Abstract
Background:
Patellar height has long been considered a risk factor for patellofemoral instability. However, recent pediatric literature demonstrated a reduction in patellar height measurements following medial patellofemoral ligament (MPFL) reconstruction.
Purpose:
To assess the mean change in patellar height and the percentage of skeletally mature patients with patellar height ratios reduced to within-normal limits following MPFL reconstruction.
Study Design:
Case series; Level of evidence, 4.
Methods:
Adult patients undergoing primary MPFL reconstruction for recurrent lateral patellar instability between 2005 and 2013 were identified. Pre- and postoperative (within 1 year of surgery) lateral knee radiographs were assessed for patellar height indices, including Caton-Deschamps, Blackburne-Peel, and Insall-Salvati ratios. The change in patellar height and the number of patients reduced from abnormal to normal patellar height ratios following MPFL reconstruction were assessed.
Results:
Overall, 32 adult patients were included in the study, with a mean age of 25.7 years (range, 18-55 years). There were 21 women (66%) and 11 men (34%). Insall-Salvati, Blackburne-Peel, and Caton-Deschamps ratios all demonstrated significant reductions in patellar height between pre- and postoperative lateral knee radiographs (P < .001). All 3 indices showed a reduction in the number of patients meeting the criteria for patella alta following MPFL reconstruction. A total of 64% of patients had an abnormal preoperative Caton-Deschamps ratio reduced to within normal limits postoperatively.
Conclusion:
MPFL reconstruction provides a consistent reduction in patellar height measurements. The Caton-Deschamps ratio was reduced to the reference range following MPFL reconstruction in 64% of patients with preoperative patella alta. Surgeons treating patellofemoral instability should expect a reduction in patellar height after ligament reconstruction, which may affect the need for more invasive distalization procedures.
Keywords: patellar instability, MPFL reconstruction, patellar height, patellofemoral arthritis
Lateral patellar dislocation is common in young athletes, with a per capita risk of 30 per 100,000.6 According to MacNab,11 15% of patients redislocate their patella, while an additional 18% experience symptoms. The etiology of recurrent patellar dislocation is multifactorial and may be secondary to recurrent trauma. Many patients also demonstrate predisposing factors, such as trochlear dysplasia, limb malalignment, and patella alta, which directly affect the biomechanics of the patellofemoral articulation.3,15,19
Patella alta is present in 48% of patients with recurrent patellofemoral instability (RPFI), as opposed to only 12% of controls.13 Biomechanically, patella alta results in decreased contact forces between the patella and the trochlea.9 Mayer et al12 performed distalization of the tibial tubercle with patellar tendon tenodesis for patients with RPFI and patella alta and reported no episodes of redislocation in 27 knees at 5-year follow-up. However, the indications for such invasive procedures remain unclear, and there is a risk for iatrogenic patella baja.15
The medial patellofemoral ligament (MPFL) provides 60% of the total medial restraining force at 20° of knee flexion.4 In addition to medial restraint, recent literature in the pediatric population has indicated that MPFL reconstruction may have a distalization effect on the patella.5 Lykissas et al10 assessed the pre- and postoperative radiographs of 38 pediatric patients who underwent MPFL reconstruction. The authors showed that the Insall-Salvati, Blackburne-Peel, and Caton-Deschamps ratios were all significantly reduced following MPFL reconstruction. However, the femoral insertion for open physeal MPFL reconstruction was located approximately 4 mm distal to the physis in a nonanatomic position.5 This orientation created an increased MPFL angle of obliquity, thereby increasing the inferior force vector. Schöttle et al16 demonstrated that adults with preoperative patella alta can correct to normal after MPFL reconstruction. However, over half of patients had undergone a tibial tubercle osteotomy, making it difficult to determine if the correction in patellar height was the result of MPFL reconstruction or corrective osteotomy.
The objective of this study was to retrospectively review the effect of isolated anatomic MPFL reconstruction on patellar height in an adult patient population. We aimed to determine the absolute change in patellar height ratios and the percentage of patients whose patellar height is reduced to within the reference range.
Methods
After approval by our institutional review board (No. 08-001342), all patients with a history of primary MPFL reconstruction at our institution from 2005 to 2013 were identified in a surgical database with Current Procedural Terminology and International Classification of Diseases codes. Patients were included if they (1) underwent primary MPFL reconstruction at our institution for recurrent patellar instability after failed nonoperative treatment, (2) had pre- and postoperative lateral knee radiographs within 1 year of surgery, and (3) were ≥18 years old at surgery. Patients were excluded if they had (1) concomitant cruciate ligament reconstruction, (2) multiligament knee injury, (3) no lateral knee radiographs, (4) tibial tubercle–trochlear groove (TT-TG) measurement >20 mm,3 and (5) moderate trochlear dysplasia (Dejour type C or greater)3,15 and were (6) <18 years old at the time of surgery. A total of 32 patients satisfied these criteria and were included in the study.
Chart review was performed to verify patient information (age, sex, surgical characteristics) and pre- and postoperative lateral knee radiographs. All lateral radiographs were performed with the knee positioned in 20° to 30° of flexion and the epicondyles perpendicular to the image receptor. Lateral radiographs were assessed for patellar height with the Caton-Deschamps,2 Blackburne-Peel,1 and Insall-Salvati ratios.7 Two authors (J.M.W. and R.A.C.—an orthopedic sports fellow and a chief resident, respectively) calculated these ratios to ensure interrater reliability (Figure 1). Means of the measures between the 2 observers were calculated and used to compare pre- and postoperative patellar height. Mean values of patellar height in the cohort were compared with values reported in the literature as normal.1,2,7 Femoral tunnel location was plotted in relation to Schöttle’s point17 on a true lateral femoral radiograph. A position within 7 mm of this point was considered anatomic as described by Servien et al.18
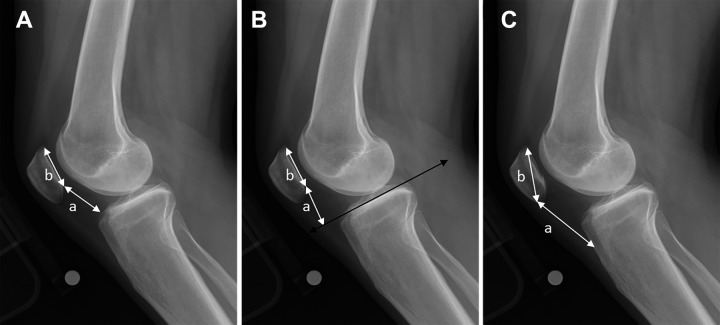
Figure 1.
Radiographic patellar height indices, each measured as a ÷ b. (A) Caton-Deschamps ratio, with line a demonstrating the distance between the distal end of the patellar articular surface to the anterosuperior angle of the tibia and line b demonstrating the length of the articular surface of the patella. (B) Blackburne-Peel ratio, with line a being perpendicular to the tibial plateau line and line b measuring the length of the articular surface of the patella. (C) Insall-Salvati ratio, with line a representing the length of the patellar tendon and line b demonstrating the maximum length of the patella.
Surgical Technique
Isolated MPFL reconstruction was performed at a single institution by 1 of 3 senior authors (A.J.K., D.L.D., M.J.S.) on patients with a clinical history of RPFI and a positive apprehension test result. Diagnostic arthroscopy was performed in all cases, with grading of the cartilage status of both the undersurface of the patella and the femoral trochlea. Mechanical chondroplasty of unstable cartilage was performed when indicated.
After diagnostic arthroscopy, the graft (11 semitendinosus autografts, 2 quadriceps tendon autografts, 11 gracilis autografts, and 8 gracilis allografts) was prepared with a running whipstitch placed in both free ends. A 4-cm incision was made over the medial aspect of the patella. Sharp dissection was carried down to the medial retinacular layer, where the interval between medial layer 2 (retinaculum) and medial layer 3 (capsule) was then defined for graft passage. A small shallow trough was then created in the superomedial aspect of the patella, in the area of the native MPFL origin. The graft was then secured to the patella with two 2.8-mm FASTak suture anchors (Arthrex) or two 3.5-mm biocomposite SwiveLock anchors (Arthrex), spaced 1 cm apart. The femoral insertion point was identified by fluoroscopy, according to the method described by Schöttle et al.17 An incision was made at this designated point, and sharp dissection was performed down to the medial aspect of the distal medial femoral condyle. The graft was then looped to create a double-bundle construct, and the free ends were passed from the patella to the femur. The graft was placed around the femoral guide wire as the knee was brought through an arc of motion to test for relative graft isometry from 0° to 90°. The diameter of the doubled graft determined the diameter of the tunnel that was drilled; typically, a 6-mm socket was made by advancing a cannulated drill over the guide wire to a depth of 30 mm. With the knee held in 30° of flexion, a 6 × 23–mm bioabsorbable interference screw (Arthrex) was then used to secure the 6-mm graft in the femoral socket. A layered closure was then performed, sterile dressings applied, and a knee immobilizer initially provided.
Postoperative Rehabilitation
Postoperative rehabilitation consisted of a knee immobilizer for 2 weeks and partial weightbearing with crutches for 6 weeks. Range-of-motion exercises were performed immediately and without restriction. Full weightbearing, full knee range of motion, and progressive strength and proprioceptive training were allowed after 6 weeks.
Statistical Analysis
The interclass correlation coefficient was used to quantify interrater reliability for each measure of patellar height. Adequate correlation was accepted as an interclass correlation coefficient >0.5; good, >0.7; and excellent, >0.8. Paired Student t tests were used to evaluate for postoperative changes in each continuous measure of patellar height. The McNemar test for paired categorical data was used to compare the number of patients with patella alta pre- versus postoperatively. All statistical analyses were performed with SAS Statistical Discovery JMP (v 7.0; SAS Inc). Differences in the means of the groups preoperatively and at final follow-up were evaluated, and significance was determined with an alpha level of 0.05.
Results
For the 32 skeletally mature patients included in the study, the mean age was 25.7 years (range, 18-55 years), and there were 21 women (66%) and 11 men (34%). The right knee was involved in 15 patients and the left in 17 patients. Radiographs were obtained at a mean 149 days before surgery and 119 days after surgery, with a mean 268 days between pre- and postoperative radiographs.
Interrater reliability was good for Caton-Deschamps and Blackburne-Peel (0.73 and 0.70, respectively) and excellent for Insall-Salvati (0.86). The mean pre- and postoperative patellar height measurements with the Insall-Salvati, Blackburne-Peel, and Caton-Deschamps ratios are listed in Table 1. All 3 ratios demonstrated a statistically significant reduction in patellar height following MPFL reconstruction. The number of patients with abnormal values for all 3 measures (patella alta) decreased after surgery: Insall-Salvati ratio (abnormal >1.2), 24 patients (75.0%) preoperatively versus 22 (68.8%) postoperatively (P = .5); Blackburne-Peel ratio (abnormal >1.0), 13 patients (40.6%) preoperatively versus only 8 patients (25%) postoperatively (P = .09); Caton-Deschamps ratio (abnormal >1.2), 11 patients (34.4%) preoperatively versus only 4 patients (12.5%) postoperatively (P = .0082). The Caton-Deschamps ratio had the greatest percentage of patients with preoperative patella alta that decreased to within the reference range (7 of 11, 64%) following MPFL reconstruction.
TABLE 1.
Means and Changes in Patellar Height Indices Pre- and Postoperatively
| Index, Mean ± SD | ||||
|---|---|---|---|---|
| Ratio | Preoperatively | Postoperatively | Mean Absolute Improvement | P Value |
| Insall-Salvati | 1.37 ± 0.2 | 1.33 ± 0.2 | 0.04 | .0005 |
| Blackburne-Peel | 1.0 ± 0.2 | 0.92 ± 0.1 | 0.08 | <.0001 |
| Caton-Deschamps | 1.13 ± 0.2 | 1.04 ± 0.1 | 0.09 | .0003 |
Discussion
Abnormal patellar height has long been considered a risk factor for patellofemoral instability, with approximately half of patients meeting the criteria for patella alta.13,19 However, the majority of the patients (70%) in the current study only marginally exceeded reference values. Furthermore, recent pediatric literature has demonstrated that radiographic patellar height measurements are decreased following MPFL reconstruction5,10 This information has raised speculation that in many cases patella alta may result from the MPFL tear as opposed to being a risk factor for patellofemoral instability.5
The MPFL is an obliquely oriented structure, with 15.9° of inferior angulation.14 Therefore, it is not surprising that the MPFL affects inferior and medial patellar translation. The influence of MPFL reconstruction on radiographic measures of patella alta was assessed in 2 previous publications.5,10 Lykissas et al10 performed single patellar and femoral tunnel gracilis tendon MPFL reconstructions. Thirty-four patients were assessed for Insall-Salvati and Caton-Deschamps ratios, and significant reductions were identified postoperatively. Fabricant et al5 supported these findings with the use of a dual patellar insertion semitendinosus tendon reconstruction technique. However, the participants in both these studies were pediatric patients with nonanatomic MPFL graft placement on the femur. LaPrade et al8 identified the anatomic MPFL femoral insertion site as being located 1.9 mm anterior and 3.8 mm distal to the adductor tubercle. This anatomic location is proximal to the femoral physis; however, the MPFL graft in a patient with open physes is commonly placed into the epiphysis approximately 5 mm distal to the physis.5 If the femoral graft is placed in the more proximal anatomic position in a skeletally immature patient, patella alta can theoretically result as the femoral physis grows distally.
The current study reviewed 32 skeletally mature patients who underwent MPFL reconstruction with Schöttle’s radiographic point for anatomic femoral insertion.17 Radiographic assessment for patella alta, including Insall-Salvati, Blackburne-Peel, and Caton-Deschamps ratios, demonstrated significantly reduced values following MPFL reconstruction. The mean differences between pre- and postoperative patellar height measurements were 0.04, 0.08, and 0.09 for Insall-Salvati, Blackburne-Peel, and Caton-Deschamps, respectively. Using the Caton-Deschamps ratio, 34% of patients (11 of 32) met the criteria for patella alta (>1.2) preoperatively, as compared with 12.5% (4 of 32) after MPFL reconstruction. This represented a 64% (7 of 11) correction to the reference range. Despite these significant changes in patellar height measurements, the mean differences in the current study were lower than those previously reported for pediatric patients5,10 (Table 2). This may be attributable to the location of the femoral tunnel in adult patients. The natural obliquity between the femoral origin and patellar insertion of the MPFL is 15.9° from horizontal. When the femoral tunnel is placed in a nonanatomic position distal to the physis in pediatric patients, this obliquity is increased. Schöttle et al16 showed that preoperative measures of patella alta among some adult patients reduced to the normal range postoperatively (as measured by Caton-Deschamps ratio). However, in this study of 15 patients, 8 underwent tibial tubercle osteotomy for TT-TG measurements >15 mm, making it difficult to determine the isolated influence of MPFL reconstruction or corrective osteotomy on patellar height.
TABLE 2.
Comparison of Mean Change in Patellar Height Indices After MPFL Reconstruction Between Current and Previous Studiesa
| Mean Difference | |||
|---|---|---|---|
| Study | Insall- Salvati | Caton- Deschamps | Blackburne- Peel |
| Current study | –0.04 | –0.09 | –0.08 |
| Lykissas et al10 | –0.11 | –0.14 | –0.12 |
| Fabricant et al5 | –0.16 | –0.22 | N/A |
aAll mean differences were statistically significant, P < .05. N/A, not applicable.
The current study supports the theory that patellar dislocation with disruption of the MPFL contributes to patella alta. MPFL reconstruction predictably reduces patellar height according to 3 radiographic measurements. Although the specific criteria for adding a tubercle distalization procedure in the presence of patella alta remains unclear, we recommend that current thresholds for distalization be re-examined, since preoperative measures of patella alta can correct to normal following MPFL reconstruction. Further research to determine the association between postoperative patellar height measurements and recurrent dislocation is needed to better define this threshold.
Limitations
The results reported in this study should be interpreted with the following limitations in mind. First, the retrospective nature of the study inherently creates patient selection bias. Second, only postinjury and postoperative images were available for review; therefore, it was not possible to determine patellar height preinjury. Third, the timing of radiographs varied significantly in relation to their surgical dates, namely because the 3 senior authors performing the procedures do not routinely reimage preoperatively after the initial consultation unless there is concern for a new injury, to reduce radiation exposure. While all patients underwent intraoperative fluoroscopic imaging, these images were not utilized in this study, as they lacked standardization of knee position and flexion angle. Fourth, despite the use of intraoperative fluoroscopic imaging, there was still some variability in graft position within the study cohort. However, an overall distalizing vector was not appreciated (Figure 2). Fifth, the difference in radiographic measurements between pre- and postoperative images may be partially explained by quadriceps inhibition. Although it can be reasoned that quadriceps strength could influence patellar height, we are not aware of any literature supporting this theory. Last, clinical outcomes were not provided; therefore, we were unable to determine whether the mean changes in patellar height observed following MPFL reconstruction represent clinically significant changes. Despite these limitations, this is the first series to report the influence of MPFL reconstruction on patellar height in skeletally mature patients. Results demonstrated a small but consistent reduction in patellar height measurements following MPFL reconstruction. This is important information for surgeons treating RPFI, as it may reduce the rate of invasive distalization procedures among patients with abnormal patellar height measurements.
Figure 2.
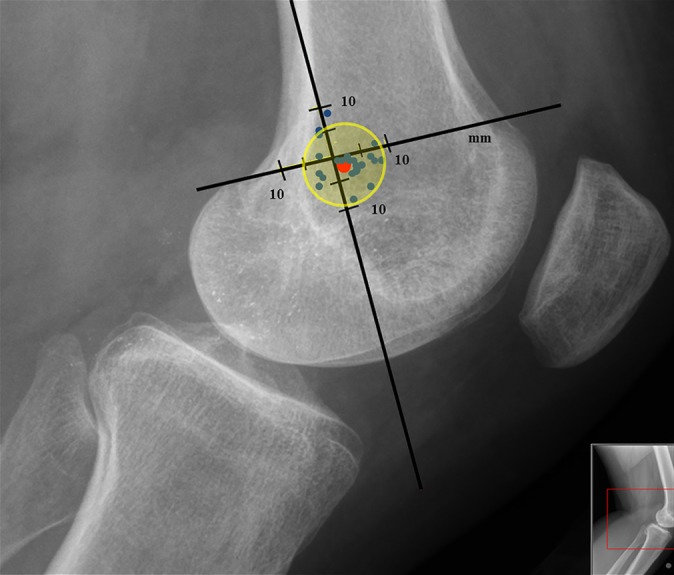
Positioning of femoral screw in current cohort in reference to Schöttle's point (red).
Conclusion
MPFL reconstruction in adult patients provides a consistent reduction in patellar height measurements. After MPFL reconstruction, the Caton-Deschamps ratio was reduced to the reference range in 64% of patients with preoperative patella alta (Caton-Deschamps >1.2). Surgeons treating patellofemoral instability should expect a reduction in patellar height after ligament reconstruction, which may affect the need for more invasive distalization procedures.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: M.J.S. is a paid consultant for Arthrex, receives royalties from Arthrex, and receives research support from Stryker. A.J.K. is a paid consultant for Arthrex and receives research support from the Arthritis Foundation and Histogenics. D.L.D. has stock/stock options in Tenex Heath, and her spouse receives royalties from Tenex Health.
Ethical approval for this study was obtained from the Mayo Clinic Institutional Review Board (No. 08-001342).
References
- 1. Blackburne JS, Peel TE. A new method of measuring patellar height. J Bone Joint Surg Br. 1977;59(2):241–242. [DOI] [PubMed] [Google Scholar]
- 2. Caton J, Deschamps G, Chambat P, Lerat JL, Dejour H. Patella infera: apropos of 128 cases [in French]. Rev Chir Orthop Reparatrice Appar Mot. 1982;68(5):317–325. [PubMed] [Google Scholar]
- 3. Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19–26. [DOI] [PubMed] [Google Scholar]
- 4. Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26(1):59–65. [DOI] [PubMed] [Google Scholar]
- 5. Fabricant PD, Ladenhauf HN, Salvati EA, Green DW. Medial patellofemoral ligament (MPFL) reconstruction improves radiographic measures of patella alta in children. Knee. 2014;21(6):1180–1184. [DOI] [PubMed] [Google Scholar]
- 6. Fithian DC, Paxton EW, Post WR, Panni AS; International Patellofemoral Study Group. Lateral retinacular release: a survey of the International Patellofemoral Study Group. Arthroscopy. 2004;20(5):463–468. [DOI] [PubMed] [Google Scholar]
- 7. Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101(1):101–104. [DOI] [PubMed] [Google Scholar]
- 8. LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am. 2007;89(9):2000–2010. [DOI] [PubMed] [Google Scholar]
- 9. Luyckx VA, Cairo LV, Compston CA, Phan WL, Mueller TF. Oncostatin M pathway plays a major role in the renal acute phase response. Am J Physiol Renal Physiol. 2009;296(4):F875–F883. [DOI] [PubMed] [Google Scholar]
- 10. Lykissas MG, Li T, Eismann EA, Parikh SN. Does medial patellofemoral ligament reconstruction decrease patellar height? A preliminary report. J Pediatr Orthop. 2014;34(1):78–85. [DOI] [PubMed] [Google Scholar]
- 11. MacNab I. Recurrent dislocation of the patella. J Bone Joint Surg Am. 1952;34A(4):957–967. [PubMed] [Google Scholar]
- 12. Mayer C, Magnussen RA, Servien E, et al. Patellar tendon tenodesis in association with tibial tubercle distalization for the treatment of episodic patellar dislocation with patella alta. Am J Sports Med. 2012;40(2):346–351. [DOI] [PubMed] [Google Scholar]
- 13. Neyret P, Robinson AH, Le Coultre B, Lapra C, Chambat P. Patellar tendon length—the factor in patellar instability? Knee. 2002;9(1):3–6. [DOI] [PubMed] [Google Scholar]
- 14. Nomura E, Inoue M, Osada N. Anatomical analysis of the medial patellofemoral ligament of the knee, especially the femoral attachment. Knee Surg Sports Traumatol Arthrosc. 2005;13(7):510–515. [DOI] [PubMed] [Google Scholar]
- 15. Sanchis-Alfonso V. Guidelines for medial patellofemoral ligament reconstruction in chronic lateral patellar instability. J Am Acad Orthop Surg. 2014;22(3):175–182. [DOI] [PubMed] [Google Scholar]
- 16. Schöttle PB, Fucentese SF, Romero J. Clinical and radiological outcome of medial patellofemoral ligament reconstruction with a semitendinosus autograft for patella instability. Knee Surg Sports Traumatol Arthrosc. 2005;13(7):516–521. [DOI] [PubMed] [Google Scholar]
- 17. Schöttle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(5):801–804. [DOI] [PubMed] [Google Scholar]
- 18. Servien E, Fritsch B, Lustig S, et al. In vivo positioning analysis of medial patellofemoral ligament reconstruction. Am J Sports Med. 2011;39(1):134–139. [DOI] [PubMed] [Google Scholar]
- 19. Wagner D, Pfalzer F, Hingelbaum S, Huth J, Mauch F, Bauer G. The influence of risk factors on clinical outcomes following anatomical medial patellofemoral ligament (MPFL) reconstruction using the gracilis tendon. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):318–324. [DOI] [PubMed] [Google Scholar]