city of Worcester hospitals for further care and/or receipt of invasive cardiac procedures might have experienced a longer hospital LOS, we carried out a similar series of analyses in which we excluded patients who were transferred to the 3 major referral hospitals in the city of Worcester. This subgroup analysis showed similar results to those observed in the entire study sample. All analyses were conducted on Stata Release 13 (College Station, TX: StataCorp LP).
RESULTS
The mean age of the study population was 63.7 years, 63.0% were men, and 91.4% were non-Hispanic white. One third of the study population had an STEMI, and two-thirds underwent a percutaneous coronary intervention (PCI). Between 2001 and 2011, the average length of hospital stay for patients with a first uncomplicated AMI was 3.5 days (median: 3 days, interquartile range: 2–4 days). Hospital readmissions for any reason within 30 days after discharge occurred in 11.9% of patients, and death occurred in 1.5% and 2.9% of patients within the first 30 and 90-days post discharge, respectively.
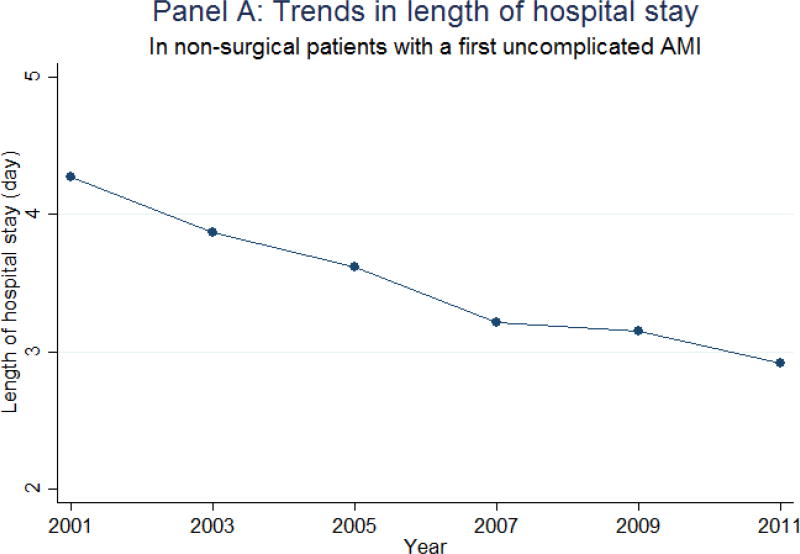
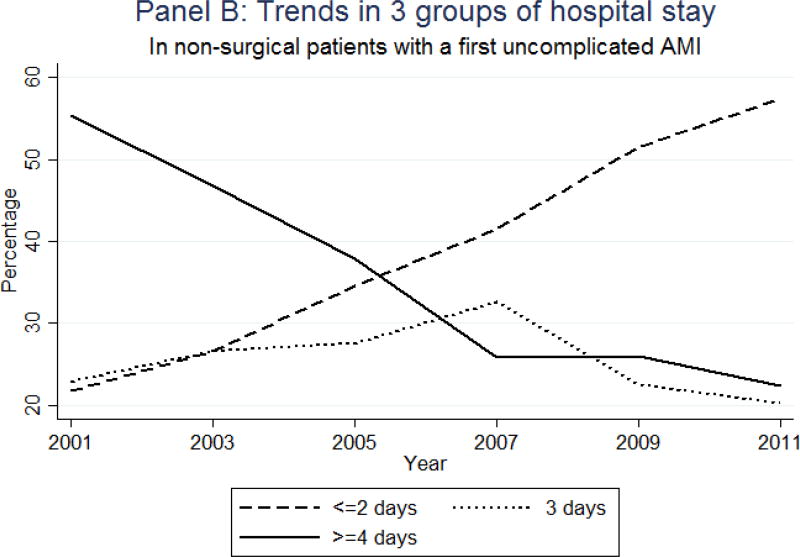
During the period under study, the average hospital LOS steadily declined from 4.3 days in 2001 to 2.9 days in 2011 (Figure 1-Panel A). After adjusting for changes in patient’s demographic and clinical characteristics during the decade long period under study, the average LOS significantly decreased by 0.14 (95%CI = 0.11 – 0.18) days after each study year. The percentage of patients who were discharged early (within the first 2 days) increased during the years under study, from 21.7% in 2001 to 57.8% in 2011, whereas the percentage of patients who were discharged after 4 or more days markedly declined over time (55.3% in 2001; 22.4% in 2011) (Figure 1-Panel B).
Figure 1.
Trends in length of hospital stay in non-surgical patients admitted to the hospital with a first uncomplicated acute myocardial infarction (AMI): Worcester Heart Attack Study
Patients who were discharged from all central Massachusetts medical centers during the first 2 days after admission had relatively similar characteristics with patients who were discharged at 3 days with a few exceptions. These included a higher percentage of men, those with higher systolic blood pressure and lower troponin I levels at the time of hospital admission, and a lower percentage of those diagnosed with a STEMI or who were treated with lipid-lowering medication during their acute hospitalization (Table 1). Compared with patients who were discharged from the hospital at 3 days, patients who were discharged at a later time (≥4 days) were approximately 7 years older, included a lower percentage of men, those with a higher average heart rate and white blood cell count findings, and a lower glomerular filtration rate at the time of hospital admission. These patients also had a higher prevalence of several previously diagnosed medical conditions including atrial fibrillation, chronic kidney disease, lung disease, and hypertension. Fewer of these patients were treated with either a PCI or lipid-lowering medication, while a higher percentage were treated with diuretics during their acute hospital stay compared with patients who were discharged from the hospital at 3 days.
Table 1.
Characteristics of patients with an uncomplicated initial acute myocardial infarction according to length of hospital stay: Worcester Heart Attack Study
| Variables | ≤2 days (n= 572) |
3 days (n=386) |
≥4 days (n= 543) |
p1 | p2 |
|---|---|---|---|---|---|
| Age (years) | 59 [53–70] | 62 [51–73] | 69 [57–78] | 0.15 | <0.001 |
| Age | 0.09 | <0.001 | |||
| <55 | 189 (33.0%) | 122 (31.6%) | 114 (21.0%) | ||
| 55–64 | 171 (29.9%) | 92 (23.8%) | 104 (19.2%) | ||
| 65–74 | 111 (19.4%) | 88 (22.8%) | 124 (22.8%) | ||
| ≥75 | 101 (17.7%) | 84 (21.8%) | 201 (37.0%) | ||
| Men | 405 (70.8%) | 246 (63.7%) | 295 (54.3%) | 0.021 | 0.004 |
| White | 510 (92.4%) | 338 (91.4%) | 468 (90.4%) | 0.57 | 0.61 |
| Transferred from other hospitals | 86 (15.0%) | 46 (11.9%) | 52 (9.6%) | 0.17 | 0.25 |
| Angina pectoris | 41 (7.2%) | 36 (9.3%) | 65 (12.0%) | 0.23 | 0.20 |
| Atrial fibrillation | 30 (5.2%) | 22 (5.7%) | 61 (11.2%) | 0.76 | 0.004 |
| Chronic obstructive pulmonary disease | 49 (8.6%) | 43 (11.1%) | 85 (15.7%) | 0.19 | 0.049 |
| Chronic kidney disease | 32 (5.6%) | 27 (7.0%) | 88 (16.2%) | 0.38 | <0.001 |
| Diabetes mellitus | 127 (22.2%) | 101 (26.2%) | 160 (29.5%) | 0.16 | 0.27 |
| Heart failure | 16 (2.8%) | 17 (4.4%) | 37 (6.8%) | 0.18 | 0.12 |
| Hypertension | 359 (62.8%) | 241 (62.4%) | 382 (70.4%) | 0.92 | 0.011 |
| Peripheral artery disease | 49 (8.6%) | 37 (9.6%) | 66 (12.2%) | 0.59 | 0.22 |
| Stroke/Transient ischemic attack | 33 (5.8%) | 33 (8.6%) | 59 (10.9%) | 0.10 | 0.24 |
| ST-segment elevation myocardial infarction | 178 (31.1%) | 150 (38.9%) | 180 (33.2%) | 0.013 | 0.07 |
| Admission presentation | |||||
| Heart rate (bpm) | 80 [68–90] | 80 [67–92] | 82 [70–99] | 0.57 | 0.006 |
| Systolic blood pressure (mmHg) | 149 [130–165] | 143 [124–162] | 142 [122–162] | 0.023 | 0.71 |
| Troponin I (ng/ml) | 0.27 [0.09–1.40] | 0.45 [0.10–3.30] | 0.66 [0.10–4.20] | 0.001 | 0.17 |
| Glomerular filtration rate (ml/min) | 61.0 [60.0–79.9] | 63.8 [58.0–80.6] | 60.3 [50.2–78.4] | 0.82 | 0.003 |
| Glucose (mg/dl) | 127 [108–158] | 130 [109–165] | 136 [111–181] | 0.29 | 0.05 |
| White blood cell count (109 cell/L) | 8.7 [7.0–10.6] | 9.0 [7.2–11.3] | 9.5 [7.3–12,3] | 0.15 | 0.028 |
| Medical treatment | |||||
| Angiotensin converting enzyme inhibitor/Angiotensin receptor blocker | 388 (67.8%) | 274 (71.0%) | 397 (73.1%) | 0.30 | 0.48 |
| Aspirin | 549 (96.0%) | 372 (96.4%) | 518 (95.4%) | 0.76 | 0.46 |
| Beta-blockers | 527 (92.1%) | 363 (94.0%) | 507 (93.4%) | 0.26 | 0.68 |
| Diuretics | 90 (15.7%) | 70 (18.1%) | 148 (27.3%) | 0.33 | 0.001 |
| Statins | 449 (78.5%) | 326 (84.5%) | 422 (77.7%) | 0.021 | 0.011 |
| Percutaneous coronary intervention | 403 (70.5%) | 274 (71.0%) | 314 (57.8%) | 0.86 | <0.001 |
p-values from Chi-square and Fisher’s-exact test for categorical variables, and Kruskal-Wallis test for continuous variables, p1: compares hospital discharge at ≤2 days vs. 3 days, p2: compares hospital discharge at 3 days vs. ≥4days
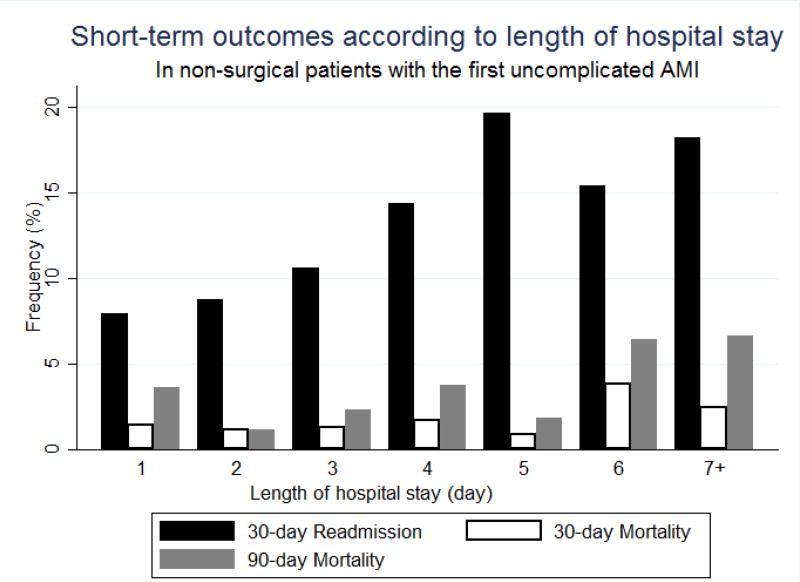
The 30-day hospital readmission rate and 90-day death rates were significantly higher in patients who had a longer hospital stay compared with patients who stayed for a shorter duration (p<0.05, Figure 2). The odds of being readmitted to the 3 principal city of Worcester hospitals within 30-days was 1.57-fold higher (95%CI = 1.05–2.35) in patients who were discharged later than 3 days compared with patients who were discharged at 3 days (Table 2). However, after adjustment for various potentially confounding demographic and clinical variables, there were no significant differences in either 30-day hospital readmissions among patients who were initially treated at our 3 major city medical centers, or in the 30- and 90-day all-cause death rates among all patients discharged from the 11 central Massachusetts medical centers, between our 3 LOS comparison groups (Table 2).
Figure 2.
Short-term outcomes according to length of hospital stay in non-surgical patients admitted to the hospital for a first uncomplicated acute myocardial infarction (AMI): Worcester Heart Attack Study
Table 2.
Association between clinical outcomes and length of hospital stay in the first 30 and 90 days after hospital discharge among patients with an uncomplicated acute myocardial infarction: Worcester Heart Attack Study
| ≤2 days | 3 days | ≥4 days | |
|---|---|---|---|
|
|
|||
| OR (95%CI) | OR (95%CI) | OR (95%CI) | |
|
|
|||
| 30-day hospital readmission | |||
| Unadjusted | 0.78 (0.50–1.22) | Reference | 1.57 (1.05–2.35) |
| Adjusted† | 0.81 (0.52–1.41) | Reference | 1.39 (0.92–2.10) |
| 30-day mortality | |||
| Unadjusted | 0.92 (0.30–2.79) | Reference | 1.50 (0.54–4.17) |
| Adjusted‡ | 0.93 (0.29–2.98) | Reference | 0.98 (0.34–2.79) |
| 90-day mortality | |||
| Unadjusted | 0.74 (0.31–1.80) | Reference | 1.87 (0.88–4.01) |
| Adjusted§ | 0.89 (0.36–2.20) | Reference | 1.19 (0.54–2.61) |
OR: odds ratio, CI: confidence interval
Note: Analyses for post-discharge mortality were conducted in a total sample of 1,501 patients discharged from all 11 metropolitan Worcester hospitals, while the analyses for hospital readmission were conducted in a subsample of 1,364 patients in whom readmission data were available from 3 city of Worcester hospitals.
Adjusted for age and comorbid chronic kidney disease
Adjusted for age and race
Adjusted for age and receipt of a percutaneous coronary intervention
DISCUSSION
We found a continuous decline in the average and median length of hospital stay for non-surgical patients who were admitted to the hospital for a first uncomplicated AMI. We also found that patients who were discharged early (2 days or less) had similar short-term outcomes compared with patients who were discharged at a later time.
Since the first clinical trial in 1988 which showed the safety and efficacy of early discharge at 3 days for low-risk patients hospitalized with an uncomplicated AMI,4 a 3 day LOS for patients with an uncomplicated AMI has become increasingly popular in clinical practice.2,5,10 There are several factors that may have contributed to this trend. For example, the shortened arrival to intervention time inspired by the Door-to-Balloon Alliance for Quality program was associated with a considerably shortened LOS.11–13 The increasing uptake of radial access for patients undergoing a PCI has also reduced the average LOS for patients hospitalized with an AMI due to fewer bleeding complications and shorter monitoring time required.14–16
Given support for the safe management of patients with an uncomplicated, low risk, AMI,17 many hospitals have shifted the management of patients with an AMI from the inpatient to outpatient setting, which constitutes early discharge and an early follow-up visit in a cardiology clinic. Our study showed that an increasing proportion of patients were discharged from central Massachusetts medical centers sooner during the years under study, perhaps due to the shifting from hospital to clinic-based management of these low-risk patients.
Many physicians have raised concerns that a short LOS is inadequate to provide effective treatment to patients with AMI. However, in the present study a shorter LOS was not associated with poorer quality of care, as similar proportions of patients discharged early (2 days or less) received evidence-based treatment practices as patients who were discharged at 3 days. Interestingly, patients who were discharged at a later time were less likely to have undergone a PCI or been treated with statins compared with patients discharged at 3 days. Data from the Get With The Guidelines program also showed that a higher percentage of patients who were discharged before 4 days received evidence-based cardiac medications compared with patients discharged after 4 days.18 Thus, patients who were discharged early may not be less likely to receive effective cardiac treatment regimens.
We found that the short-term outcomes that were examined in the present study were not significantly different in patients discharged from central Massachusetts medical centers early as compared with patients discharged at hospital day 3. This finding confirms results from prior clinical trials in patients treated with a PCI for a STEMI, including the Prague-5 and the Early Discharge after Primary Percutaneous Coronary Intervention (EDAPPCI) trials.2,19
The similar hospital readmission and mortality findings observed between the early and day 3 patient discharge groups in the present study may be explained by many similarities between these two groups with regards to their medical history and clinical presentation at the time of hospital admission. Inasmuch, early discharge from the hospital at ≤2 days may be as safe as discharge at 3 days in non-surgical patients with an uncomplicated first AMI. An early discharge strategy is made possible with early out-patient follow-up visits after discharge since many important components for the successful management of patients, including patient education or behavioral interventions, can be effectively carried out in the outpatient setting.20 Furthermore, early outpatient follow-up is associated with better evidence-based medication use among patients, perhaps due to the fact that many adverse effects that cause medication nonadherence occur days or weeks after taking the medication.20–23 An in-hospital monitoring period for the initiation of evidence-based medications may not be cost-effective and further lengthens the hospital stay.
Our study included patients treated with a PCI and non-invasive medical treatment, as well as patients with a STEMI and NSTEMI; other studies have only focused on STEMI patients who were successfully treated with a PCI.19,24 Many stable patients with a low risk NSTEMI can be successfully managed with an ischemia-guided strategy, which avoids the use of invasive coronary intervention procedures, unless patients experience refractory or recurrent ischemic symptoms or become hemodynamically unstable.25 Data from 920 patients with a NSTEMI enrolled in the multicenter randomized Veterans Affairs Non–Q-Wave Infarction Strategies in Hospital (VANQWISH) trial showed that an ischemia-based strategy resulted in a shorter LOS and receipt of fewer coronary interventions or coronary artery graft bypass surgery in comparison to patients treated with an early reperfusion strategy.26
The strengths of the present study include data from an established community-based study of AMI. However, we were unable to examine the timing, quantity, and quality of outpatient visits following hospital discharge, which may have been differential between our hospital LOS comparison groups. Being an observational study, there are a number of unmeasured potentially confounding factors that may have affected our study findings. Inasmuch, a large, randomized trial comparing short-term outcomes in patients who are discharged from the hospital after experiencing a low risk uncomplicated AMI at 2 days versus 3 days may be warranted to replicate and extend our findings.
Acknowledgments
Partial support for R.J.G. was provided by NIH/NHLBI grants 1R01HL126911-01A1, 5R01HL125089-02, and 5R01HL115295-05. Partial support for M.S.T. was provided by the National Institute of Aging, Advancing Geriatrics Infrastructure & Network Growth (AGING) grant 1R24AG045050. Partial support for J.Y. and G.E. was provided by NIH grant 1R01HL135129-01.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DISCLOSURES
Partial support for R.J.G. was provided by NIH/NHLBI grant 1R01HL126911-01A1, 5R01HL125089-02, and 5R01HL115295-05. Partial support for M.S.T. was provided by the National Institute of Aging, Advancing Geriatrics Infrastructure & Network Growth (AGING) grant 1R24AG045050. Partial support for J.Y. and E.G. was provided by NIH 1R01HL135219-01. Other authors declare no conflict of interest.
References
- 1.Saczynski JS, Lessard D, Spencer FA, Gurwitz JH, Gore JM, Yarzebski J, Goldberg RJ. Declining length of stay for patients hospitalized with AMI: impact on mortality and readmissions. Am J Med. 2010;123:1007–1015. doi: 10.1016/j.amjmed.2010.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Satılmısoglu MH, Gorgulu S, Aksu HU, Aksu H, Ertaş G, Tasbulak O, Buturak A, Kalkan AK, Degirmencioglu A, Koroglu B, Tusun E, Murat A, Oz A. Safety of Early Discharge After Primary Percutaneous Coronary Intervention. Am J Cardiol. 2016;117:1911–1916. doi: 10.1016/j.amjcard.2016.03.039. [DOI] [PubMed] [Google Scholar]
- 3.Vavalle JP, Lopes RD, Chen AY, Newby LK, Wang TY, Shah BR, Ho PM, Wiviott SD, Peterson ED, Roe MT, Granger CB. Hospital Length of Stay in Patients with Non-ST-segment Elevation Myocardial Infarction. Am J Med. 2012;125:1085–1094. doi: 10.1016/j.amjmed.2012.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Topol EJ, Burek K, O'Neill WW, Kewman DG, Kander NH, Shea MJ, Schork MA, Kirscht J, Juni JE, Pitt B. A randomized controlled trial of hospital discharge three days after myocardial infarction in the era of reperfusion. N Engl J Med. 1988;318:1083–1088. doi: 10.1056/NEJM198804283181702. [DOI] [PubMed] [Google Scholar]
- 5.Grines CL, Marsalese DL, Brodie B, Griffin J, Donohue B, Costantini CR, Balestrini C, Stone G, Wharton T, Esente P, Spain M, Moses J, Nobuyoshi M, Ayres M, Jones D, Mason D, Sachs D, Grines LL, O’Neill W. Safety and Cost-Effectiveness of Early Discharge After Primary Angioplasty in Low Risk Patients With Acute Myocardial Infarction. J Am Coll Cardiol. 1998;31:967–972. doi: 10.1016/s0735-1097(98)00031-x. [DOI] [PubMed] [Google Scholar]
- 6.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Recent changes in attack and survival rates of acute myocardial infarction (1975 through 1981): the Worcester Heart Attack Study. JAMA. 1986;255:2774–2779. [PubMed] [Google Scholar]
- 7.Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Joint ESCAAHAWHFTFftUDoMI. Katus HA, Lindahl B, Morrow DA, Clemmensen PM, Johanson P, Hod H, Underwood R, Bax JJ, Bonow RO, Pinto F, Gibbons RJ, Fox KA, Atar D, Newby LK, Galvani M, Hamm CW, Uretsky BF, Steg PG, Wijns W, Bassand JP, Menasche P, Ravkilde J, Ohman EM, Antman EM, Wallentin LC, Armstrong PW, Simoons ML, Januzzi JL, Nieminen MS, Gheorghiade M, Filippatos G, Luepker RV, Fortmann SP, Rosamond WD, Levy D, Wood D, Smith SC, Hu D, Lopez-Sendon JL, Robertson RM, Weaver D, Tendera M, Bove AA, Parkhomenko AN, Vasilieva EJ, Mendis S. Third universal definition of myocardial infarction. Circulation. 2012;126:2020–2035. doi: 10.1161/CIR.0b013e31826e1058. [DOI] [PubMed] [Google Scholar]
- 8.Bogaty P, Dumont S, O’Hara GE, Boyer L, Auclair L, Jobin J, Boudreault J-R. Randomized trial of a noninvasive strategy to reduce hospital stay for patients with low-risk myocardial infarction. J Am Coll Cardiol. 2001;37:1289–1296. doi: 10.1016/s0735-1097(01)01131-7. [DOI] [PubMed] [Google Scholar]
- 9.Firth D. Bias reduction of maximum likelihood estimates. Biometrika. 1993;80:27–38. [Google Scholar]
- 10.Kotowycz MA, Cosman TL, Tartaglia C, Afzal R, Syal RP, Natarajan MK. Safety and feasibility of early hospital discharge in ST-segment elevation myocardial infarction—A prospective and randomized trial in low-risk primary percutaneous coronary intervention patients (the Safe-Depart Trial) Am Heart J. 2010;159:117.e111–117.e116. doi: 10.1016/j.ahj.2009.10.024. [DOI] [PubMed] [Google Scholar]
- 11.Krumholz HM, Herrin J, Miller LE, Drye EE, Ling SM, Han LF, Rapp MT, Bradley EH, Nallamothu BK, Nsa W. Improvements in door-to-balloon time in the United States, 2005 to 2010. Circulation. 2011 doi: 10.1161/CIRCULATIONAHA.111.044107. CIRCULATIONAHA. 111.044107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khot UN, Johnson ML, Ramsey C, Khot MB, Todd R, Shaikh SR, Berg WJ. Emergency department physician activation of the catheterization laboratory and immediate transfer to an immediately available catheterization laboratory reduce door-to-balloon time in ST-elevation myocardial infarction. Circulation. 2007;116:67–76. doi: 10.1161/CIRCULATIONAHA.106.677401. [DOI] [PubMed] [Google Scholar]
- 13.Mentias A, Raza MQ, Barakat AF, Youssef D, Raymond R, Menon V, Simpfendorfer C, Franco I, Ellis S, Tuzcu EM, Kapadia SR. Effect of Shorter Door-to-Balloon Times Over 20 Years on Outcomes of Patients With Anterior ST-Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention. Am J Cardiol. 2017;120:1254–1259. doi: 10.1016/j.amjcard.2017.07.006. [DOI] [PubMed] [Google Scholar]
- 14.Cruden NL, Teh CH, Starkey IR, Newby DE. Reduced vascular complications and length of stay with transradial rescue angioplasty for acute myocardial infarction. Catheter Cardiovasc Interv. 2007;70:670–675. doi: 10.1002/ccd.21182. [DOI] [PubMed] [Google Scholar]
- 15.Caputo RP, Tremmel JA, Rao S, Gilchrist IC, Pyne C, Pancholy S, Frasier D, Gulati R, Skelding K, Bertrand O. Transradial arterial access for coronary and peripheral procedures: executive summary by the Transradial Committee of the SCAI. Catheter Cardiovasc Interv. 2011;78:823–839. doi: 10.1002/ccd.23052. [DOI] [PubMed] [Google Scholar]
- 16.Joyal D, Bertrand OF, Rinfret S, Shimony A, Eisenberg MJ. Meta-Analysis of Ten Trials on the Effectiveness of the Radial Versus the Femoral Approach in Primary Percutaneous Coronary Intervention. Am J Cardiol. 2012;109:813–818. doi: 10.1016/j.amjcard.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 17.Hill J, Hampton J, Mitchell J. A randomised trial of home-versus-hospital management for patients with suspected myocardial infarction. Lancet. 1978;311:837–841. doi: 10.1016/s0140-6736(78)90190-3. [DOI] [PubMed] [Google Scholar]
- 18.Tickoo S, Bhardwaj A, Fonarow GC, Liang L, Bhatt DL, Cannon CP. Relation between hospital length of stay and quality of care in patients with acute coronary syndromes (from the American Heart Association's get with the guidelines - Coronary artery disease data set) Am J Cardiol. 2016;117:201–205. doi: 10.1016/j.amjcard.2015.10.027. [DOI] [PubMed] [Google Scholar]
- 19.Jirmár R, Widimský P, Capek J, Hlinomaz O, Groch L. Next day discharge after successful primary angioplasty for acute ST elevation myocardial infarction. Int Heart J. 2008;49:653–659. doi: 10.1536/ihj.49.653. [DOI] [PubMed] [Google Scholar]
- 20.Faridi KF, Peterson ED, McCoy LA, Thomas L, Enriquez J, Wang TY. Timing of first postdischarge follow-up and medication adherence after acute myocardial infarction. JAMA Cardiology. 2016;1:147–155. doi: 10.1001/jamacardio.2016.0001. [DOI] [PubMed] [Google Scholar]
- 21.Daugherty SL, Ho P, Spertus JA, et al. Association of early follow-up after acute myocardial infarction with higher rates of medication use. Arch Intern Med. 2008;168:485–491. doi: 10.1001/archinte.168.5.485. [DOI] [PubMed] [Google Scholar]
- 22.Andrejak M, Andrejak M-T, Osterman G. Enalapril, captopril, and cough. Arch Intern Med. 1988;148:249–249. [PubMed] [Google Scholar]
- 23.Kaufman J, Casanova JE, Riendl P, Schiuder DP. Bronchial Hyperreactivity and Cough due to Angiotensin-converting Enzyme Inhibitors. Chest. 1989;95:544–548. doi: 10.1378/chest.95.3.544. [DOI] [PubMed] [Google Scholar]
- 24.Karabulut A, Cakmak M, Uzunlar B, Bilici A. What is the optimal length of stay in hospital for ST elevation myocardial infarction treated with primary percutaneous coronary intervention? Cardiol J. 2011;18:378–384. [PubMed] [Google Scholar]
- 25.Amsterdam EA, Wenger NK, Brindis RG, Casey DE, Ganiats TG, Holmes DR, Jaffe AS, Jneid H, Kelly RF, Kontos MC. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes. Circulation. 2014 doi: 10.1016/j.jacc.2014.09.017. CIR. 0000000000000134. [DOI] [PubMed] [Google Scholar]
- 26.Barnett PG, Chen S, Boden WE, Chow B, Every NR, Lavori PW, Hlatky MA. Cost-Effectiveness of a Conservative, Ischemia-Guided Management Strategy After Non-Q-Wave Myocardial Infarction: Results of a Randomized Trial. Circulation. 2002;105:680–684. doi: 10.1161/hc0602.103584. [DOI] [PubMed] [Google Scholar]