Abstract
Background
Interest in surgical careers among medical students has declined over the past decade. Multiple explanations have been offered for why top students are deterred or rejected from surgical programs, though no consensus has emerged.
Methods
We conducted a review of the literature to better characterize what factors affect the pursuit of a surgical career. We searched PubMed and EMBASE and performed additional reference checks. Agency for Healthcare Research and Quality (AHRQ) and Newcastle–Ottawa Education scores were used to evaluate the included data.
Results
Our search identified 122 full-text, primary articles. Analysis of this evidence identified 3 core concepts that impact surgical career decision-making: gender, features of surgical education, and student “fit” in the culture of surgery.
Conclusion
Real and perceived gender discrimination has deterred female medical students from entering surgical careers. In addition, limited exposure to surgery during medical school and differences between student and surgeon personality traits and values may deter students from entering surgical careers. We suggest that deliberate and visible effort to include women and early-career medical students in surgical settings may enhance their interest in carreers in surgery.
Abstract
Contexte
On constate que l’intérêt pour une carrière en chirurgie a décliné chez les étudiants en médecine depuis une dizaine d’années. Plusieurs raisons ont été invoquées pour expliquer le désintérêt des étudiants talentueux à l’égard des programmes de chirurgie ou leur rejet de ces programmes, sans qu’on en arrive à un consensus.
Méthodes
Nous avons procédé à une revue de la littérature afin de mieux cerner les facteurs qui influent sur la poursuite d’une carrière de chirurgien. Nous avons interrogé les bases de données PubMed et Embase et procédé à des vérifications additionnelles des références. Nous avons utilisé les scores de l’Agency for Healthcare Research and Quality (AHRQ) et l’échelle Newcastle–Ottawa pour l’éducation afin d’analyser les données retenues.
Résultats
Notre recherche a permis de recenser 122 articles de fond en texte intégral. Leur analyse a mis au jour 3 facteurs clés qui influent sur les prises de décisions concernant une carrière en chirurgie: le sexe, les caractéristiques de la formation chirurgicale et la concordance entre le profil de l’étudiant et la culture du milieu chirurgical.
Conclusion
La discrimination sexuelle réelle et perçue a détourné des étudiantes de la chirurgie comme perspective de carrière. De plus, l’exposition limitée à la chirurgie durant les études de médecine et les différences entre les traits de personnalité et les valeurs des étudiants et des chirurgiens peuvent dissuader les étudiants d’entreprendre une carrière en chirurgie. Selon nous, des efforts délibérés et tangibles d’intégration des femmes et des futurs médecins au domaine chirurgical contribueraient à accroître leur intérêt pour cette spécialité.
Declining interest in surgical careers has been of concern for more than a decade.1–4 The Canadian Resident Matching Service (CaRMS) surgical specialties have had a reduction in applications ranking surgical programs as first choice from 24.7% in 1998 to 21.7% in 2006 to 17.2% in 2016, whereas an increasing proportion of applications are to “controlled lifestyle” specialties, such as radiology, emergency medicine and anesthesiology.5–7 This is true even in historically competitive surgical specialties, such as plastic surgery.8 With increasing match participation and stable interest in surgical careers, the quota of surgical residencies continues to be filled, but this should not be equated with increasing interest in the profession. Proportionally fewer Canadian students are applying to surgical residencies, but the rapid decline in the number of available surgical positions over the past 5 years has ensured that programs are filled.7 In the United States there has been no change in the number of available surgical positions or in the number of applications to surgical residencies over the past 5 years despite increasing numbers of total participants in the National Resident Matching Program (NRMP) Match; application to surgical residency in the United States has reduced proportionally to the overall increase in match participation.9 A 2005 survey of graduating U.S. medical students found that 45% of first-year medical students were interested in a surgical career, whereas only 7% of graduating students were matched to surgical residencies; findings suggested that features yet unknown during the course of medical school made surgery unpopular.3
Effort has been made to respond to the apparent decreased interest in surgical careers among medical students by preferentially selecting high-achieving, resilient and hard-working individuals during the residency selection process. Despite this effort, residency selection is imperfect, and the quality of future surgeons is not reliably predicted by residency applications.10,11 One alternative solution to the decreased number of applications to surgical residency programs from strong candidates is to encourage early interest in surgery among medical students. We hypothesize that potentially strong candidates for surgical residency lose interest in a surgical career during medical school and subsequently do not apply for surgical residency positions. A thorough understanding of the features that attract or deter medical students from surgery must be obtained in order to expand the applicant pool for surgical training programs.
We conducted a systematic review of the published literature to clarify which factors deter students from pursuing a surgical career. The goal of this review was to facilitate active recruitment of medical students who may ultimately be interested in a surgical career, especially those who would not otherwise have considered surgery seriously.
Methods
This study was conducted according to the PRISMA 2009 Checklist recommendations for systematic review.12 We performed a literature search in December 2016 using PubMed with the search terms “perception of surgical career,” “surgical residency selection,” or “surgery elective undergraduate education.” We conducted a search of EMBASE using the the medical subject headings (MeSH) [focus] “Decision making,” “Surgery,” and [explode] “Medical education.” Manual reference checks of publications were performed to supplement the electronic search. We selected this strategy in an effort to identify components of the medical education processes as well as the decision-making processes in which we expect career decisions to be made. A broad search strategy was chosen owing to the variation in terminology surrounding this topic.
For the purpose of this study, medical trainees were defined as individuals in medical school or internship years who were not graduated doctors and who required supervision during clinical encounters. We considered surgical career selection to describe the decision of medical students to apply for residency training in a surgical specialty. Published randomized controlled trials and observational studies investigating trainee exposure to and interest in surgery were eligible for inclusion. No language or publication date restrictions were imposed. We included studies from all surgical specialties, including general surgery, general surgical subspecialities, vascular surgery, plastic and reconstructive surgery, neurosurgery, orthopedic surgery, otolaryngology, obstetrics and gynecology, and ophthalmology. Studies describing medical student rationale for specialty selection outside of surgery were also included. Studies that did not address our research question were excluded. Studies identified by the search strategy were initially screened by title and abstract. Full text review of and data collection from all studies meeting our inclusion criteria was performed independently by a single reviewer (J.K.P.) using a standard data extraction form.
We evaluated strength of evidence qualitatively according to the Agency for Healthcare Research and Quality (AHRQ) checklist and using the Newcastle–Ottawa Scale adapted for cross-sectional studies.13,14 The AHRQ assessment criteria grade quality of evidence based on study design, directness, precision and consistency; quality is graded as low, moderate, or high according to satisfaction of criteria in each of these categories. Directness describes whether the measured outcomes of included studies correspond to the outcome of interest for the review. Precision is defined as the degree of certainty for the included studies, and is impacted by sample size. Consistency describes whether the included studies find similar or dissimilar results. To meet criteria for high-quality evidence, a body of evidence must be largely prospective, randomized controlled trials with low risk of bias and that satisfy criteria for directness, precision and consistency. Although this tool tends to be used to assess clinical interventions, its application is useful for the evaluation of the impact certain interventions have in health care programs; we consider clinical placements and clinical training interventions among these. The Newcastle–Ottawa Scale awards studies a maximum of 10 points through the evaluation of selection, comparability and outcome criteria. Selection describes the procedures outlined in a paper to study an appropriate population. Comparability refers to how well differences between groups are accounted for. Outcome criteria refer to the risk of bias conferred by the described qualitative and quantitative assessments used in a study. Typically these scores are presented for each included paper, but for simplicity of presentation we chose to present the mean scores.
Results
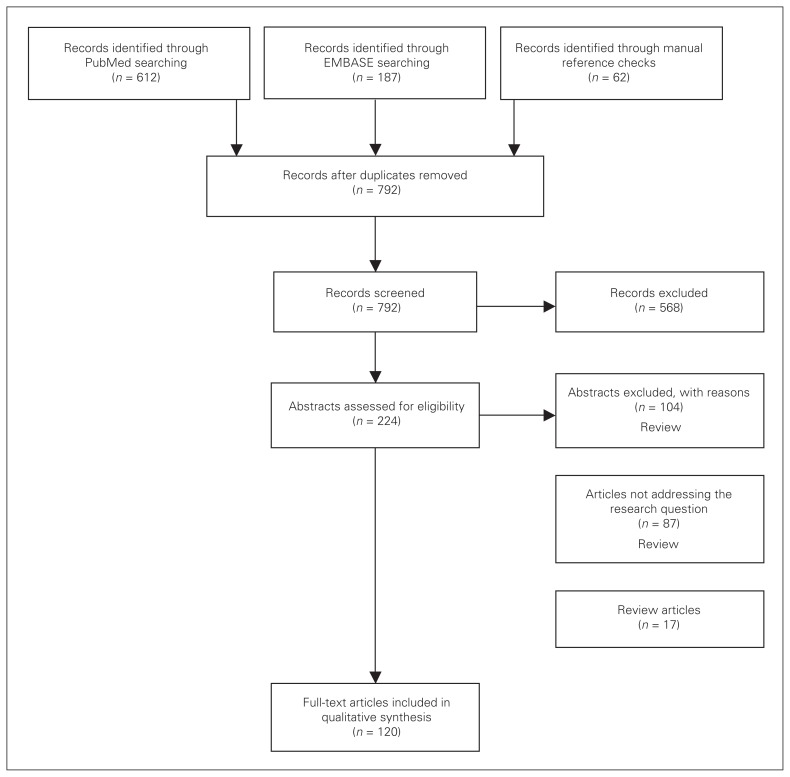
Our PubMed search strategy identified 612 studies, the EMBASE search identified 186 studies, and our manual search of reference lists identified 62 studies. Once duplicates were removed, a total of 792 titles were available for screening. Screening excluded 568 studies that were not related to our research question. Full text review of the remaining 224 studies resulted in further exclusion of 104: 87 studies were excluded because they did not address our research question, and 17 reviews were excluded because they did not meet our study design criteria. In total, 120 studies were included in our analysis. Most included studies used a cross-sectional design, with limited evidence coming from prospective studies. These results are summarized in Figure 1.
Fig. 1.
Study selection process.
Impact of gender
Gender discrimination
We chose to discuss “gender” to include the experiences of students identifying and expressing a gender different than their biological sex. Our search identified studies that used either term but that intended to communicate gender identity, and we have included them all using “gender” as the preferred term for this paper. Our search identified 13 cross-sectional studies discussing gender discrimination.15–27 An AHRQ grade of moderate strength was awarded to this body of evidence, with a mean Newcastle–Ottawa score of 6.9. The experience of gender discrimination is reported across all medical specialties, and is not unique to surgery.22 However, the perception of gender bias is frequently reported during surgical experiences and has been shown to decrease interest in the pursuit of further surgical training.15–27 This perceived culture in surgery has been described as “a gender-specific deterrence to a career in surgery for women.”16 Six large-scale surveys of medical trainees independently reported that a significant portion of female medical students experienced gender discrimination (68%–96%) and that this experience of bias influenced their career decisions.15,17–20,28 Significantly fewer female than male medical students considered surgical careers and ranked surgical residencies.20,28 In contrast, male medical students in these studies reported significantly less harassment than female medical students, and this correlated to greater interest in surgical careers.18,20,28
Gender bias was also reported as a barrier for career advancement in 4 surveys of surgeons and surgical residents, and 1 survey of 100 staff cardiothoracic surgeons reported a significant income difference between men and women and that surgeons of either gender were significantly less likely to encourage women to enter surgical careers.21,23,24,27
Lack of same-gender role models
The lack of female role models is also a frequently reported explanation for reduced interest in surgery among female students. Eleven cross-sectional studies studying the impact of same-gender role models were identified in our search.19,22,29–37 An AHRQ grade of moderate strength was awarded to this body of evidence, with a mean Newcastle–Ottawa score of 7.5. It has been shown that residency programs appearing to lack diversity are unappealing to women and other self-reported underrepresented minorities.22 Furthermore, it has been shown that female students are significantly more likely to enter specialties with a higher proportion of women.29,37 In 1 survey, as few as 35% of female medical students could identify a mentor during surgical clerkship, and a different study showed that among women who did have a mentor, 90% had a male rather than a female mentor.35,36 These findings suggest that female students may be deterred from surgical residency because there has historically been fewer women in surgery and there may be a dearth of female colleagues.
Impact of child care, pregnancy, and lifestyle considerations for women
In the studies we identified, women cited lifestyle among their most important considerations during career decision-making.34,38 The opportunity for women to lead a balanced lifestyle was reported by 10 studies to be an influential factor when deciding whether or not to pursue a surgical career.17,28,34,38–44 An AHRQ grade of moderate strength was awarded to this body of evidence, with a mean Newcastle–Ottawa score of 6.8. Among these, 4 studies reported that female students perceived general surgery to be incompatible with having children or a rewarding family life, despite 2 studies showing female staff surgeon satisfaction with their capacity to balance work and family life.17,40,42–44
Three studies identified in our search commented explicitly on maternity leave and support for child care, finding that limited or no infrastructure exists for residents who have children during training.28,39,41 One of these studies was Canadian and the other 2 were American.
Impact of surgical education
Preclerkship exposure
Exposure to surgery before students enter their clinical years has been shown to influence interest in surgery by 10 of the studies identified by our search strategy, 3 of which were cross-sectional and 7 of which were cohort studies.45–54 An AHRQ grade of moderate strength was awarded to this body of evidence, with a mean Newcastle–Ottawa score of 6.6. The results from these studies were uniformly positive; following exposure to surgery during the preclinical years, students expressed greater confidence that surgery allows for work–life balance and meaningful change in patients’ lives.
Clinical exposure
Our literature search identified 21 studies that assessed the association between clinical exposure and student interest in surgery. An AHRQ grade of moderate strength was awarded to this body of evidence, with a mean Newcastle–Ottawa score of 7.6. Of these studies, 11 showed that clinical exposure improves student knowledge of and interest in surgery.55–65
Clerkship changed student perception of surgery and the surgical lifestyle in 6 of the studies we identified.66–71 This has a variable impact on student interest in a surgical career. Four studies reported that surgical clerkship increases student interest in surgical topics and shows the potential for work–life balance, thus increasing student interest in these careers.66,69–71 However, 2 studies reported that clerkship reduced interest in surgery. One survey of African medical students showed that an anesthesiology rotation reduced interest in the career, with students citing that it clarified how this career did not achieve student goals.67 The other study by Zuccatto and colleagues68 showed that clinical exposure reduced student interest in neurosurgery from 25% to 10%, as students came to appreciate the workload of neurosurgeons.
The impact of surgical simulation training on developing medical student interest in surgery was assessed in 4 studies identified by our search strategy.72–75 Surgical simulation training improved student experience of surgical clerkship in all of these studies and improved interest in surgery in 2 studies.73,74 Galiñanes and colleagues72 found that orientation to basic laparoscopy can benefit a student’s clerkship experience, but does not improve student interest in surgery.
Global health exposure
Global health electives in surgery are an opportunity for medical students to develop clinical experience and surgical skills in unique, often resource-limited environments. Our literature search identified 4 papers assessing medical student interest in surgery following international surgery electives.76–79 An AHRQ grade of low strength was awarded to this body of evidence, with a mean Newcastle–Ottawa score of 4.8. In these reports, a small group of medical students participated in supervised medical electives and were interviewed about their experiences. It was shown that these unique international experiences did not impair students’ ability to meet the same curricular objectives as their peers at a home site.76 These experiences were shown to provide a culturally broader experience and greater clinical responsibility than what was afforded to students at their home institution, though no direct comment on the impact this had on student interest in a surgical career was reported.76–79
Impact of student fit in surgical culture
Surgical lifestyle
The surgical lifestyle and its impact on student pursuit of surgical careers was the most heavily studied association, having been discussed in 31 of the studies identified in our search.3,35,66,68,71,80–105 An AHRQ grade of moderate strength was awarded to this body of evidence, with a mean Newcastle–Ottawa score of 7.9. Among these, 22 studies commented explicitly on the weight that students place on duration of training and work–life balance when making career decisions.3,35,66,68,71,80–87,89,91,98–102,104,105 Lifestyle considerations included prolonged work hours, the perceived barrier to achieving work–life balance and the nature of patient interactions in surgery. These survey data showed that most medical students did not see their lives as compatible with surgery, and therefore considered the career-focused surgical lifestyle their primary deterrent from surgical specialties.
In contrast, medical students interested in surgery tended to consider lifestyle less important when making career decisions. Nine studies supported the theory that students who identify as surgeons prioritized their interest in surgical topics over value of a controlled lifestyle.88,90,92–97,103
Efforts to enhance student interest in surgery by putting in place lifestyle modifications have had mixed success. Work hour restrictions have been shown to improve students’ experience of their surgical rotations and to enhance their interest in surgical careers.85,88,104 One study showed that work hour restrictions had an impact on clerkship experience and interest in surgical careers.104 In 2 studies of medical students completing surgical clerkships, it has been shown that these duty hour limitations produce significantly more favourable impressions of surgical lifestyles, though no statistically significant improvement in student interest in surgery was observed with the implementation of restricted work hours.85,88 In contrast, exposing medical students to community and private practice surgery has resulted in improved clerkship experience as well as enhanced interest in surgical careers, as shown by 2 studies included in our review.60,71
Mentorship
The presence of a role model in surgery was reported in 26 studies to be a significant, positive influence on surgical career decision-making.3,31,32,36,49,56,61,74,91,96,97,106–120 An AHRQ grade of moderate strength was awarded to this body of evidence, with a mean Newcastle–Ottawa score of 7.8. These studies clearly showed that medical students had significantly greater interest in surgery when they were partnered with a surgical mentor. The absence of such a mentor has been shown to have a deterrent effect on student interest in surgery.
Three studies in our review discussed the role of residents as surgical mentors.106,107,115 These studies reported a positive association between exposure to surgical residents and interest in a surgical career. The authors of these studies suggested that residents are particularly effective mentors for medical students because of the extent to which students and residents interact.106,107,115
Our search strategy revealed only 1 study that assessed the impact of mentorship outside of clinical experience. Day and colleagues49 reported that a mentorship program for 18 students in preclinical years of medical school was successful at improving student interest in surgical careers.
Personality type
Our search strategy identified 6 studies that sought to identify particular personality traits that predispose an individual to interest in surgery.121–126 All of these studies reported that individuals interested in surgery were significantly more extroverted and conscientious than the general population and significantly less impulsive.121–126 Inconsistency among studies existed when reporting neuroticism in the surgical personality.122,125,126 Emotional intelligence was not found to be useful in differentiating medical students interested in surgical versus medical specialties.127
Our review identified 5 studies that commented on how prestige and financial reward factored into career decisions among medical students.96,128–131 These studies reported that medical students who valued prestige, financial gain and academic ambition tended to pursue careers in surgery more frequently than their counterparts, suggesting a personality that is more drawn to surgery. Furthermore, 1 study reported that medical students considered surgery to be the medical career with the greatest potential for prestige, skill and knowledge.128
An AHRQ grade of low strength was awarded to these studies, with a mean Newcastle–Ottawa score of 7.8.
Discussion
Gender discrimination among medical students and surgeons has been discussed in the surgical literature for more than 20 years as an explanation for gender imbalances in surgical specialties. During this time, changing gender roles in society and the changing role of surgeons in the health care team has resulted in an increased inclusion of women in surgery. However, many of the studies included in this review are dated and do not reflect these changes. Furthermore, despite this progress, a position statement from the Association of Women Surgeons (AWS) expresses ongoing concern regarding gender bias causing income inequality.132 Our interpretation of the literature is consistent with the findings of the AWS that gender discrimination has deterred female interest in surgery. We propose that historical and ongoing gender discrimination has resulted in under-representation of women in surgery, especially in leadership roles and academia. This under-representation may be perceived as a “glass ceiling” hindering career development of women in surgery, thereby discouraging more women from considering careers in surgery. As effort has been made to improve representation of women in surgery, we expect this to change, but based on our findings we recommend that ongoing effort be made to demonstrate inclusion and equal opportunity within surgery.
An important means of demonstrating inclusivity and facilitating recruitment of female medical students is the explicit communication of support to those students interested in having a family; it is important to medical students that the surgical community be perceived as welcoming of diversity, encouraging of women surgeons and supportive of parental leave. Our recommendations therefore echo those of Mayer41: formal policies regarding diversity and child care support during residency should exist to ensure that students considering a family are not deterred from pursuing a career in surgery.
The perceived inability of surgeons to maintain work–life balance was another frequently reported deterrent to pursuing surgical careers and has been cited as a cause for concern among surgical training programs. Certain non-modifiable features of surgical careers, such as night call and early morning rounds, can deter students from surgery, but the data in this review suggest that clerkship may improve interest in surgical careers by dispelling the myth that surgery precludes work–life balance.68,71,118 Notably, clerkship rotations at a community hospital resulted in medical students feeling reassured that surgeons can maintain work–life balance.60,71 We recommend making an effort to ensure that work–life balance is an additional learning objective in surgical clerkship.
The data in our review emphasize the importance of early interest in surgery among medical students, as those students who have built an intellectual interest in surgery are not discouraged by the busy surgical lifestyle or the challenges surgeons face in finding work–life balance.45–54,80,82,83,85,88 The importance of exposure to surgery early in training is further supported by a study by Sallee and colleagues,128 which showed that medical student impressions of a specialty form before adequate clinical exposure in that specialty is obtained. These findings, together with ours, suggest that decisions about specialties of interest are formed during the preclerkship years. We recommend that medical students be given introductory exposure to surgery before their clerkship years in order to build early interest in surgical careers.
In addition to recruitment of medical students who are not discouraged by the busy surgical lifestyle, recruitment could be further enhanced by wellness initiatives. Surgeon wellness during residency and throughout a surgical career has become a priority, and this may encourage interest in surgery among students who are undecided.133,134 One approach to ensuring wellness among surgical trainees is the restriction of duty hours, which was found in our review to have a beneficial impact on student experience of surgery and mixed impact on student pursuit of a career in surgery.85,88,104 However, duty hour restriction is controversial, and results from prominent studies, such as the FIRST trial, illuminate the nuanced balance between duty hour policies and surgical trainee well-being.135 We cannot make recommendations based on our review regarding duty hour restrictions.
Alternative wellness initiatives and the increasing emphasis on preventing burnout among surgeons reflects a culture shift that may allow for a more balanced perception of surgical careers.133 The Royal College of Physicians and Surgeons of Canada has begun implementation of the Competence By Design (CBD) framework, which emphasizes gradual increases in responsibility as trainees advance in their knowledge and ability. Among the goals of this new curriculum is to provide a more balanced approach to exam preparation and to ensure that trainees are not held to expectations beyond their ability.136 We hypothesize that discussion of wellness during clinical training and the introduction of greater balance in training curricula will expose this emphasis on wellness to those clerks who are yet undecided about a career in surgery and may enhance student interest in surgery.
Our review identified mentorship as having a positive impact on student interest in surgical careers. Some data suggested that resident mentors had a particularly beneficial impact on student clerkship experiences, as residents work more closely with students than staff surgeons do.106,107,115 Furthermore, mentorship of female and under-represented minority medical students has been shown to lead to similar increases in student interest in surgical careers.19,22,29–37,137 Program diversity is an important consideration for medical students, and we posit that mentorship may allow for honest discussion of diversity in surgery and can also create a more welcoming environment for medical students who see themselves as “outsiders” in surgical settings.22,137
Mentorship in surgery may also be beneficial because it allows students to become familiar with the personalities of potential future colleagues. The concept of a surgical personality was first developed by McGreevy and Wiebe,126 who identified similarities in trait variance on personality testing among surgical residents. Students who are extroverted, ambitious and motivated by the prestige of surgical work may be good candidates for surgical training.121–126,96,128–131 However, bias may exist in studies of a surgical personality among medical students: students interested in surgery may construct a value system for themselves based on that of the surgeons they know, thereby promoting personality traits unique to certain surgeons that may or may not reflect the value system inherent to surgery.
A common feature of the studies discussing the importance of mentorship is that a mentor relationship was established during clinical rotations.3,31,32,36,49,56,61,74,91,96,97,106–120 Clinical experience is known to have a significant impact on career decisions, but the mentorship during exciting clinical opportunities may lead to an especially transformative experience during surgical clerkship. We encourage that mentor relationships be established with medical students whenever possible and that same-gender mentors are more favourable if available.
Limitations
Our outcome of interest — student interest in surgical careers — has not been shown to reliably predict pursuit of a surgical career. Only 1 study captured by our search strategy assessed match rates to surgical residency in students who reported interest in surgery, and this was not the primary outcome of the study.60 Student interest in surgery was selected a priori as our outcome of interest because it was thought to best reflect the attitudes of medical students in the process of making career decisions. Other outcomes, such as match rates to surgical residency, would not as readily report the impact that certain factors have on career decision-making and are affected by external factors, such as changes to program funding and the availability of surgical training positions.
Most studies identified in our search were cross-sectional observational studies, and many were dated. Applying these older papers to contemporary surgery is problematic, because the climate of surgery is dynamic and the evolution of culture in surgery may not yet be reflected in the literature. Because these limited-quality data were the best available, as identified by our search strategy, it is clear that there is an absence of recent, high-quality studies assessing surgical interest among medical students. We consider our results in the context of largely dated, survey-based evidence.
Strength of evidence for a heterogeneous body of largely dated, cross-sectional data, such as that assessed in our review, is difficult. Few epidemiologic tools exist to grade the strength of evidence from cross-sectional studies in a review, so we are limited in our ability to objectively grade the quality of evidence included in our review. We have applied 2 literature-validated tools for grading strength of evidence in health care programs, but these are not typically used in the context of career decision-making.13,14 Our use of multiple tools validated for different contexts attempts to overcome the limitations of using a single tool on this challenging body of evidence.
The studies that identified an association between clinical exposure to surgery and an interest in a surgical career were limited inasmuch as clerkship experiences are variable, and bias existed in the survey design.55–65 Specifically, students with early interest in surgery were more likely to seek out surgical experiences and were more inclined to report a positive clerkship experience, thereby artificially strengthening the association between exposure and interest.138
Conclusion
The goal of this review was to clarify which deterrents to entering surgical careers were perceived by medical students. Real and perceived gender discrimination detered female medical students from entering surgical careers. In addition, limited exposure to surgery and the operating room during medical school and real and perceived differences between student and surgeon personality traits and values may deter students from entering surgical careers. Some evidence identifies a unique surgical personality that could be identified in medical students, but the application of this to recruitment efforts has not yet been validated in the literature. Evidence supports the matching of students with surgical mentors to encourage surgical careers. Those students ambivalent toward careers in surgery may have enhanced interest in surgical careers if they are mentored, included in clinical work from early stages of training, and made to feel part of the surgical team; we suggest that faculty and residents consider these factors when working with medical students.
Footnotes
See the related commentary by Acai and colleagues on p. 6
Competing interests: None declared.
Contributors: All authors designed the study. J. Peel acquired and analyzed the data. J. Peel and N. Alkhamesi wrote the article, which all authors reviewed and approved for publication.
References
- 1.Bland KI, Isaacs G. Contemporary trends in student selection of medical specialties. Arch Surg. 2002;137:259–67. doi: 10.1001/archsurg.137.3.259. [DOI] [PubMed] [Google Scholar]
- 2.Niethard M, Donner S, Depeweg D, et al. Promoting the next generation — What can we improve? Unfallchirurg. 2013;116:21–4. doi: 10.1007/s00113-012-2301-1. [DOI] [PubMed] [Google Scholar]
- 3.Brundage SI, Lucci A, Miller CC, et al. Potential targets to encourage a surgical career. J Am Coll Surg. 2005;200:946–53. doi: 10.1016/j.jamcollsurg.2005.02.033. [DOI] [PubMed] [Google Scholar]
- 4.Marschall JG, Karimuddin AA. Decline in popularity of general surgery as a career choice in North America: review of postgraduate residency training selection in Canada, 1996–2001. World J Surg. 2003;27:249–52. doi: 10.1007/s00268-002-6642-8. [DOI] [PubMed] [Google Scholar]
- 5.Pukite J, Pukite P. Modeling for reliability analysis: Markov modeling for reliability, maintainability, safety, and supportability analyses of complex systems. Hoboken (NJ): Wiley-IEEE Press; 1998. [Google Scholar]
- 6.Scott I, Gowans M, Wright B, et al. Determinants of choosing a career in surgery. Med Teach. 2012;33:1011–7. doi: 10.3109/0142159X.2011.558533. [DOI] [PubMed] [Google Scholar]
- 7.Service CRM. Canadian Residency Matching Service Report. Ottawa (ON): CaRMS; 2016. [Google Scholar]
- 8.Austin RE, Wanzel KR. Exposure to plastic surgery during undergraduate medical training: a single-institution review. Plast Surg (Oakv) 2015;23:43–7. doi: 10.4172/plastic-surgery.1000903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Resident Matching Program. National Resident Matching Program, Results and Data. Washington (DC): NRMP; 2017. [Google Scholar]
- 10.Papp KK, Polk HC, Jr, David Richardson J. The relationship between criteria used to select residents and performance during residency. Am J Surg. 1997;173:326–9. doi: 10.1016/s0002-9610(96)00389-3. [DOI] [PubMed] [Google Scholar]
- 11.Snadden D. Expanding undergraduate medical education in British Columbia: a distributed campus model. CMAJ. 2005;173:589–90. doi: 10.1503/cmaj.050439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berkman ND, Lohr KN, Ansari M, et al. Grading the strength of a body of evidence when assessing health care interventions for the Effective Health Care Program of the Agency for Healthcare Research and Quality. An Update. Methods Guide for Effectiveness and Comparative Effectiveness Reviews [Internet] Rockville (MD): Agency for Healthcare Research and Quality; 2008. [PubMed] [Google Scholar]
- 14.Herzog R, Álvarez-Pasquin MJ, Díaz C, et al. Are healthcare workers’ intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health. 2013;13:1141. doi: 10.1186/1471-2458-13-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Richardson HC, Redfern N. Why do women reject surgical careers? Ann R Coll Surg Engl. 2000;82:290–3. [PubMed] [Google Scholar]
- 16.Gargiulo DA, Hyman NH, Hebert JC. Women in surgery: Do we really understand the deterrents? Arch Surg. 2006;141:405–7. doi: 10.1001/archsurg.141.4.405. [DOI] [PubMed] [Google Scholar]
- 17.Park J, Minor S, Taylor RA, et al. Why are women deterred from general surgery training? Am J Surg. 2005;190:141–6. doi: 10.1016/j.amjsurg.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 18.Lillemoe KD, Ahrendt GM, Yeo CJ, et al. Surgery — still an “old boys’ club”? Surgery. 1994;116:255–9. [PubMed] [Google Scholar]
- 19.Fitzgerald JEF, Tang S-W, Ravindra P, et al. Gender-related perceptions of careers in surgery among new medical graduates: results of a cross-sectional study. Am J Surg. 2013;206:112–9. doi: 10.1016/j.amjsurg.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 20.Stratton TD, McLaughlin MA, Witte FM, et al. Does students’ exposure to gender discrimination and sexual harassment in medical school affect specialty choice and residency program selection? Acad Med. 2005;80:400–8. doi: 10.1097/00001888-200504000-00020. [DOI] [PubMed] [Google Scholar]
- 21.Cochran A, Hauschild T, Elder WB, et al. Perceived gender-based barriers to careers in academic surgery. Am J Surg. 2013;206:263–8. doi: 10.1016/j.amjsurg.2012.07.044. [DOI] [PubMed] [Google Scholar]
- 22.Ku MC, Li YE, Prober C, et al. Decisions, decisions: how program diversity influences residency program choice. J Am Coll Surg. 2011;213:294–305. doi: 10.1016/j.jamcollsurg.2011.04.026. [DOI] [PubMed] [Google Scholar]
- 23.Dresler CM. Experiences of women in cardiothoracic surgery. Arch Surg. 1996;131:1128. doi: 10.1001/archsurg.1996.01430230010002. [DOI] [PubMed] [Google Scholar]
- 24.Schroen AT, Brownstein MR, Sheldon GF. Women in academic general surgery. Acad Med. 2004;79:310–8. doi: 10.1097/00001888-200404000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Schroeder JE, Zisk-Rony RY, Liebergall M, et al. Medical students’ and interns’ interest in orthopedic surgery: the gender factor. J Surg Educ. 2014;71:198–204. doi: 10.1016/j.jsurg.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 26.Calkins EV, Willoughby TL, Arnold LM. Women medical students’ ratings of the required surgery clerkship: implications for career choice. J Am Med Womens Assoc. 1972;1992:58–60. [PubMed] [Google Scholar]
- 27.Hill E, Vaughan S. The only girl in the room: how paradigmatic trajectories deter female students from surgical careers. Med Educ. 2013;47:547–56. doi: 10.1111/medu.12134. [DOI] [PubMed] [Google Scholar]
- 28.Ferris LE, Mackinnon SE, Mizgala CL, et al. Do Canadian female surgeons feel discriminated against as women? CMAJ. 1996;154:21–7. [PMC free article] [PubMed] [Google Scholar]
- 29.Jagsi R, Griffith KA, DeCastro RA, et al. Sex, role models, and specialty choices among graduates of US medical schools in 2006–2008. J Am Coll Surg. 2014;218:345–52. doi: 10.1016/j.jamcollsurg.2013.11.012. [DOI] [PubMed] [Google Scholar]
- 30.Rohde RS, Wolf JM, Adams JE. Where are the women in orthopaedic surgery? Clin Orthop Relat Res. 2016;474:1950–6. doi: 10.1007/s11999-016-4827-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Neumayer L, Kaiser S, Anderson K, et al. Perceptions of women medical students and their influence on career choice. Am J Surg. 2002;183:146–50. doi: 10.1016/s0002-9610(01)00863-7. [DOI] [PubMed] [Google Scholar]
- 32.Hill JF, Yule A, Zurakowski D, et al. Residents’ perceptions of sex diversity in orthopaedic surgery. J Bone Joint Surg Am. 2013;95:e144-1–6. doi: 10.2106/JBJS.L.00666. [DOI] [PubMed] [Google Scholar]
- 33.Shortell CK, Cook C. Importance of gender-specific role models in vascular surgery. Vascular. 2008;16:123–9. doi: 10.2310/6670.2008.00024. [DOI] [PubMed] [Google Scholar]
- 34.McCord JH, McDonald R, Leverson G, et al. Motivation to pursue surgical subspecialty training: Is there a gender difference? J Am Coll Surg. 2007;205:698–703. doi: 10.1016/j.jamcollsurg.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 35.Ek EW, Ek ET, Mackay SD. Undergraduate experience of surgical teaching and its influence and its influence on career choice. ANZ J Surg. 2005;75:713–8. doi: 10.1111/j.1445-2197.2005.03500.x. [DOI] [PubMed] [Google Scholar]
- 36.Mayer KL, Perez RV, Ho HS. Factors affecting choice of surgical residency training program. J Surg Res. 2001;98:71–5. doi: 10.1006/jsre.2001.6143. [DOI] [PubMed] [Google Scholar]
- 37.Rouprêt M, Maggiori L, Lefevre JH. Upcoming female preponderance within surgery residents and the association of sex with the surgical career choice in the new millennium: results from a national survey in France. Am J Surg. 2011;202:237–42. doi: 10.1016/j.amjsurg.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 38.Gofin Y, Afek A, Derazne E, et al. A model for assessing the gap between physician residency demand and present status. Isr Med Assoc J. 2012;14:275–80. [PubMed] [Google Scholar]
- 39.Turner PL, Lumpkins K, Gabre J, et al. Pregnancy among women surgeons. Arch Surg. 2012;147:474–9. doi: 10.1001/archsurg.2011.1693. [DOI] [PubMed] [Google Scholar]
- 40.Ahmadiyeh N, Cho NL, Kellogg KC, et al. Career satisfaction of women in surgery: perceptions, factors, and strategies. J Am Coll Surg. 2010;210:23–8. doi: 10.1016/j.jamcollsurg.2009.08.011. [DOI] [PubMed] [Google Scholar]
- 41.Mayer KL. Childbearing and child care in surgery. Arch Surg. 2001;136:649. doi: 10.1001/archsurg.136.6.649. [DOI] [PubMed] [Google Scholar]
- 42.Field D, Lennox A. Gender in medicine: the views of first and fifth year medical students. Med Educ. 1996;30:246–52. doi: 10.1111/j.1365-2923.1996.tb00825.x. [DOI] [PubMed] [Google Scholar]
- 43.van Tongeren-Alers M, van Esch M, Verdonk P, et al. Are new medical students’ specialty preferences gendered? Related motivational factors at a Dutch medical school. Teach Learn Med. 2011;23:263–8. doi: 10.1080/10401334.2011.586928. [DOI] [PubMed] [Google Scholar]
- 44.Williams C, Cantillon P. A surgical career? The views of junior women doctors. Med Educ. 2000;34:602–7. doi: 10.1046/j.1365-2923.2000.00666.x. [DOI] [PubMed] [Google Scholar]
- 45.Zuckerman SL, Mistry AM, Hanif R, et al. Neurosurgery elective for preclinical medical students: early exposure and changing attitudes. World Neurosurgery. 2016;86:120–6. doi: 10.1016/j.wneu.2015.08.081. [DOI] [PubMed] [Google Scholar]
- 46.Khatib M, Soukup B, Boughton O, et al. Plastic surgery undergraduate training. Ann Plast Surg. 2015;75:208–12. doi: 10.1097/SAP.0000000000000058. [DOI] [PubMed] [Google Scholar]
- 47.Davis CR, O’Donoghue JM, McPhail J, et al. How to improve plastic surgery knowledge, skills and career interest in undergraduates in one day. J Plast Reconstr Aesthet Surg. 2010;63:1677–81. doi: 10.1016/j.bjps.2009.10.023. [DOI] [PubMed] [Google Scholar]
- 48.Cloyd J, Holtzman D, O’Sullivan P, et al. Operating room assist: surgical mentorship and operating room experience for preclerkship medical students. J Surg Educ. 2008;65:275–82. doi: 10.1016/j.jsurg.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 49.Day KM, Schwartz TM, Rao V, et al. Medical student clerkship performance and career selection after a junior medical student surgical mentorship program. Am J Surg. 2016;211:431–6. doi: 10.1016/j.amjsurg.2015.10.007. [DOI] [PubMed] [Google Scholar]
- 50.Teo LLS, Venkatesh SK, Goh PS, et al. A survey of local preclinical and clinical medical students’ attitudes towards radiology. Ann Acad Med Singapore. 2010;39:692–4. [PubMed] [Google Scholar]
- 51.Are C, Stoddard HA, Thompson JS, et al. The influence of surgical demonstrations during an anatomy course on the perceptions of first-year medical students toward surgeons and a surgical career. J Surg Educ. 2010;67:320–4. doi: 10.1016/j.jsurg.2010.07.016. [DOI] [PubMed] [Google Scholar]
- 52.Gawad N, Moussa F, Christakis GT, et al. Planting the “SEAD”: early comprehensive exposure to surgery for medical students. J Surg Educ. 2013;70:487–94. doi: 10.1016/j.jsurg.2013.03.006. [DOI] [PubMed] [Google Scholar]
- 53.George J, Combellack T, Lopez-Marco A, et al. Winning hearts and minds: inspiring medical students into cardiothoracic surgery through highly interactive workshops. J Surg Educ. 2017;74:372–6. doi: 10.1016/j.jsurg.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 54.Pulcrano ME, Malekzadeh S, Kumar A. The impact of gross anatomy laboratory on first year medical students’ interest in a surgical career. Clin Anat. 2016;29:691–5. doi: 10.1002/ca.22730. [DOI] [PubMed] [Google Scholar]
- 55.McLean TR, Haller CC, DeConink D. Investing in medical students: Which ones are worth a surgeon’s time? J Surg Educ. 2011;68:194–8. doi: 10.1016/j.jsurg.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 56.Johnson AL, Sharma J, Chinchilli VM, et al. Why do medical students choose orthopaedics as a career? J Bone Joint Surg Am. 2012;94:e78-1–9. doi: 10.2106/JBJS.K.00826. [DOI] [PubMed] [Google Scholar]
- 57.Cahan MA. Transforming the culture of surgical education. Arch Surg. 2011;146:830. doi: 10.1001/archsurg.2011.157. [DOI] [PubMed] [Google Scholar]
- 58.Crace PP, Nounou J, Engel AM, et al. Attracting medical students to surgical residency programs. Am Surg. 2006;72:485–90. [PubMed] [Google Scholar]
- 59.Binsaleh S, Al-Jasser A, Almannie R, et al. Attitude and perception of urology by medical students at the end of their medical school: an appraisal from Saudi Arabia. Urol Ann. 2015;7:211–20. doi: 10.4103/0974-7796.150511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cook MR, Yoon M, Hunter J, et al. A nonmetropolitan surgery clerkship increases interest in a surgical career. Am J Surg. 2015;209:21–5. doi: 10.1016/j.amjsurg.2014.08.027. [DOI] [PubMed] [Google Scholar]
- 61.Makama JG, Ameh EA. Does general surgery clerkship make a future career in surgery more appealing to medical students? Afr Health Sci. 2010;10:292–6. [PMC free article] [PubMed] [Google Scholar]
- 62.Singh N, Causey W, Brounts L, et al. Vascular surgery knowledge and exposure obtained during medical school and the potential impact on career decisions. J Vasc Surg. 2010;51:252–8. doi: 10.1016/j.jvs.2009.07.116. [DOI] [PubMed] [Google Scholar]
- 63.Ekenze SO, Ugwumba FO, Obi UM, et al. Undergraduate surgery clerkship and the choice of surgery as a career: perspective from a developing country. World J Surg. 2013;37:2094–100. doi: 10.1007/s00268-013-2073-y. [DOI] [PubMed] [Google Scholar]
- 64.Al-Heeti KNM, Nassar AK, Decorby K, et al. The effect of general surgery clerkship rotation on the attitude of medical students towards general surgery as a future career. J Surg Educ. 2012;69:544–9. doi: 10.1016/j.jsurg.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 65.Hagopian TM, Vitiello GA, Hart AM, et al. Does the amount of time medical students spend in the operating room during the general surgery core clerkship affect their career decision? Am J Surg. 2015;210:167–72. doi: 10.1016/j.amjsurg.2014.10.031. [DOI] [PubMed] [Google Scholar]
- 66.Kaderli R, Buser C, Stefenelli U, et al. Students’ interest in becoming a general surgeon before and after a surgical clerkship in German-speaking Switzerland. Swiss Med Wkly. 2011;141:w13246. doi: 10.4414/smw.2011.13246. [DOI] [PubMed] [Google Scholar]
- 67.Nwasor EO. Perception of final-year medical students about choice of anaesthesia as a specialty. Niger J Med. 2010;19 doi: 10.4314/njm.v19i2.56523. [DOI] [PubMed] [Google Scholar]
- 68.Zuccato JA, Kulkarni AV. The impact of early medical school surgical exposure on interest in neurosurgery. Can J Neurol Sci. 2016;43:410–6. doi: 10.1017/cjn.2015.332. [DOI] [PubMed] [Google Scholar]
- 69.Pignot G, Beley S, Larre S, et al. Prospective evaluation of the effects of a practical introduction to urology session on the recruitment of urology intern in Paris: final results. Prog Urol. 2007;17:240–4. doi: 10.1016/s1166-7087(07)92271-x. [DOI] [PubMed] [Google Scholar]
- 70.Cochran A, Paukert JL, Neumayer LA. Does a general surgery clerkship influence student perceptions of surgeons and surgical careers? Surgery. 2003;134:153–7. doi: 10.1067/msy.2003.216. [DOI] [PubMed] [Google Scholar]
- 71.Carter MB, Larson GM, Polk HC., Jr A brief private group practice rotation changes junior medical students’ perception of the surgical lifestyle. Am J Surg. 2005;189:458–61. doi: 10.1016/j.amjsurg.2004.09.019. [DOI] [PubMed] [Google Scholar]
- 72.Galiñanes EL, Shirshenkan JR, Doty J, et al. Standardized laparoscopic simulation positively affects a student’s surgical experience. J Surg Educ. 2013;70:508–13. doi: 10.1016/j.jsurg.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 73.Lee JT, Qiu M, Teshome M, et al. The utility of endovascular simulation to improve technical performance and stimulate continued interest of preclinical medical students in vascular surgery. J Surg Educ. 2009;66:367–73. doi: 10.1016/j.jsurg.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 74.Lee JT, Son JH, Chandra V, et al. Long-term impact of a preclinical endovascular skills course on medical student career choices. J Vasc Surg. 2011;54:1193–200. doi: 10.1016/j.jvs.2011.04.052. [DOI] [PubMed] [Google Scholar]
- 75.Madan AK, Frantzides CT, Quiros R, et al. Effects of a laparoscopic course on student interest in surgical residency. JSLS. 2005;9:134–7. [PMC free article] [PubMed] [Google Scholar]
- 76.Chin-Quee A, White L, Leeds I, et al. Medical student surgery elective in rural Haiti: a novel approach to satisfying clerkship requirements while providing surgical care to an underserved population. World J Surg. 2011;35:739–44. doi: 10.1007/s00268-011-0966-1. [DOI] [PubMed] [Google Scholar]
- 77.Hugar LA, McCullough CM, Quinn ME, et al. Scaling up short-term humanitarian surgery: a global surgery elective for senior medical students. J Surg Educ. 2014;71:871–7. doi: 10.1016/j.jsurg.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 78.Aziz SR, Ziccardi VB, Chuang S-K. Survey of residents who have participated in humanitarian medical missions. J Oral Maxillofac Surg. 2012;70:e147–57. doi: 10.1016/j.joms.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 79.Abedini NC, Danso-Bamfo S, Moyer CA, et al. Perceptions of Ghanaian medical students completing a clinical elective at the University of Michigan Medical School. Acad Med. 2014;89:1014–7. doi: 10.1097/ACM.0000000000000291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tahiri Y, Lee J, Kanevsky J, et al. The differing perceptions of plastic surgery between potential applicants and current trainees: the importance of clinical exposure and electives for medical students. Can J Plast Surg. 2013;21:178–80. doi: 10.1177/229255031302100307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Goltz CJ, Bachusz RC, Mancini E, et al. Medical student career survey — vascular surgery awareness initiative. Ann Vasc Surg. 2013;27:225–31. doi: 10.1016/j.avsg.2012.02.012. [DOI] [PubMed] [Google Scholar]
- 82.Boyd JS, Clyne B, Reinert SE, et al. Emergency medicine career choice: a profile of factors and influences from the Association of American Medical Colleges (AAMC) graduation questionnaires. Acad Emerg Med. 2009;16:544–9. doi: 10.1111/j.1553-2712.2009.00385.x. [DOI] [PubMed] [Google Scholar]
- 83.Pikoulis E, Avgerinos ED, Pedeli X, et al. Medical students’ perceptions on factors influencing a surgical career: the fate of general surgery in Greece. Surgery. 2010;148:510–5. doi: 10.1016/j.surg.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 84.Schwartz RW, Simpson WG, Strodel WE, et al. Career change: in quest of a controllable lifestyle. J Surg Res. 1989;47:189–92. doi: 10.1016/0022-4804(89)90105-4. [DOI] [PubMed] [Google Scholar]
- 85.Arnold MW, Patterson AF, Tang ASL. Has implementation of the 80-hour work week made a career in surgery more appealing to medical students? Am J Surg. 2005;189:129–33. doi: 10.1016/j.amjsurg.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 86.Valente J, Rappaport W, Neumayer L, et al. Influence of spousal opinions on residency selection. Am J Surg. 1992;163:596–8. doi: 10.1016/0002-9610(92)90565-9. [DOI] [PubMed] [Google Scholar]
- 87.Kao LS, Wilson EB, Anderson KD. Perceptions and predictors of surgeon satisfaction: a survey of spouses of academic surgeons. J Am Coll Surg. 2005;200:684–90. doi: 10.1016/j.jamcollsurg.2005.01.009. [DOI] [PubMed] [Google Scholar]
- 88.Zarebczan B, Rajamanickam V, Lewis B, et al. The impact of the 80-hour work week on student interest in a surgical career. J Surg Res. 2011;171:422–6. doi: 10.1016/j.jss.2010.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nuthalapaty FS, Jackson JR, Owen J. The influence of quality-of-life, academic, and workplace factors on residency program selection. Acad Med. 2004;79:417–25. doi: 10.1097/00001888-200405000-00010. [DOI] [PubMed] [Google Scholar]
- 90.Lee JT, Teshome M, de Virgilio C, et al. A survey of demographics, motivations, and backgrounds among applicants to the integrated 0 + 5 vascular surgery residency. J Vasc Surg. 2010;51:496–503. doi: 10.1016/j.jvs.2009.08.076. [DOI] [PubMed] [Google Scholar]
- 91.Cochran A, Melby S, Neumayer LA. An Internet-based survey of factors influencing medical student selection of a general surgery career. Am J Surg. 2005;189:742–6. doi: 10.1016/j.amjsurg.2005.03.019. [DOI] [PubMed] [Google Scholar]
- 92.Incorvaia AN, Ringley CD, Boysen DA. Factors influencing surgical career decisions. Curr Surg. 2005;62:429–35. doi: 10.1016/j.cursur.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 93.Avan BI, Raza SA, Hamza H, et al. Factors influencing the selection of surgical specialty among Pakistani medical graduates. J Postgrad Med. 2003;49:197–200. [PubMed] [Google Scholar]
- 94.Brandt MG, Wright ED. Medical student career choice and mental rotations ability. Clin Invest Med. 2005;28:112–7. [PubMed] [Google Scholar]
- 95.Fogarty CA, Bonebrake RG, Fleming AD, et al. Obstetrics and gynecology — To be or not to be? Factors influencing one’s decision. Am J Obstet Gynecol. 2003;189:652–4. doi: 10.1067/s0002-9378(03)00880-9. [DOI] [PubMed] [Google Scholar]
- 96.Thakur A, Fedorka P, Ko C, et al. Impact of mentor guidance in surgical career selection. J Pediatr Surg. 2001;36:1802–4. doi: 10.1053/jpsu.2001.28842. [DOI] [PubMed] [Google Scholar]
- 97.Erzurum VZ, Obermeyer RJ, Fecher A, et al. What influences medical students’ choice of surgical careers. Surgery. 2000;128:253–6. doi: 10.1067/msy.2000.108214. [DOI] [PubMed] [Google Scholar]
- 98.Boyle E, Healy D, Hill ADK, et al. Career choices of today’s medical students: Where does surgery rank? Ir J Med Sci. 2012;182:337–43. doi: 10.1007/s11845-012-0882-x. [DOI] [PubMed] [Google Scholar]
- 99.Freed GL, Dunham KM, Jones MD, et al. General pediatrics resident perspectives on training decisions and career choice. Pediatrics. 2009;123:S26–30. doi: 10.1542/peds.2008-1578H. [DOI] [PubMed] [Google Scholar]
- 100.Scott IM, Matejcek AN, Gowans MC, et al. Choosing a career in surgery: factors that influence Canadian medical students’ interest in pursuing a surgical career. Can J Surg. 2008;51:371–7. [PMC free article] [PubMed] [Google Scholar]
- 101.Harris MG, Gavel PH, Young JR. Factors influencing the choice of specialty of Australian medical graduates. Med J Aust. 2005;183:295–300. doi: 10.5694/j.1326-5377.2005.tb07058.x. [DOI] [PubMed] [Google Scholar]
- 102.Lawal TA, Afolabi AO. Factors influencing the choice of surgery as a career by pre-registration interns. Afr Health Sci. 2013;13:814–9. doi: 10.4314/ahs.v13i3.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.McHugh S, Corrigan M, Sheikh A, et al. Factors influencing career choice after initial training in surgery. World J Surg. 2011;35:487–92. doi: 10.1007/s00268-010-0934-1. [DOI] [PubMed] [Google Scholar]
- 104.Miller G, Bamboat ZM, Allen F, et al. Impact of mandatory resident work hour limitations on medical students’ interest in surgery. J Am Coll Surg. 2004;199:615–9. doi: 10.1016/j.jamcollsurg.2004.05.275. [DOI] [PubMed] [Google Scholar]
- 105.Montgomery SC, Privette AR, Ferguson PL, et al. Inadequately marketing our brand: medical student awareness of acute care surgery. J Trauma Acute Care Surg. 2015;79:858–64. doi: 10.1097/TA.0000000000000851. [DOI] [PubMed] [Google Scholar]
- 106.Quillin RC, III, Pritts TA, Davis BR, et al. Surgeons underestimate their influence on medical students entering surgery. J Surg Res. 2012;177:201–6. doi: 10.1016/j.jss.2012.05.064. [DOI] [PubMed] [Google Scholar]
- 107.McCaffrey JC. Medical student selection of otolaryngology-head and neck surgery as a specialty: influences and attitudes. Otolaryngol Head Neck Surg. 2005;133:825–30. doi: 10.1016/j.otohns.2005.07.042. [DOI] [PubMed] [Google Scholar]
- 108.Klingensmith ME, Cogbill TH, Luchette F, et al. Factors influencing the decision of surgery residency graduates to pursue general surgery practice versus fellowship. Ann Surg. 2015;262:449–55. doi: 10.1097/SLA.0000000000001435. [DOI] [PubMed] [Google Scholar]
- 109.Brandt MG, Scott GM, Doyle PC, et al. Otolaryngology-head and neck surgeon unemployment in Canada: a cross-sectional survey of graduating otolaryngology-head and neck surgery residents. J Otolaryngol Head Neck Surg. 2014;43:37. doi: 10.1186/s40463-014-0037-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Reid CM, Kim DY, Mandel J, et al. Impact of a third-year surgical apprenticeship model: perceptions and attitudes compared with the traditional medical student clerkship experience. J Am Coll Surg. 2014;218:1032–7. doi: 10.1016/j.jamcollsurg.2014.01.047. [DOI] [PubMed] [Google Scholar]
- 111.Yazigi A, Nasr M, Sleilaty G, et al. Clinical teachers as role models: perceptions of interns and residents in a Lebanese medical school. Med Educ. 2006;40:654–61. doi: 10.1111/j.1365-2929.2006.02502.x. [DOI] [PubMed] [Google Scholar]
- 112.Berman L, Rosenthal MS, Curry LA, et al. Attracting surgical clerks to surgical careers: role models, mentoring, and engagement in the operating room. J Am Coll Surg. 2008;207:793–800.e2. doi: 10.1016/j.jamcollsurg.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 113.McCord JH, McDonald R, Sippel RS, et al. Surgical career choices: the vital impact of mentoring. J Surg Res. 2009;155:136–41. doi: 10.1016/j.jss.2008.06.048. [DOI] [PubMed] [Google Scholar]
- 114.Nguyen SQ, Divino CM. Surgical residents as medical student mentors. Am J Surg. 2007;193:90–3. doi: 10.1016/j.amjsurg.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 115.Whittaker LD, Jr, Estes NC, Ash J, et al. The value of resident teaching to improve student perceptions of surgery clerkships and surgical career choices. Am J Surg. 2006;191:320–4. doi: 10.1016/j.amjsurg.2005.10.029. [DOI] [PubMed] [Google Scholar]
- 116.Abioye IA, Ibrahim NA, Odesanya MO, et al. The future of trauma care in a developing country: interest of medical students and interns in surgery and surgical specialties. Int J Surg. 2012;10:209–12. doi: 10.1016/j.ijsu.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 117.Hernandez J, Al-Saadi S, Boyle R, et al. Surgeons can favorably influence career choices and goals for students interested in careers in medicine. J Am Coll Surg. 2009;209:62–7. doi: 10.1016/j.jamcollsurg.2009.02.065. [DOI] [PubMed] [Google Scholar]
- 118.Kaderli RM, Klasen JM, Businger AP. Mentoring in general surgery in Switzerland. Med Educ Online. 2015;20:27528. doi: 10.3402/meo.v20.27528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kahn SA, Goldman M, Daul M, et al. The burn surgeon: an endangered species. Can exposure in medical school increase interest in burn surgery? J Burn Care Res. 2011;32:39–45. doi: 10.1097/BCR.0b013e318204b318. [DOI] [PubMed] [Google Scholar]
- 120.Kollias C, Banza L, Mkandawire N. Factors involved in selection of a career in surgery and orthopedics for medical students in Malawi. Malawi Med J. 2010;22:20–3. doi: 10.4314/mmj.v22i1.55904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Bell RM, Fann SA, Morrison JE, et al. Determining personal talents and behavioral styles of applicants to surgical training: a new look at an old problem, part II. J Surg Educ. 2012;69:23–9. doi: 10.1016/j.jsurg.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 122.Preece RA, Cope AC. Are surgeons born or made? A comparison of personality traits and learning styles between surgical trainees and medical students. J Surg Educ. 2016;73:768–73. doi: 10.1016/j.jsurg.2016.03.017. [DOI] [PubMed] [Google Scholar]
- 123.Drosdeck JM, Osayi SN, Peterson LA, et al. Surgeon and non-surgeon personalities at different career points. J Surg Res. 2015;196:60–6. doi: 10.1016/j.jss.2015.02.021. [DOI] [PubMed] [Google Scholar]
- 124.Martinou E, Allan H, Vig S. Personality differences among junior postgraduate trainees in the United Kingdom. J Surg Educ. 2015;72:122–7. doi: 10.1016/j.jsurg.2014.06.014. [DOI] [PubMed] [Google Scholar]
- 125.Eng MKH, Macneily AE, Alden L. The urological personality: Is it unique? Can J Urol. 2004;11:2401–6. [PubMed] [Google Scholar]
- 126.McGreevy J, Wiebe D. A preliminary measurement of the surgical personality. Am J Surg. 2002;184:121–5. doi: 10.1016/s0002-9610(02)00919-4. [DOI] [PubMed] [Google Scholar]
- 127.Borges NJ, Stratton TD, Wagner PJ, et al. Emotional intelligence and medical specialty choice: findings from three empirical studies. Med Educ. 2009;43:565–72. doi: 10.1111/j.1365-2923.2009.03371.x. [DOI] [PubMed] [Google Scholar]
- 128.Sallee DS, Cooper C, Ravin CE. Medical student perceptions of diagnostic radiology. Influence of a senior radiology elective. Invest Radiol. 1989;24:724–8. doi: 10.1097/00004424-198909000-00015. [DOI] [PubMed] [Google Scholar]
- 129.Skrzypek M, Turska D. [Personality of medical students declaring surgical specialty choice in the context of prospective medical practice style]. Przegl Lek. 2015;72:295–301. [PubMed] [Google Scholar]
- 130.Kiker BF, Zeh M. Relative income expectations, expected malpractice premium costs, and other determinants of physician specialty choice. J Health Soc Behav. 1998;39:152. [PubMed] [Google Scholar]
- 131.Azizzadeh A, McCollum CH, Miller CC, III, et al. Factors influencing career choice among medical students interested in surgery. Curr Surg. 2003;60:210–3. doi: 10.1016/S0149-7944(02)00679-7. [DOI] [PubMed] [Google Scholar]
- 132.Association of Women Surgeons. Association of Women Surgeons statement on gender salary equity. Chicago (IL): AOWS; 2017. [accessed 2017 May 1]. Available: www.womensurgeons.org/2017-statement-on-gender-salaryequity/ [Google Scholar]
- 133.Balch CM, Freischlag JA, Shanafelt TD. Stress and burnout among surgeons: understanding and managing the syndrome and avoiding the adverse consequences. Arch Surg. 2009;144:371–6. doi: 10.1001/archsurg.2008.575. [DOI] [PubMed] [Google Scholar]
- 134.Khoushhal Z, Hussain MA, Greco E, et al. Prevalence and causes of attrition among surgical residents. JAMA Surg. 2017;152:265–72. doi: 10.1001/jamasurg.2016.4086. [DOI] [PubMed] [Google Scholar]
- 135.Bilimoria KY, Chung JW, Hedges LV, et al. National cluster-randomized trial of duty-hour flexibility in surgical training. N Engl J Med. 2016;374:713–27. doi: 10.1056/NEJMoa1515724. [DOI] [PubMed] [Google Scholar]
- 136.Royal College of Physicians and Surgeons of Canada. Competence by Design. Ottawa (ON): RCPSC; 2017. [accessed 2017 July 26]. Available: www.royalcollege.ca/rcsite/cbd/rationale-why-cbd-e. [Google Scholar]
- 137.Nellis JC, Eisele DW, Francis HW, et al. Impact of a mentored student clerkship on underrepresented minority diversity in otolaryngology-head and neck surgery. Laryngoscope. 2016;126:2684–8. doi: 10.1002/lary.25992. [DOI] [PubMed] [Google Scholar]
- 138.Hill E, Bowman K, Stalmeijer R, et al. You’ve got to know the rules to play the game: how medical students negotiate the hidden curriculum of surgical careers. Med Educ. 2014;48:884–94. doi: 10.1111/medu.12488. [DOI] [PubMed] [Google Scholar]